The Standard Transthoracic Echo Study
INDICATIONS FOR TRANSTHORACIC ECHO
The versatility of transthoracic echo (TTE) means that it can play a useful role in a diverse range of clinical situations. The British Society of Echocardiography (BSE) has published guidance on the appropriate clinical indications for TTE (see Further Reading). The American College of Cardiology Foundation has also produced guidance (jointly with a number of other societies). The two sets of guidelines are broadly similar and describe echo as being an appropriate investigation in the assessment of patients with:
symptoms, signs or previous tests that indicate possible structural heart disease
heart murmurs when associated with symptoms or when structural heart disease is suspected, and the follow-up of those with known significant valvular stenosis or regurgitation
prosthetic valves (except asymptomatic patients with mechanical valves or those in whom no further intervention would be undertaken)
suspected or proven infective endocarditis
known or suspected ischaemic heart disease (e.g. diagnostic stress echo, assessment following myocardial infarction)
known or suspected cardiomyopathy
suspected pericarditis, pericardial effusion, cardiac tamponade or pericardial constriction, and follow-up of patients with known moderate or large pericardial effusions (or small effusions if there has been a clinical change)
suspected or possible cardiac masses (and follow-up of patients following surgical excision of a cardiac mass)
pulmonary disease (with cardiac involvement)
pulmonary hypertension
thromboembolism
neurological disorders (with cardiac involvement)
arrhythmia, palpitations and syncope (with suspected/possible structural heart disease)
prior to cardioversion (unless the patient is on long-term anticoagulants at a therapeutic level and there is no suspicion of structural heart disease)
hypertension (if left ventricular hypertrophy (LVH)/dysfunction or aortic coarctation are suspected)
aortic disease (e.g. monitoring of aortic root dimensions in Marfan syndrome)
known or suspected congenital heart disease.
Transthoracic echo is also indicated for pre-operative assessment in patients awaiting elective or semi-urgent surgery if they have:
known ischaemic heart disease with a reduced functional capacity
unexplained breathlessness (with an abnormal electrocardiogram and/or chest X-ray)
a murmur (with suspected structural heart disease or in the presence of cardiac or respiratory symptoms).
It is essential that echo requests contain adequate clinical data both to judge the appropriateness of the request and also to allow the sonographer to place the echo findings into an appropriate clinical context (see the box ‘Sensitivity, specificity and Bayesian analysis’). Echo requests must therefore carry appropriate clinical details and contain information about known cardiac diagnoses or previous cardiac interventions/surgery (e.g. prosthetic valves). Clinicians requesting echo studies should be encouraged to include specific questions with their request (e.g. ‘Does this patient have pulmonary hypertension?’), as this provides a clear focus for the echo study and ensures that the sonographer can address the specific concerns of the clinician.
SENSITIVITY, SPECIFICITY AND BAYESIAN ANALYSIS
A perfect diagnostic test would always detect an abnormality when present (‘true positive’) or rule out an abnormality when absent (‘true negative’). However, as with virtually every clinical test, echo has its limitations and can sometimes produce an erroneous result. Detecting an abnormality when in fact none is present is called a ‘false positive’, and missing an abnormality that is present is a ‘false negative’. The terms ‘sensitivity’ and ‘specificity’ are often used to describe the accuracy of a test:
Sensitivity is the degree to which a test will identify all those who have a particular disease – if 100 people with disease ‘X’ undergo a test with 90 per cent sensitivity, the test will detect the disease in 90 of them (but will produce a false negative in 10).
Specificity is the degree to which a test will identify all those without a particular disease – if 100 people without disease ‘X’ undergo a test with 90 per cent specificity, the test will be normal in 90 of them (but will produce a false positive in 10).
The number of people who receive false positive/negative results is determined not only by the sensitivity and specificity of the test, but also by the population prevalence of the disease in question. Screening a large number of normal individuals for a rare disease using a test with imperfect specificity will produce a relatively large number of false positive results.
The technique of Bayesian analysis takes this into account by considering how likely it is that the patient has the disease in question (the pretest probability) in order to predict how likely it is that a positive or negative test result is genuinely positive or negative. In general terms, a positive test result for disease ‘X’ is more likely to be a true positive if the patient already had a high probability of having disease ‘X’ before the test was done – it is therefore important to know a patient’s full clinical details before performing a test such as an echo in order to judge the likely significance of any abnormalities that you find.
Triage of inpatient echo requests
Echo should be performed immediately if acute cardiac tamponade is suspected following an interventional procedure or if a patient presents with likely acute (massive) pulmonary embolism and echo is likely to help in deciding whether to administer thrombolysis.
