The Role of Exercise Testing in Chest Pain Units: Evolution, Application, Results
Ezra A. Amsterdam
J. Douglas Kirk
Deborah B. Diercks
William R. Lewis
Samuel D. Turnipseed
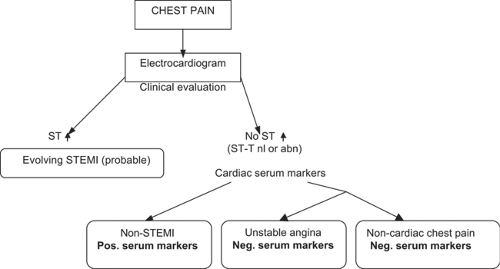
Despite advances in the management of low-risk patients presenting to the emergency department (ED) with chest pain, this syndrome remains a major clinical challenge (1), accounting for over 8 million ED visits and more than two million hospital admissions annually in the United States for presumed acute coronary syndrome (ACS) at a cost of cost of $8 billion (2). However, a coronary event is confirmed in only a minority of these patients (3) who pose a dilemma to the clinician because of inadvertent discharge of those with a life-threatening condition versus unnecessary admission for a benign process with associated expense. The continuum of risk for this population is depicted in Figure 10-1 and the single largest group is the one with noncardiac chest pain. The early era of coronary care units (CCUs) had a low threshold for admission of these patients, as reflected in the recommendation that “Patients should be admitted to the CCU solely on suspicion of having a myocardial infarction” (4). To the degree that this concept has persisted, it reflects a focus on patient welfare as well as the litigation potential of missed ACS (5). Although appropriate alternative approaches have subsequently evolved, inadvertent discharge of patients with ACS remains a challenge. Indeed, recent data suggest that this problem persists at a rate of up to 5% and accounts for a substantial morbidity and mortality (6). However, a consequence of the low threshold for admission has been large numbers of unnecessary hospitalizations and inefficient resource utilization.
Chest pain units (CPU) have been developed to provide safe, accurate and cost-effective management of low-risk patients presenting with possible ACS. Their original purpose was to facilitate rapid coronary reperfusion therapy, but these units have subsequently evolved into centers for management of the lower risk population that comprises the majority of patients presenting with chest pain. The latter include those without objective evidence of myocardial ischemia or injury on presentation in whom accelerated risk stratification can identify those requiring admission and those who can be safely discharged with outpatient follow-up (7,8,9,10,11,12,13,14). Basic to this approach is the accelerated diagnostic protocol (ADP) culminating in stress testing after a negative initial assessment for ACS. The primary stress test has been exercise electrocardiography (ECG). The ADP is predicated on initial recognition of patients with low clinical risk on presentation.
Identification of Low Clinical Risk
Multiple studies have demonstrated that low clinical risk can be recognized on presentation and that this finding identifies a group that neither requires nor benefits from traditional intensive care. Lee et al reported that in patients admitted to rule out a coronary event, those with <5% probability of acute myocardial infarction (MI) could be identified by type of chest pain, past history, and initial ECG (15). Extension of this approach to over 4,600 patients demonstrated that the initial clinical assessment could distinguish those with less than <1% probability of major complications (16). The prognostic importance of the initial ECG in patients admitted to rule out MI was demonstrated by Brush et al (7), who found that a negative ECG on admission was associated with a 0.6% rate of serious complications during hospitalization compared with a 14% incidence in those with an abnormal ECG. An earlier study indicated that in patients admitted for preinfarction angina, a normal ECG predicted benign early and late outcomes in contrast to ECG evidence of ischemia, which correlated with markedly increased cardiac morbidity and mortality (18). These findings were confirmed by Schroeder and colleagues in their report that in patients in whom MI was ruled out, ECG evidence of ischemia was associated with a 1-year mortality similar to that of post-MI patients (19). An important concept to emerge from these studies was that, although the etiology of chest pain is frequently elusive, basic clinical tools provide powerful estimates of cardiac risk.
Recognition of low clinical risk stimulated alternative approaches to conventional coronary care, such as reduced time in the CCU (20,21), direct admission to a step-down unit (22), and observation in a short stay unit (23). Recent innovations in the management of low-risk patients include guidelines, critical pathways, new serum markers of cardiac injury, novel ECG monitoring systems, early treadmill testing or noninvasive cardiac imaging, coronary calcium screening in the ED, noninvasive coronary angiography by computed tomography, and conventional coronary angiography (7,8,9,10,11,12,13,14,20).
Chest Pain Unit Concept
Risk is low but not negligible in patients selected for CPU evaluation. CPUs provide an integrated approach to management of these patients that affords (a) early identification of clinical risk and (b) further stratification of low-risk patients to identify those who require admission and those who can be discharged (7,8,9,10,11,12,13,14,20). CPUs vary in form and may either occupy a designated structural area or function as virtual units comprising primarily personnel and process. Close coordination between ED physicians and cardiologists is an essential element for successful functioning of the unit. The strategy is based on a protocol-driven process that employs current standards of care for efficient and timely treatment in conformity with the guidelines of the American College of Cardiology (ACC) and American Heart Association (AHA) (24).
Accelerated Diagnostic Protocols
Accelerated dignostic protocols (ADPs) have been increasingly utilized in low-risk patients with the final step comprising one of the cardiac stress tests methods if the ACS is excluded. The most commonly used ADPs usually entail 6 to 12 hours of clinical observation, serial 12-lead ECGs, continuous ECG monitoring, and measurement of serial serum cardiac injury markers (10,12,14,20,24). Positive findings indicate ACS (usually non-ST elevation [non-STE] ACS, rarely ST elevation MI) and mandate admission for further management. Negative findings are consistent with the absence of MI and ischemia at rest. In these cases, a stress test is performed to detect inducible ischemia. Patients with a positive test are admitted, and those with a negative result are discharged to outpatient follow-up. Multiple methods are currently available to detect stress-induced ischemia, the most widely available and readily applicable of which is treadmill exercise testing. The utility of this test in conjunction with ADPs has been has been well demonstrated, as indicated by its safety and predictive accuracy in this setting.
Evolution of Early Exercise Testing
Until it was validated by recent studies, there were strong admonitions against early exercise testing even in low-risk patients presenting with symptoms suggestive of ACS (9,25). The evolution of this approach is reflected in the statement of The 31st Bethesda Conference on Emergency Cardiac Care (1999) that “ADPs, including exercise testing as a key element, have been associated with reduced hospital stay and lower costs” (10). The absence of adverse effects and the accurate identification of low clinical risk were also recognized. A subsequent Science Advisory of the AHA concluded that contemporary studies “confirmed the safety of symptom-limited treadmill exercise ECG testing after 8 to 12 hours of evaluation in patients who have been identified as being at low to intermediate risk by a clinical algorithm that uses serum markers of myocardial necrosis and resting ECGs” (26). This strategy is incorporated in the 2002 guidelines of the ACC/AHA for management of patients with non-ST-elevation ACS in which it is recommended that exercise testing can be performed in stable, low-risk patients if “a follow-up 12-lead ECG and cardiac marker measurements after 6 to 8 hours of observation are normal” (23). Recent exercise testing guidelines are in accord with these recommendations (27,28). It is noteworthy that these recent recommendations reflect evolution from earlier versions, which advised exercise testing only after patients had been symptom free for a “minimum of 48 hours” (29).
All studies of early exercise testing in patients presenting with chest pain have required that patients are clinically stable with no ECG evidence of ischemia/injury. The criteria for a
positive test for myocardial ischemia are the standard indicators: ≥1.0 mm horizontal or downsloping ST segment shift 60 to 80 msec after the J point. Other exercise-induced alterations that indicate an abnormal test and the need for further evaluation include angina, arrhythmias, and exercise-induced fall in blood pressure. The first two investigations of this method included only small numbers of patients, but they demonstrated its safety in low-risk patients in the ED setting (30,31), and its utility was confirmed in multiple subsequent publications (Table 10-1). Of note, there have been no reports of adverse events in any study of early exercise testing of low-risk patients.
positive test for myocardial ischemia are the standard indicators: ≥1.0 mm horizontal or downsloping ST segment shift 60 to 80 msec after the J point. Other exercise-induced alterations that indicate an abnormal test and the need for further evaluation include angina, arrhythmias, and exercise-induced fall in blood pressure. The first two investigations of this method included only small numbers of patients, but they demonstrated its safety in low-risk patients in the ED setting (30,31), and its utility was confirmed in multiple subsequent publications (Table 10-1). Of note, there have been no reports of adverse events in any study of early exercise testing of low-risk patients.
Early Exercise Testing in an Accelerated Diagnostic Protocol
The first study of exercise testing in patients with the clinical profile of those currently included in ADPs was published from our institution in 1994. In this investigational protocol, selected patients presenting with chest pain who were designated for admission by ED physicians to rule out ACS underwent immediate treadmill testing (32) (Table 10-1). The study group comprised 93 patients in whom ED symptom-limited exercise testing was performed by a cardiologist using a modified Bruce protocol without prior measurement of any markers. The test was performed within a median time of less than 1 hour from the decision to admit. Positive tests occurred in 13% of patients, negative in 64%, and nondiagnostic (no ischemia but peak heart rate <85% of age-predicted maximum) in 13%. Ischemic ECG changes occurred at a significantly lower percentage of age-predicted maximal heart rate (70%) in patients with true-positive tests compared to those with false-positives (>90%) (Fig. 10-2). No complications were associated with exercise testing. Coronary angiography revealed significant coronary artery disease (CAD) in 6 of the 13 patients with positive tests, 5 of whom had multivessel involvement. A majority (54%) of the 81 patients with negative or nondiagnostic results was discharged immediately after the exercise test. At 6-month follow-up, there were no coronary events in patients with negative or nondiagnostic exercise tests. There are several unique aspects of this study, which demonstrated the utility of early exercise testing in low-risk patients and provided the basis for our current approach of “immediate” exercise testing in low-risk patients without excluding MI by a traditional series of negative cardiac serum markers. In contrast to the preceding studies, it included only patients who were assigned to admission for a traditional rule-out MI protocol. In these patients, exercise testing was performed prior to the latter process, there were no adverse effects of testing, true- and false-positive tests were related to the heart rate at ST-segment depression, the majority of patients were discharged immediately following a negative or nondiagnostic test, and there were no coronary events during the posthospital course. Of note, one patient with a positive test was found to have non-ST-elevation MI by subsequent serial serum enzymes. Coronary angiography revealed right coronary artery stenosis, coronary angioplasty was performed, and the clinical course was uncomplicated.
Gibler and associates demonstrated the utility of early exercise testing in 782 patients in whom low risk was indicated by an ADP (33) (Table 10-1). Their protocol included serial ECGs and serum CK-MB, 9 hours of continuous ST-segment monitoring, and a resting ECG followed by symptom-limited exercise testing in those with negative findings. There were no adverse effects and no mortality at 30-day follow-up in the patients with negative tests. The negative predictive value of the exercise test was 99%. Although the positive predictive value was less than 50%, only 9 of 782 patients (<2%) had positive exercise tests, which was lower than in our initial investigation (32).
Table 10-1. Studies of Exercise ECG Testing in Chest Pain Centersa | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree