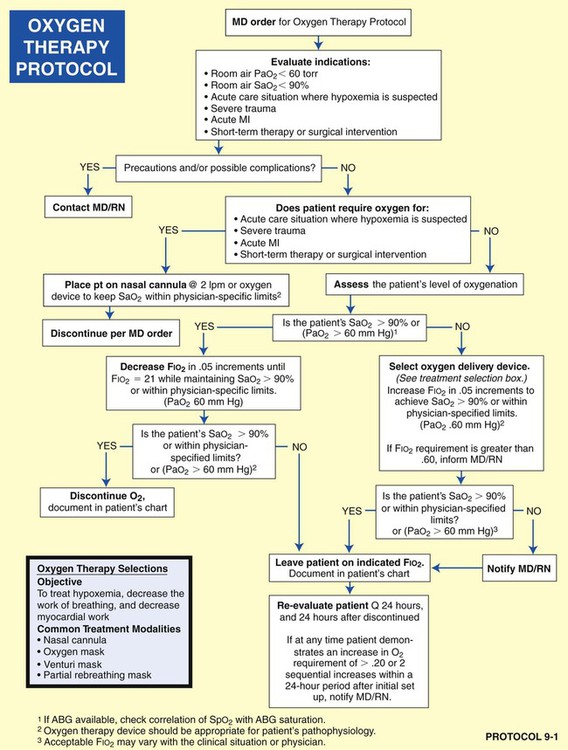
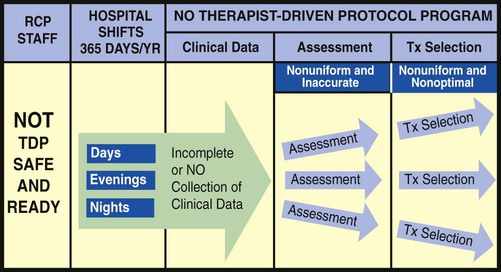
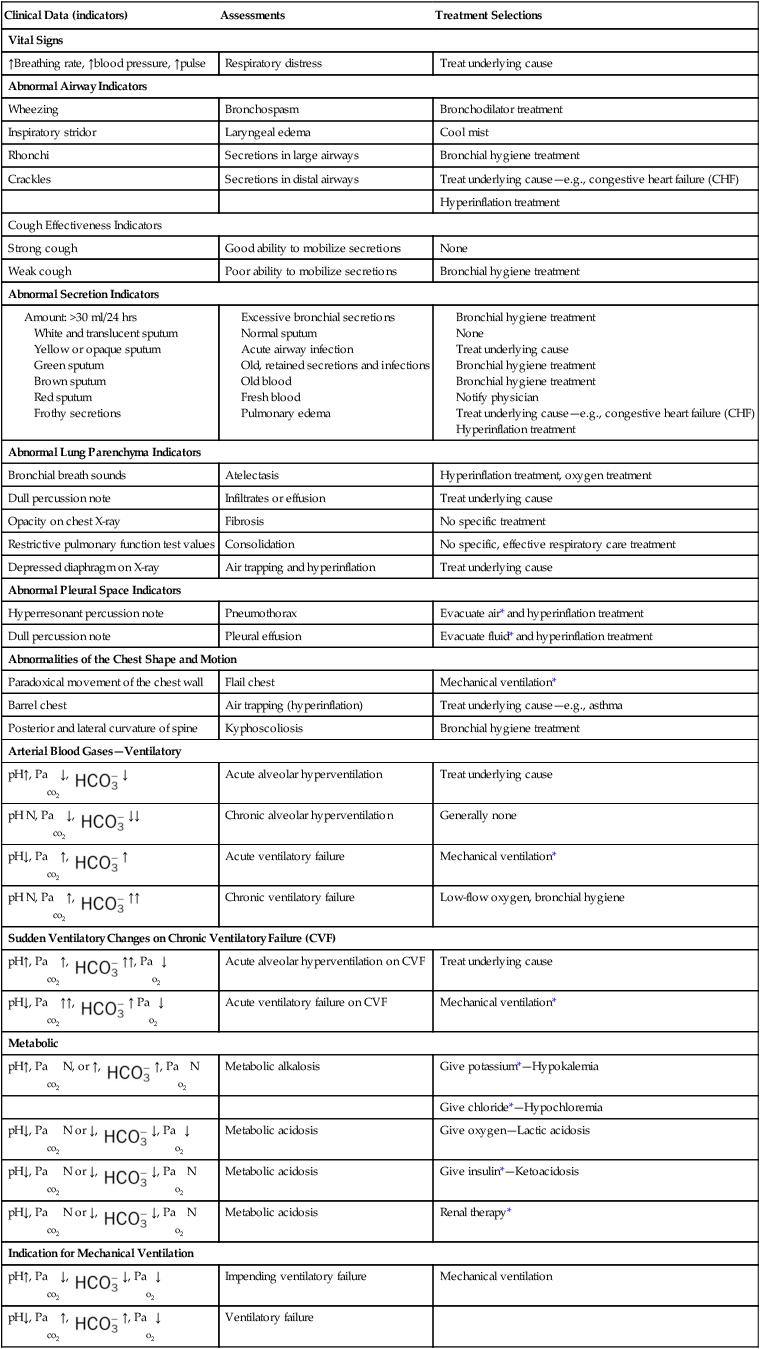
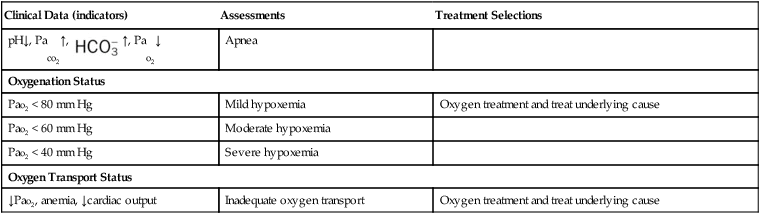
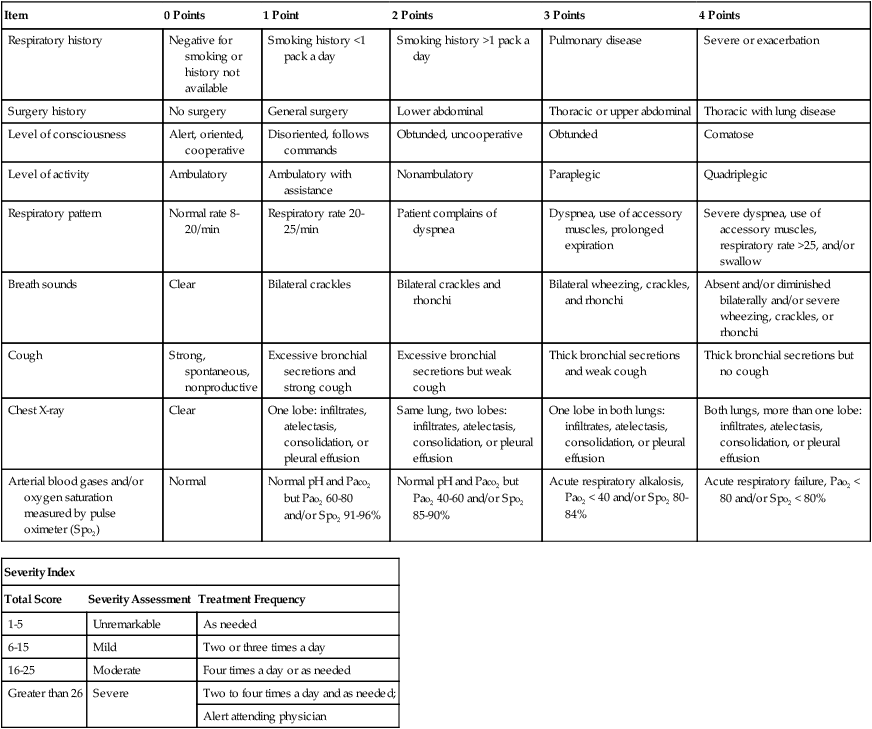
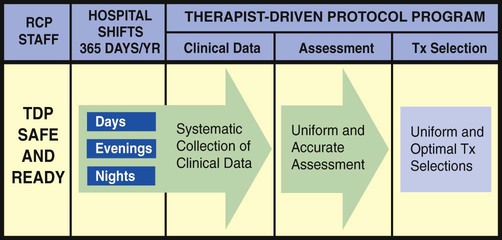
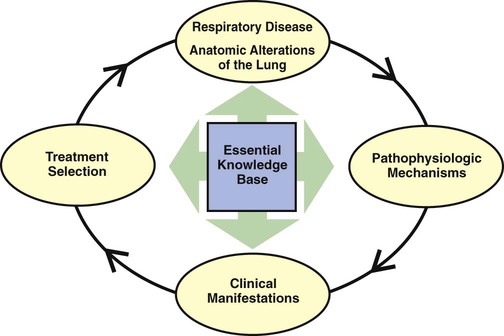
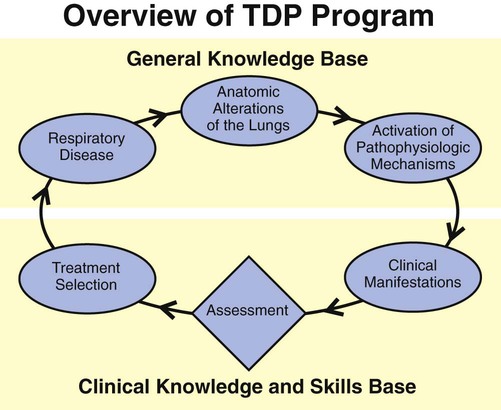
After reading this chapter, you will be able to: • Describe the Therapist-Driven Protocol (TDP) program and the role of the respiratory care practitioner. • Discuss the knowledge base required for a successful TDP program. • Explain the assessment process skills required for a successful TDP program, and include the following: • The clinical manifestations, assessments, and treatment selections made by the respiratory care practitioner • The frequency at which a respiratory therapy modality can be determined in response to a severity assessment • Describe the following essential cornerstone respiratory protocols for a successful TDP program: • Bronchopulmonary hygiene therapy protocol • Lung expansion therapy protocol • Aerosolized medication therapy protocol • Mechanical ventilation protocol • Mechanical ventilation weaning protocol • Describe ventilatory management in catastrophes. • List the following common anatomic alterations of the lungs: • Increased alveolar-capillary membrane thickness • Excessive bronchial secretions • Distal airway and alveolar weakening • Analyze the clinical scenarios—chain of events—activated by the common anatomic alterations of the lungs, and include the following: • Anatomic alterations of the lungs • Pathophysiologic mechanisms activated • Treatment protocols used to correct the problem • Identify the most common anatomic alterations associated with the respiratory disorders presented in this textbook. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. • Deliver individualized diagnostic and therapeutic respiratory care to patients • Assist the physician with evaluating patients’ respiratory care needs and optimize the allocation of respiratory care services • Determine the indications for respiratory therapy and the appropriate modalities for providing high-quality, cost-effective care that improves patient outcomes and decreases length of stay • Empower respiratory care practitioners to allocate care using sign- and symptom-based algorithms for respiratory treatment Unfortunately, the implementation of TDPs throughout the United States has been slow. In 2008 the AARC Protocol Implementation Committee conducted a survey to evaluate the barriers to protocol implementation. Over 450 respiratory managers responded to the survey. Despite the overwhelming evidence that protocols clearly improve outcomes and reduce cost, the survey showed that less than 50% of respiratory care was provided by protocols. About 75% of the respondents had at least one protocol in operation. The majority of the hospitals did not have a comprehensive program in place. According to the managers, the medical directors, managers of the department, nurses, and administrators were not perceived as barriers. The biggest barrier to the implementation of protocols was perceived to be the medical staff. The primary reason for the medical staff’s resistance was perceived to be that “staff therapists did not have the skills (e.g., assessment skills) to function under protocols.” The AARC Protocol Implementation Committee states that “[this] perception must change… .”* The essential components of a good TDP program do not come easy. This is because a strong TDP program promises that the respiratory care practitioner, who is identified as “TDP safe and ready,” be qualified to (1) systematically collect the appropriate clinical data, (2) formulate a uniform and accurate assessment, and (3) select a uniform and optimal treatment within the limits set by the protocol (Figure 9-1). The converse, however, is also true: When the respiratory care practitioner is not “TDP safe and ready,” the collection of clinical data is not done at all or is incomplete. As a result, nonuniform or inaccurate assessments are made, resulting in nonuniform or inaccurate treatment selections (Figure 9-2). This inappropriate and ineffective type of respiratory therapy leads to the misallocation of care, the administration of unneeded care, and—most important—the nonprovision of needed patient care. The bottom line is poor-quality patient care and unnecessary costs. To be sure, the development and implementation of a strong TDP program require some fundamental knowledge, training, and practice, but the benefits are worth the price. The essential components of a good TDP program are discussed in the following paragraphs. As shown in Figure 9-3, the essential knowledge base for a successful TDP program includes (1) the anatomic alterations of the lungs caused by common respiratory disorders, (2) the major pathophysiologic mechanisms activated throughout the respiratory and cardiac systems as a result of the anatomic alterations, (3) the common clinical manifestations that develop as a result of the activated pathophysiologic mechanisms, and (4) the treatment modalities used to correct them. In other words, the clinical manifestations demonstrated by the patient do not arbitrarily appear but are the result of anatomic lung alterations and pathophysiologic events. Using the knowledge base described above, the respiratory care practitioner must also be competent in performing the actual assessment process. This means that the practitioner can (1) quickly and systematically gather the clinical information demonstrated by the patient, (2) formulate an accurate assessment of the clinical data (i.e., identify the cause and severity of the problem), (3) select an optimal treatment modality, and (4) document this process quickly, clearly, and precisely. In the clinical setting, the practice—and mastery—of the assessment process is absolutely central and essential to the success of a good TDP program (Figure 9-4). In other words, immediately after the respiratory care practitioner identifies the appropriate clinical manifestations (clinical indicators), an assessment of the data must be performed, and a treatment plan must be formulated. For the most part the assessment is primarily directed at the anatomic alterations of the lungs that are causing the clinical indicators (e.g., bronchospasm) and the severity of the clinical indicators. For example, an appropriate assessment for the clinical indicator of wheezing might be bronchospasm—the anatomic alteration of the lungs. If the practitioner assesses the cause of the wheezing correctly as bronchospasm, then the correct treatment selection would be a bronchodilator treatment from the Aerosolized Medication Therapy Protocol (see Protocol 9-4, page 122). If, however, the cause of the wheezing is correctly assessed to be excessive airway secretions, then the appropriate treatment plan would entail a specific treatment modality under the Bronchopulmonary Hygiene Therapy Protocol, such as cough and deep breathing or chest physical therapy (see Protocol 9-2, page 120). Table 9-1 illustrates common clinical manifestations (i.e., clinical indicators), assessments, and treatment selections routinely made by the respiratory care practitioner. TABLE 9-1 *These procedures should be performed only as ordered by the physician. The frequency at which a respiratory therapy modality is to be administered is just as important as the correct selection of a respiratory therapy treatment. Often the frequency of treatment must be up-regulated or down-regulated on a shift-by-shift, hour-to-hour, minute-to-minute, or even (in life-threatening situations) second-to-second basis. Such frequency changes must be made in response to a severity assessment. In a good TDP program, the well-seasoned respiratory care practitioner routinely and systematically documents many severity assessments throughout each working day. For the new practitioner, however, a predesigned Severity Assessment Rating Form may be used to enhance this important part of the assessment process. One excellent, semiquantitative method of accomplishing this is illustrated in Table 9-2. The clinical application of this severity assessment is provided in the following case example. TABLE 9-2 Respiratory Care Protocol Severity Assessment
The Therapist-Driven Protocol Program and the Role of the Respiratory Care Practitioner
Introduction
The “Knowledge Base” Required for a Successful Therapist-Driven Protocol Program
The “Assessment Process Skills” Required for a Successful Therapist-Driven Protocol Program
Clinical Data (indicators)
Assessments
Treatment Selections
Vital Signs
↑Breathing rate, ↑blood pressure, ↑pulse
Respiratory distress
Treat underlying cause
Abnormal Airway Indicators
Wheezing
Bronchospasm
Bronchodilator treatment
Inspiratory stridor
Laryngeal edema
Cool mist
Rhonchi
Secretions in large airways
Bronchial hygiene treatment
Crackles
Secretions in distal airways
Treat underlying cause—e.g., congestive heart failure (CHF)
Hyperinflation treatment
Cough Effectiveness Indicators
Strong cough
Good ability to mobilize secretions
None
Weak cough
Poor ability to mobilize secretions
Bronchial hygiene treatment
Abnormal Secretion Indicators
Abnormal Lung Parenchyma Indicators
Bronchial breath sounds
Atelectasis
Hyperinflation treatment, oxygen treatment
Dull percussion note
Infiltrates or effusion
Treat underlying cause
Opacity on chest X-ray
Fibrosis
No specific treatment
Restrictive pulmonary function test values
Consolidation
No specific, effective respiratory care treatment
Depressed diaphragm on X-ray
Air trapping and hyperinflation
Treat underlying cause
Abnormal Pleural Space Indicators
Hyperresonant percussion note
Pneumothorax
Evacuate air* and hyperinflation treatment
Dull percussion note
Pleural effusion
Evacuate fluid* and hyperinflation treatment
Abnormalities of the Chest Shape and Motion
Paradoxical movement of the chest wall
Flail chest
Mechanical ventilation*
Barrel chest
Air trapping (hyperinflation)
Treat underlying cause—e.g., asthma
Posterior and lateral curvature of spine
Kyphoscoliosis
Bronchial hygiene treatment
Arterial Blood Gases—Ventilatory
pH↑, Paco2↓,  ↓
↓
Acute alveolar hyperventilation
Treat underlying cause
pH N, Paco2↓,  ↓↓
↓↓
Chronic alveolar hyperventilation
Generally none
pH↓, Paco2↑,  ↑
↑
Acute ventilatory failure
Mechanical ventilation*
pH N, Paco2↑,  ↑↑
↑↑
Chronic ventilatory failure
Low-flow oxygen, bronchial hygiene
Sudden Ventilatory Changes on Chronic Ventilatory Failure (CVF)
pH↑, Paco2↑,  ↑↑, Pao2↓
↑↑, Pao2↓
Acute alveolar hyperventilation on CVF
Treat underlying cause
pH↓, Paco2↑↑,  ↑ Pao2↓
↑ Pao2↓
Acute ventilatory failure on CVF
Mechanical ventilation*
Metabolic
pH↑, Paco2 N, or ↑,  ↑, Pao2 N
↑, Pao2 N
Metabolic alkalosis
Give potassium*—Hypokalemia
Give chloride*—Hypochloremia
pH↓, Paco2 N or ↓,  ↓, Pao2↓
↓, Pao2↓
Metabolic acidosis
Give oxygen—Lactic acidosis
pH↓, Paco2 N or ↓,  ↓, Pao2 N
↓, Pao2 N
Metabolic acidosis
Give insulin*—Ketoacidosis
pH↓, Paco2 N or ↓,  ↓, Pao2 N
↓, Pao2 N
Metabolic acidosis
Renal therapy*
Indication for Mechanical Ventilation
pH↑, Paco2↓,  ↓, Pao2↓
↓, Pao2↓
Impending ventilatory failure
Mechanical ventilation
pH↓, Paco2↑,  ↑, Pao2↓
↑, Pao2↓
Ventilatory failure
pH↓, Paco2↑,  ↑, Pao2↓
↑, Pao2↓
Apnea
Oxygenation Status
Pao2 < 80 mm Hg
Mild hypoxemia
Oxygen treatment and treat underlying cause
Pao2 < 60 mm Hg
Moderate hypoxemia
Pao2 < 40 mm Hg
Severe hypoxemia
Oxygen Transport Status
↓Pao2, anemia, ↓cardiac output
Inadequate oxygen transport
Oxygen treatment and treat underlying cause
Severity Assessment
Item
0 Points
1 Point
2 Points
3 Points
4 Points
Respiratory history
Negative for smoking or history not available
Smoking history <1 pack a day
Smoking history >1 pack a day
Pulmonary disease
Severe or exacerbation
Surgery history
No surgery
General surgery
Lower abdominal
Thoracic or upper abdominal
Thoracic with lung disease
Level of consciousness
Alert, oriented, cooperative
Disoriented, follows commands
Obtunded, uncooperative
Obtunded
Comatose
Level of activity
Ambulatory
Ambulatory with assistance
Nonambulatory
Paraplegic
Quadriplegic
Respiratory pattern
Normal rate 8-20/min
Respiratory rate 20-25/min
Patient complains of dyspnea
Dyspnea, use of accessory muscles, prolonged expiration
Severe dyspnea, use of accessory muscles, respiratory rate >25, and/or swallow
Breath sounds
Clear
Bilateral crackles
Bilateral crackles and rhonchi
Bilateral wheezing, crackles, and rhonchi
Absent and/or diminished bilaterally and/or severe wheezing, crackles, or rhonchi
Cough
Strong, spontaneous, nonproductive
Excessive bronchial secretions and strong cough
Excessive bronchial secretions but weak cough
Thick bronchial secretions and weak cough
Thick bronchial secretions but no cough
Chest X-ray
Clear
One lobe: infiltrates, atelectasis, consolidation, or pleural effusion
Same lung, two lobes: infiltrates, atelectasis, consolidation, or pleural effusion
One lobe in both lungs: infiltrates, atelectasis, consolidation, or pleural effusion
Both lungs, more than one lobe: infiltrates, atelectasis, consolidation, or pleural effusion
Arterial blood gases and/or oxygen saturation measured by pulse oximeter (Spo2)
Normal
Normal pH and Paco2 but Pao2 60-80 and/or Spo2 91-96%
Normal pH and Paco2 but Pao2 40-60 and/or Spo2 85-90%
Acute respiratory alkalosis, Pao2 < 40 and/or Spo2 80-84%
Acute respiratory failure, Pao2 < 80 and/or Spo2 < 80%
Severity Index
Total Score
Severity Assessment
Treatment Frequency
1-5
Unremarkable
As needed
6-15
Mild
Two or three times a day
16-25
Moderate
Four times a day or as needed
Greater than 26
Severe
Two to four times a day and as needed;
Alert attending physician
The Therapist-Driven Protocol Program and the Role of the Respiratory Care Practitioner

 41, and Pa
41, and Pa