Urgent echo (within 24 hours, or even sooner depending on the clinical situation) is required for patients who are unstable with infective endocarditis, who have a new murmur following acute or recent myocardial infarction, who are persistently hypotensive (and not responding to treatment) for unknown reasons, have suspected pericardial effusion/bleeding/tamponade or have suspected aortic dissection.
Other inpatient echo requests can be performed more routinely, but should nevertheless be undertaken on an inpatient basis as soon as practicable. If circumstances do not permit this, discuss the request with the referring clinician to see if the study can be deferred and performed on an outpatient basis once the patient is discharged from hospital.
PATIENT PREPARATION
Patients attending for an echo study may feel anxious, not only about having the test itself but also about any abnormalities that it may reveal. To help reduce anxiety, describe the test to patients in clear and reassuring terms – explain to patients why they are having an echo, whether any special preparation is needed before they attend, what happens during the scan and how long it is likely to take. Reassure patients that having an echo is safe and painless. Patients can eat and drink normally before attending for a standard TTE, and they can take their medication as usual.
It is good practice to offer patients an information leaflet before they attend (and to make available large-print/Braille and translated versions as appropriate). The patient information leaflet and/or appointment letter can also invite the patient to bring a friend or relative if they wish to have someone accompany them during the echo. If a friend or relative does not accompany the patient when they attend, offer the patient a chaperone in line with hospital policy.
Prior to performing the echo study, it is good practice to record the patient’s height and weight, as this will allow the indexing of echo measurements for body surface area. You should also ideally record the patient’s heart rate and blood pressure.
Once you have checked that the patient understands the test that is about to be performed, ask the patient to undress to the waist for the echo study. Always offer female patients a gown to wear during the echo (even if the sonographer is female). Ask the patient to sit on the echo couch and recline at 45°, rolling on to their left side. The patient should then raise their left arm and place their left hand behind their head. Be sure to check if the patient has any physical limitations that may make it difficult or uncomfortable for them to adopt this position. If so, you may need to adapt the patient’s position until they are comfortable. Sonographers who prefer to scan left-handed will also need to adapt the patient’s positioning accordingly.
When the patient is in a comfortable position, apply the ECG electrodes and ensure that a clear ECG tracing is visible on the screen of the echo machine. You may need to adjust the electrodes and/or the ECG gain setting to obtain a good trace. Ensure that the correct patient identification and clinical details are entered into the echo machine, and then perform and report the study as described in the sections that follow. At the end of the study, explain to the patient that you will be writing a report which will be sent to the referring clinician. Patients may ask you what the study has shown, but you should not discuss the study findings at this stage and it is usually better to redirect persistent requests for information to the referring clinician.
STANDARD WINDOWS AND VIEWS
The BSE has produced a guidance document, entitled A Standard Transthoracic Echocardiogram, which provides a framework for performing a comprehensive transthoracic echo study. This document forms the basis of the approach outlined in this chapter, and identifies minimum requirements and recommendations (in terms of views and measurements).
A comprehensive echo study should include not only the minimum requirements but also the recommendations, and this is particularly important in individuals who are being scanned for the first time. Moreover, if pathology is found, then additional views/measurements (over and above the minimum requirements and recommendations) may be appropriate. However, it is also acknowledged that some echo studies (for instance follow-up studies, or focussed/targeted studies) will not necessarily need to include all of the minimum requirements described here.
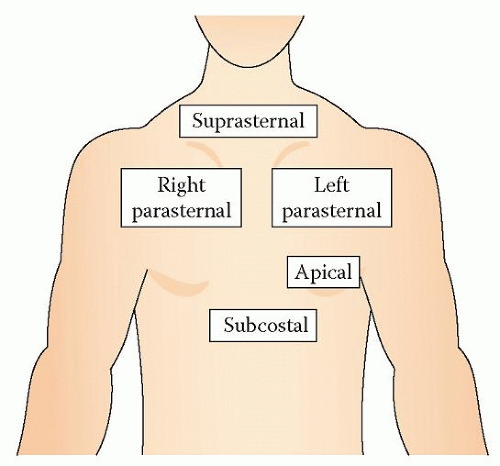
There are five TTE windows (Fig. 6.1), each providing one or more views of the heart. The right parasternal window is optional and can be used when other views are suboptimal or when additional information is needed:
Left parasternal window
Parasternal long axis view
Parasternal right ventricular (RV) inflow view
Parasternal RV outflow view
Parasternal short axis view (base, mid-cavity, apex)
(Right parasternal window)
Apical window
Apical 4-chamber view
Modified apical 4-chamber view (to assess the right heart)
Apical 5-chamber view
Apical 2-chamber view
Apical 3-chamber (long axis) view
Subcostal window
Subcostal long axis view
Subcostal short axis view
Suprasternal window
Aorta view.
Left parasternal window
The left parasternal window is located to the left of the sternum, usually in the third or fourth intercostal space, but in some patients you may need to adjust the position to optimize the image by moving the probe up/down a rib space or further towards/away from the sternum. From the left parasternal window a number of views can be obtained.
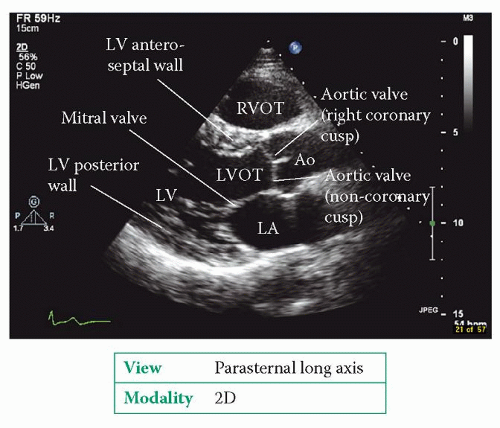
Parasternal long axis view
The parasternal long axis (LAX) view is shown in Fig. 6.2. To obtain the view with the probe in the left parasternal window, rotate the probe so that the probe’s ‘reference point’ (sometimes a ‘dot’) is pointing towards the patient’s right shoulder.
For an optimal view, aim to position the probe so that the view cuts through the centre of the mitral and aortic valves, without foreshortening the left ventricle (LV) or ascending aorta. In this view:
Use 2D to:
measure LV cavity size and wall thickness (this can be done using M-mode if you prefer)
assess LV radial function (thickening and motion of the anteroseptal and inferolateral (also known as posterior) wall)
inspect the appearance of the left atrium (LA) and measure its size at end-systole
assess structure and mobility of the mitral valve – in this view, the A2 and P2 segments are visible
assess structure and mobility of the aortic valve. The right and non-coronary cusps are visible and normally have a central closure line – an eccentric closure line suggests bicuspid aortic valve
inspect the appearance of the left ventricular outflow tract (LVOT) and measure its diameter (no more than 1 cm below the aortic valve annulus)
measure the diameter of the right ventricular outflow tract (RVOT)
inspect and measure the aortic root (at the level of the aortic annulus, sinuses of Valsalva and sinotubular junction)
inspect and measure the proximal ascending aorta (tilt the probe superiorly to view the mid-ascending aorta)
look at the descending aorta as it runs behind the LA – this is a useful landmark for assessing a pericardial/pleural effusion
assess the pericardium and check for any pericardial (or pleural) effusion.
Use M-mode:
with the cursor placed at the level of the aortic valve cusp tips to measure aortic root diameter (at end-diastole) and LA diameter (at end-systole), as an alternative to 2D measurement
with the cursor placed at the level of the mitral valve leaflet tips to measure mitral valve E point septal separation (the distance between the E point of the anterior mitral leaflet and the septum, p. 130)
Use colour Doppler to:
assess the aortic valve for stenosis or regurgitation (if regurgitation is present, measure the vena contracta and the width of the jet in relation to the diameter of the LVOT)
assess the mitral valve for stenosis or regurgitation (if regurgitation is present, measure the vena contracta)
check for flow acceleration in the LVOT in association with septal hypertrophy
check the integrity of the interventricular septum (IVS).
Parasternal right ventricular inflow view
This view is obtained from the left parasternal window by tilting the probe so that it points more medially and towards the patient’s right hip, bringing the right atrium (RA), tricuspid valve and RV into view (Fig. 6.3).
Use 2D to:
assess size and function of the RV
inspect the structure of the RA. In this view it may be possible to see the coronary sinus and the inferior and superior vena cavae as they join the RA. There may be a prominent Eustachian valve at the junction with the inferior vena cava (IVC)
assess the structure and mobility of the tricuspid valve (the two leaflets seen are the anterior and posterior leaflets).
Use colour Doppler to examine tricuspid valve inflow and check for regurgitation.
Parasternal right ventricular outflow view
This view is obtained from the left parasternal window by tilting the probe so that it points more laterally and towards the patient’s left shoulder, bringing the RVOT, pulmonary valve and pulmonary artery into view (Fig. 6.4). It may be possible to see the pulmonary artery bifurcation.
Use 2D to:
assess the structure of the RVOT and main pulmonary artery; check for the presence of thrombus (pulmonary embolus)
assess the structure and mobility of the pulmonary valve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree