3
The Rhythm of the Heart
So far we have only considered the spread of depolarization that follows the normal activation of the sinoatrial (SA) node. When depolarization begins in the SA node the heart is said to be in sinus rhythm. Depolarization can, however, begin in other places. Then the rhythm is named after the part of the heart where the depolarization sequence originates, and an ‘arrhythmia’ is said to be present.
When attempting to analyse a cardiac rhythm remember:
• Atrial contraction is associated with the P wave of the ECG.
• Ventricular contraction is associated with the QRS complex.
• Atrial contraction normally precedes ventricular contraction, and there is normally one atrial contraction per ventricular contraction (i.e. there should be as many P waves as there are QRS complexes).
The keys to rhythm abnormalities are:
• The P waves – can you find them? Look for the lead in which they are most obvious.
• The relationship between the P waves and the QRS complexes – there should be one P wave per QRS complex.
• The width of the QRS complexes (should be 120 ms or less).
• Because an arrhythmia should be identified from the lead in which the P waves can be seen most easily, full 12-lead ECGs are better than rhythm strips.
THE INTRINSIC RHYTHMICITY OF THE HEART
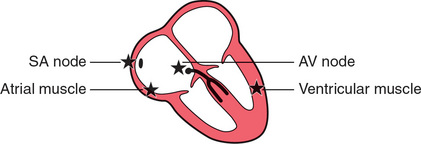
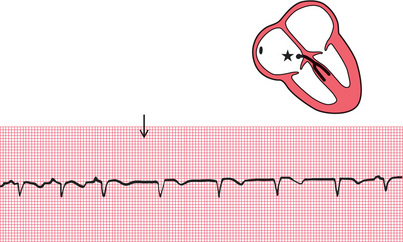
The stars in the figures in this chapter indicate the part of the heart where the activation sequence began. The SA node normally has the highest frequency of discharge. Therefore the rate of contraction of the ventricles will equal the rate of discharge of the SA node. The rate of discharge of the SA node is influenced by the vagus nerves, and also by reflexes originating in the lungs. Changes in heart rate associated with respiration are normally seen in young people, and this is called ‘sinus arrhythmia’ ( Fig. 3.1).

ABNORMAL RHYTHMS
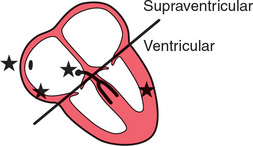
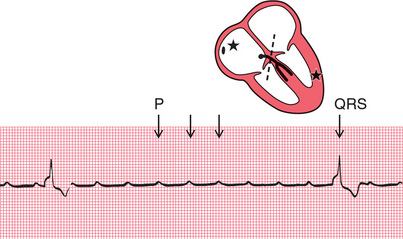
Abnormal cardiac rhythms can begin in one of three places ( Fig. 3.2): the atrial muscle; the region around the atrioventricular (AV) node (this is called ‘nodal’ or, more properly, junctional′); or the ventricular muscle. Although Figure 3.2 suggests that electrical activation might begin at specific points within the atrial and ventricular muscles, abnormal rhythms can begin anywhere within the atria or ventricles.
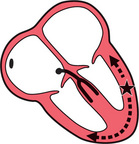
Sinus rhythm, atrial rhythm and junctional rhythm together constitute the ‘supraventricular’ rhythms ( Fig. 3.3). In the supraventricular rhythms, the depolarization wave spreads to the ventricles in the normal way via the His bundle and its branches ( Fig. 3.4). The QRS complex is therefore normal, and is the same whether depolarization was initiated by the SA node, the atrial muscle, or the junctional region.
In ventricular rhythms, on the other hand, the depolarization wave spreads through the ventricles by an abnormal and slower pathway, via the Purkinje fibres ( Fig. 3.5). The QRS complex is therefore wide and is abnormally shaped. Repolarization is also abnormal, so the T wave is also of abnormal shape. Remember:
• Supraventricular rhythms have narrow QRS complexes.
• Ventricular rhythms have wide QRS complexes.
• The only exception to this rule occurs when there is a supraventricular rhythm with right or left bundle branch block, or the Wolff-Parkinson-White (WPW) syndrome, when the QRS complex will be wide (see p. 79).
THE BRADYCARDIAS – THE SLOW RHYTHMS
It is clearly advantageous if different parts of the heart are able to initiate the depolarization sequence, because this gives the heart a series of failsafe mechanisms that will keep it going if the SA node fails to depolarize, or if conduction of the depolarization wave is blocked. However, the protective mechanisms must normally be inactive if competition between normal and abnormal sites of spontaneous depolarization is to be avoided. This is achieved by the secondary sites having a lower intrinsic frequency of depolarization than the SA node.
ATRIAL ESCAPE
If the rate of depolarization of the SA node slows down and a different focus in the atrium takes over control of the heart, the rhythm is described as ‘atrial escape’ ( Fig. 3.6). Atrial escape beats can occur singly.
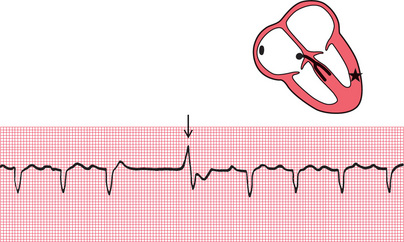
NODAL (JUNCTIONAL) ESCAPE
If the region around the AV node takes over as the focus of depolarization, the rhythm is called ‘nodal’, or more properly, ‘junctional’ escape ( Fig. 3.7).
VENTRICULAR ESCAPE
‘Ventricular escape’ is most commonly seen when conduction between the atria and ventricles is interrupted by complete heart block ( Fig. 3.8).
Ventricular escape rhythms can occur without complete heart block, and ventricular escape beats can be single ( Fig. 3.9).
The rhythm of the heart can occasionally be controlled by a ventricular focus with an intrinsic frequency of discharge faster than that seen in complete heart block. This rhythm is called ‘accelerated idioventricular rhythm’ ( Fig. 3.10), and is often associated with acute myocardial infarction. Although the appearance of the ECG is similar to that of ventricular tachycardia (described later), accelerated idioventricular rhythm is benign and should not be treated. Ventricular tachycardia should not be diagnosed unless the heart rate exceeds 120/min.
EXTRASYSTOLES
Any part of the heart can depolarize earlier than it should, and the accompanying heartbeat is called an extrasystole. The term ‘ectopic’ is sometimes used to indicate that depolarization originated in an abnormal location, and the term ‘premature contraction’ means the same thing.
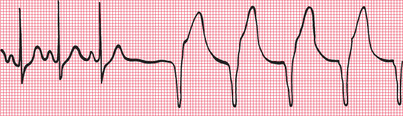
Atrial extrasystoles have abnormal P waves ( Fig. 3.11). In a junctional extrasystole there is no P wave at all, or the P wave appears immediately before or immediately after the QRS complex ( Fig. 3.11). The QRS complexes of atrial and junctional extrasystoles are, of course, the same as those of sinus rhythm.
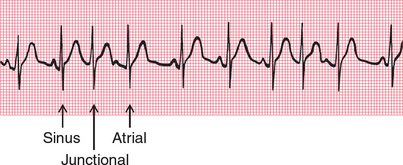
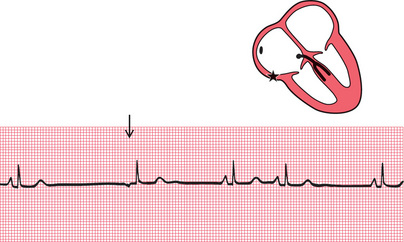
Fig. 3.11 Atrial and junctional (nodal) extrasystoles
Note
• This record shows sinus rhythm with junctional and atrial extrasystoles
• A junctional extrasystole has no P wave
• An atrial extrasystole has an abnormally shaped P wave
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree