Chapter 3
The respiratory muscles
An important concept that will be explored in this chapter is that of imbalance in the demand / capacity relationship of the respiratory muscles, and, in particular, the inspiratory muscles. Evaluating function in the context of relative demand is a pragmatic method of defining ‘weakness’, since it incorporates context. A muscle might not be considered ‘weak’ in absolute terms, but if the demands that are placed upon a ‘normal muscle’ are excessive then it is rendered ‘weak’ functionally. For example, morbidly obese people with normal quadriceps muscle strength have functional weakness by virtue of their greater body mass. The same principle applies to the respiratory muscles: patients with lung fibrosis may have normal inspiratory muscle strength, but the elevated intrinsic inspiratory load generates functional weakness that manifests as reduced inspiratory muscle endurance (Hart et al, 2002). Traditionally, weakness has been defined by reference to measures of strength, but it is important to appreciate that strength is a one-dimensional index of function, and is just one of a number of important functional properties of muscles (see Ch. 4, Fig. 4.1). Thus weakness and dysfunction are multi-dimensional, and can be primary (sub-normal performance) and functional (inadequate for the prevailing demands). The overriding question is whether the muscles’ capability is ‘fit for purpose’, or whether it induces a functional limitation. The latter can be defined as the inability to undertake a task that would be considered normal. For example, the inability of a middle-aged woman to walk on level ground at 3.96 km·h− 1 (1.10 m·s− 1) (Bohannon & Williams Andrews, 2011) without the need to stop and ‘catch her breath’ defines her as being functionally limited by dyspnoea. In Chapter 1, the underlying physiology of dyspnoea and breathing effort was described. Although dyspnoea is a complex phenomenon, a major contributor to its magnitude is the relative intensity of inspiratory muscle work. This is determined by two factors: (1) the prevailing respiratory system mechanics, and (2) the function of the respiratory muscles; in other words, the resistances and elastances that must be overcome during breathing, as well as the capacity of the respiratory muscles to meet these mechanical demands. An exacerbating factor with respect to this relationship is the prevailing ventilatory demand, which is affected by a wide range of factors including aerobic fitness, ventilation / perfusion matching, diffusing capacity and breathing pattern. To add a further layer of complexity to the demand / capacity relationship of the respiratory muscles, many of these factors are interdependent; for example, altered lung mechanics can precipitate a rapid shallow breathing pattern, which in turn increases the demand for minute ventilation because of its effect on the dead space / tidal volume relationship.
This chapter will explore how disease, exercise and posture interact to influence the demand / capacity relationship of the respiratory muscles. In doing so, a theoretical rationale for specific training will be offered. Evidence relating to the influence of respiratory muscle training upon clinical outcomes is considered in Chapter 4.
CHANGES IN RESPIRATORY MUSCLE FUNCTION AND BREATHING MECHANICS
In the various conditions described below there is either: (1) an imbalance in the demand / capacity relationship of the respiratory muscles that contributes to dyspnoea, exercise limitation and even to respiratory failure, or (2) a contribution to symptoms or morbidity that arises from the respiratory system, including the upper airway. This section will therefore describe the abnormalities of respiratory mechanics, respiratory muscle function and ventilatory demand in a range of situations and, in so doing, establish the rationale for training the respiratory muscles. A comprehensive overview of respiratory muscle disorders can also be found in the excellent review of Laghi & Tobin (2003).
Respiratory disease
The primary symptom and exercise-limiting factor in respiratory disease is dyspnoea. In this section the impact of respiratory disease upon respiratory mechanics, respiratory muscle function and ventilatory demand will be described. Readers wishing to know more about the physiological basis of respiratory disease are referred to Hamid and colleagues’ comprehensive text on the subject (Hamid et al, 2005).
Chronic obstructive pulmonary disease
The hallmark of chronic obstructive pulmonary disease (COPD) is expiratory flow limitation, which results from both reduced lung recoil and airway tethering (see Ch. 1), in addition to intrinsic airway narrowing. Although the most obvious repercussion of airway narrowing for the respiratory muscles is an increased flow resistive work of breathing, this is only the tip of the iceberg. In recent years, the phase ‘dynamic hyperinflation’ has emerged to describe how the loss of lung recoil and airway narrowing disrupt normal breathing mechanics during exercise. Hyperinflation is a pathophysiological manifestation of airway obstruction, and the consequent expiratory flow limitation, which lead to incomplete lung emptying, i.e., expiration is curtailed before the lungs have reached their equilibrium volume (functional residual capacity: FRC). The lungs therefore become hyperinflated. In severe COPD, hyperinflation is present at rest (static hyperinflation), but during exercise even mild obstruction results in a state of dynamic hyperinflation, the severity of which is proportional to the severity of flow limitation and the magnitude of the ventilatory demand.
Figure 3.1 illustrates how, during exercise, expiratory flow limitation stimulates migration of the tidal flow loop towards total lung capacity (TLC), increasing end-expiratory lung volume (EELV) and reducing inspiratory capacity (IC). Although dynamic hyperinflation serves to maximize tidal expiratory flow under conditions of expiratory flow limitation (by moving the tidal flow loop away from the maximum envelope), the requirement to breathe at higher ranges of the TLC increases the elastic load presented to the inspiratory muscles by the lungs and chest wall. This creates a ‘restrictive’ pulmonary defect. The most important mechanical and sensory repercussions of expiratory flow limitation are therefore borne by the inspiratory muscles. However, the repercussions of hyperinflation and / or expiratory flow limitation are not limited to an increase in the elastic work of breathing; inspiratory muscle loading is exacerbated in three further ways:
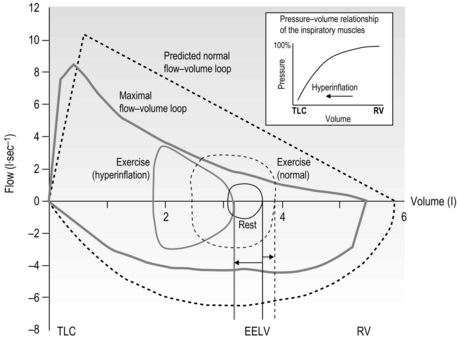
Figure 3.1 Comparison of the response of the exercise tidal flow volume in a person with expiratory flow limitation (EFL) (solid lines), compared with that predicted for someone with normal lungs (dashed lines). Note that in the presence of EFL there is encroachment upon the inspiratory capacity in order to increase minute ventilation (flow volume loop shifts to the left and end-expiratory lung volume (EELV) increases). The person with normal lungs (dashed lines) is able to increase minute ventilation by utilizing both their inspiratory and expiratory reserve volumes (EELV decreases). The inset illustrates the pressure–volume relationship of the inspiratory muscles showing that, as lung volume increases from residual volume (RV) towards total lung capacity (TLC) (as occurs in hyperinflation) the inspiratory muscles become weaker.
• By inducing functional weakening of the inspiratory muscles (see inset to Fig. 3.1). Foreshortening of expiration alters diaphragm geometry, making it flatter and moving the inspiratory muscles to a weaker portion of their pressure–volume relationship (Decramer, 1997).
• By generating intrinsic positive end-expiratory pressure (PEEPi). Expiration ends before all of the forces acting on the lung are in equilibrium, so inspiration is initiated under a positive expiratory load.
• By forcing inspiratory time to shorten. This is another adaptive response, in this case to allow more time for expiration. The cost is to move the inspiratory muscles to a weaker portion of their force–velocity relationship (the faster a muscle contracts, the lower is its force-generating capacity).
Hyperinflation has also been shown to impair respiratory muscle blood flow in a dog model (Kawagoe et al, 1994); in this study, despite an almost two-fold increase in the work of breathing, diaphragm blood flow remained unchanged and accessory muscle blood flow fell during acute hyperinflation. It is not clear whether hyperinflation exerts the same effect in human beings with COPD, but impaired accessory muscle perfusion in the face of an increased demand for muscle work would predispose these muscles to fatigue and / or accumulation of metabolic by-products (see section ‘Respiratory muscle involvement in exercise limitation’).
Thus, COPD-induced changes in respiratory mechanics exert a very potent influence upon dyspnoea because they affect both the demand for inspiratory pressure generation and the capacity of the inspiratory muscles to generate sufficient pressure to meet that demand (see Fig. 3.1). Both phenomena increase the requirement for inspiratory motor drive and intensify dyspnoea (O’Donnell, 2001). However, the inspiratory muscle dysfunction of COPD is not confined to the functional (secondary) weakening precipitated by hyperinflation (Similowski et al, 1991; Polkey et al, 1996). There is also primary dysfunction due to abnormalities within the muscle tissue itself, which lead to declines in strength and endurance (Levine et al, 2003; Barreiro et al, 2005; Ottenheijm et al, 2005). This deterioration of muscle may be in part due to disuse (sedentary lifestyles), but is more likely to be the result of oxidative stress (Barreiro et al, 2005) resulting from the systemic manifestations of COPD, including the chronic inflammatory state. Furthermore, malnutrition causes generalized muscle weakness, which may exacerbate disease-specific respiratory muscle weakness (Decramer, 2001). Finally, the use of oral corticosteroids has been shown to have a myopathic influence upon the respiratory muscles of patients without respiratory disease, who show significant reductions in strength (~ 30%) and endurance (~ 50%) over the treatment period (Weiner et al, 1993; Weiner et al, 1995). Although these changes show some reversal following cessation of corticosteroid treatment, function may take as long as 6 months to normalize (Weiner et al, 1993). Since primary and secondary dysfunction coexist, there is a significant impairment in the capacity of the inspiratory muscles to deliver changes in intrathoracic pressure and tidal volume. Indeed, disease severity correlates negatively with respiratory muscle function (Terzano et al, 2008). Furthermore, hyperinflation leads to changes in chest wall geometry, inducing functional weakening of the accessory inspiratory muscles, which also contributes to a global reduction in the ability of the respiratory pump to generate inspiratory pressure (De Troyer & Wilson, 2009).
Much has been made in recent years of the adaptations that occur within the inspiratory muscles in response to the mechanical changes and increased physical demands described above. The chronically hyperinflated, flattened state of the diaphragm in COPD appears to lead to shortening of the total diaphragm length by around 15% to 25%, depending upon whether this is assessed at functional residual capacity FRC or residual volume (RV) respectively (McKenzie et al, 2009). This adaptation reduces the ability of the diaphragm to shorten during contraction, and thus limits its ability to generate inspiratory flow. However, the adaptations in diaphragm geometry and length appear to have some functional benefits in terms of maintaining its ability to deliver volume excursion, as well as its pressure-generating capacity (McKenzie et al, 2009). In respect of the latter, at equivalent absolute lung volumes the diaphragm pressure-generating capacity of patients with COPD is equal, or superior, to that of control participants (Similowski et al, 1991). However, despite this, the ability of the diaphragm to generate changes in volume at high lung volumes is diminished (McKenzie et al, 2009). It is important to keep in mind that diaphragm function at the same relative lung volumes is impaired in patients with COPD (see above), and that they have a reduced reserve capacity for volume and flow generation.
Change in diaphragm length is not the only chronic adaptation to hyperinflation and chronic inspiratory loading in patients with COPD. There are also changes in diaphragm biochemistry that appear to result from chronic loading (Levine et al, 1997; Ottenheijm et al, 2005). The healthy diaphragm is composed predominantly of two types of muscles fibres: one with high endurance but low power (type I, 45%), the other with low endurance but high power (type II, 55%). Patients with long-standing COPD have an abnormally high proportion of the former (type I 64%, type II 36%), which is an adaptive response to continuous inspiratory muscle loading (Levine et al, 1997).
Studies of the functional properties of the COPD-adapted diaphragm in vitro indicate that the fibres have a smaller cross-sectional area, contain less contractile protein and generate lower forces than those from patients without COPD (Ottenheijm et al, 2005). The dynamic properties of the contractile machinery of the COPD-adapted fibres are also impaired; the fibres appear to be less sensitive to calcium and show slower rates of myosin to actin attachment / detachment (Ottenheijm et al, 2005). Thus there is not only a loss of contractile protein; the protein that remains is also dysfunctional.
On the face of it, a shift towards an endurance-trained phenotype might be considered a positive adaptation; indeed it is cited as a reason for the futility of specific inspiratory muscle training (Polkey et al, 2011). However, it has been suggested that the increase in the proportion of type I fibres might, at least in part, explain the reduction in force-generating capacity (Clanton & Levine, 2009). Thus, depending upon the specific demands placed upon the inspiratory muscles, this adaptation can be either advantageous or disadvantageous. For example, it is advantageous for prolonged, low-intensity work, but disadvantageous for short, high-intensity work. The former is encountered at rest, whereas the latter is encountered during exercise. The diaphragm in patients with COPD therefore appears to be well adapted to generating low flow rates for long periods of time, but this adaptation robs them of the ability to generate the high pressures and flow rates required during exercise.
This suggestion is confirmed by studies of the in vivo strength and endurance of the inspiratory muscles of patients with COPD. For example, compared with control individuals, evoked diaphragm twitch pressure, maximal inspiratory pressure and a measure of endurance during inspiratory loading were all lower in patients with COPD (Barreiro et al, 2005). Furthermore, impairments were proportional to the severity of disease, despite the fact that a concomitant increase in type I fibres, and decrease in capillary to fibre ratio, were also proportional to disease severity. Thus, the shift towards a more endurance-trained phenotype reduced strength and did not appear to protect the inspiratory muscles from global fatigue under conditions of inspiratory loading (Barreiro et al, 2005). This is probably because weaker muscles must operate at a greater proportion of their maximum capacity, which predisposes them to fatigue.
Notwithstanding this apparent predisposition to fatigue, studies have so far failed to demonstrate evidence of exercise-induced contractile fatigue of the diaphragm in patients with COPD using low-frequency phrenic nerve stimulation (Polkey et al, 1995; Mador et al, 2000a; Mador et al, 2000b). However, this finding should not be misinterpreted to indicate that the inspiratory muscles are working within the limits of their capacity to deliver ![]() E, or that they do not impose any limitation upon exercise tolerance. The latter issue will be explored in greater detail in the section ‘Respiratory muscle involvement in exercise limitation’, but in the meantime it is noteworthy that studies where COPD patients walk (Kyroussis et al, 1996) or cycle (Yan et al, 1997) to the limit of tolerance have found a predominance of the rib cage muscle contribution to breathing. By measuring the rate of relaxation of the inspiratory muscles following a sniff effort, it is possible to detect the presence of global inspiratory muscle fatigue. Using this technique, it has been shown that, in patients who walk to the limit of tolerance, there is a slowing of the relaxation rate of oesophageal sniff pressure without any change in diaphragm twitch pressure, which is suggestive of accessory inspiratory muscle fatigue (Kyroussis et al, 1996). Furthermore, there does appear to be a subgroup of COPD patients who display diaphragm fatigue post-exercise (see below) (Hopkinson et al, 2010).
E, or that they do not impose any limitation upon exercise tolerance. The latter issue will be explored in greater detail in the section ‘Respiratory muscle involvement in exercise limitation’, but in the meantime it is noteworthy that studies where COPD patients walk (Kyroussis et al, 1996) or cycle (Yan et al, 1997) to the limit of tolerance have found a predominance of the rib cage muscle contribution to breathing. By measuring the rate of relaxation of the inspiratory muscles following a sniff effort, it is possible to detect the presence of global inspiratory muscle fatigue. Using this technique, it has been shown that, in patients who walk to the limit of tolerance, there is a slowing of the relaxation rate of oesophageal sniff pressure without any change in diaphragm twitch pressure, which is suggestive of accessory inspiratory muscle fatigue (Kyroussis et al, 1996). Furthermore, there does appear to be a subgroup of COPD patients who display diaphragm fatigue post-exercise (see below) (Hopkinson et al, 2010).
Finally, this section would be incomplete without mentioning the expiratory muscles, as well as contextualizing the changes in muscle function induced by COPD. As has already been alluded to, there is generalized muscle weakness, which also affects the expiratory muscles (Gosselink et al, 2000). In COPD patients the voluntary force-generating capacity of the expiratory muscles (maximal expiratory pressure: MEP) is ~ 30% lower than in healthy elderly people (Gosselink et al, 2000). This compares with differences in maximal inspiratory pressure (MIP), handgrip and quadriceps strength of ~ 40%, ~ 20% and 25%, respectively (Gosselink et al, 2000). The slightly larger effect of COPD upon MIP than MEP is most likely a manifestation of the additional influence of secondary weakness, due to the effects of hyperinflation (Gosselink et al, 2000). A recent study examined the influence of symptom limited cycling upon non-voluntary measures of expiratory and inspiratory muscle strength in patients with COPD; a significant exercise-induced fatigue of the abdominal muscles (7.2% fall in twitch gastric pressure) was found, but no change in diaphragm function (Hopkinson et al, 2010). Interestingly, only around one-third of the group exhibited expiratory muscle fatigue (twitch gastric pressure, 21%), and this subgroup also exhibited a significant fall in twitch diaphragm pressure (7.9%). The non-fatiguers exhibited no change in twitch gastric pressure, but a 7.7% increase in twitch diaphragm pressure. Unfortunately, the group was not subdivided to examine the diaphragm fatiguers in more detail. These data suggest that: (1) there is both inspiratory and expiratory muscle overload in at least some patients with COPD, and (2) diaphragm fatigue may be masked by lack of reliability in baseline measurements of twitch diaphragm pressure.
Patients with COPD also experience an increase in the demand for inspiratory muscle work, which arises from an elevated demand for minute ventilation (![]() E), especially during exercise. Ventilation/perfusion mismatching and a higher than normal ratio of dead space to tidal volume (VD / VT) both necessitate an increase in
E), especially during exercise. Ventilation/perfusion mismatching and a higher than normal ratio of dead space to tidal volume (VD / VT) both necessitate an increase in ![]() E in order to minimize changes in blood gases, but hypoxaemia is nevertheless a common finding. Furthermore, patients with COPD also have poor aerobic fitness, which increases the ventilatory demand of exercise (Casaburi et al, 1991), and thus increases inspiratory muscle work still further. Needless to say, these increased ventilatory flow requirements also exacerbate hyperinflation (Somfay et al, 2002).
E in order to minimize changes in blood gases, but hypoxaemia is nevertheless a common finding. Furthermore, patients with COPD also have poor aerobic fitness, which increases the ventilatory demand of exercise (Casaburi et al, 1991), and thus increases inspiratory muscle work still further. Needless to say, these increased ventilatory flow requirements also exacerbate hyperinflation (Somfay et al, 2002).
In summary, patients with COPD have a dramatically increased demand for inspiratory muscle work, but a reduced capacity to supply this demand due to muscle dysfunction. In other words, the demand / capacity relationship is stacked in completely the wrong direction. In the section ‘Respiratory muscle involvement in exercise limitation’, respiratory muscle-induced limitations to exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with COPD.
Asthma
The mechanical abnormalities in patients with asthma mimic closely those described in COPD; however, there are important differences. For example, there is less reduction in static lung recoil pressure and more widespread intrathoracic airway narrowing in asthma (Pride & Macklem, 1986). In addition, the increased airway collapsibility in patients with COPD is not seen in asthmatics. Furthermore, the reversible nature of airways obstruction in asthma results in relatively short-lived periods of stress upon the inspiratory muscles. The latter means that patients with asthma do not show the same changes in inspiratory muscle length or fibre composition that are expressed in patients with COPD (see above).
There is no clear consensus regarding the presence of primary weakness of the inspiratory muscles in patients with asthma compared with healthy people, as no biopsy data exists. However, the finding that steroid-dependent patients receiving oral corticosteroids show lower inspiratory muscle strength, but similar severity of hyperinflation, suggests that there may be myopathy in steroid-dependent patients with asthma (Akkoca et al, 1999). Generally, respiratory muscle strength and endurance are relatively normal in patients with stable asthma (Hill, 1991).
However, it is accepted universally that bronchoconstriction-induced hyperinflation is associated with secondary weakness of the inspiratory muscles (Fig. 3.1 inset) (Weiner et al, 1990; Perez et al, 1996; Akkoca et al, 1999; Stell et al, 2001; Weiner et al, 2002). As is the case in COPD, the major mechanical consequences of airway narrowing are increased flow resistive work, increased elastic work and PEEPi (resulting from dynamic lung hyperinflation), as well as reduced dynamic lung compliance (Martin et al, 1980; Lougheed et al, 1995). In a study comparing inspiratory muscle function of patients with COPD and asthma, with equivalent severity of hyperinflation, endurance was impaired to a greater degree in patients with asthma (Perez et al, 1996). Interestingly, strength was lower in the COPD patients compared with those with asthma. These data suggest that some of the structural and biochemical adaptations that occur in response to chronic loading in COPD are absent in patients with asthma. Thus, where airway obstruction is present, patients with asthma experience the same acute functional defect in their pulmonary function as those with COPD. However, the reversible nature of the airway obstruction may place patients with asthma at a functional disadvantage, and thus greater vulnerability to functional overload.
In a study of histamine-induced bronchoconstriction (FEV1 49% of baseline), the inspiratory work was found to increase 11-fold, 69% of the increase being due to the elastic component of the work of breathing (Martin et al, 1983). In addition, there also appears to be a prolonged activation of inspiratory muscles during exhalation in the presence of bronchoconstriction-induced hyperinflation (Muller et al, 1980; Muller et al, 1981), which suggests that the work of the total inspiratory muscles may be increased to an even greater extent than inspiratory work alone indicates.
The interrelationship between bronchoconstriction, hyperinflation and dyspnoea has also been studied. Multiple regression analysis indicates that, during methacholine-induced bronchoconstriction, change in inspiratory capacity (an index of dynamic hyperinflation) was the most powerful predictor of dyspnoea during bronchoconstriction – accounting for 74% of the variance in the perceptual rating (Lougheed et al, 1993). These observations are supported by more recent evidence confirming that hyperinflation is a major determinant of dyspnoea in patients with asthma (Martinez-Moragon et al, 2003).
As is the case in COPD, the mechanical changes associated with bronchoconstriction most likely increase the intensity of dyspnoea via their effect upon the magnitude of inspiratory neural drive (see Ch. 1). There is experimental support for this suggestion; Bellofiore et al (1996) found that the strongest determinant of dyspnoea during methacholine-induced bronchoconstriction was inspiratory neural drive (P0.1, mouth occlusion pressure), which explained 82% of the total variance in dyspnoea. More recently, Binks et al (2002) reported that institution of mechanical ventilation during methacholine-induced bronchoconstriction and hyperinflation significantly reduced ratings of ‘effort to breathe’ in people with mild asthma. Furthermore, it has also been shown that gender differences in inspiratory muscle strength may underpin differences in dyspnoea perception, quality of life and consumption of β2-agonist medication (Weiner et al, 2002). These data, along with data from inspiratory muscle training studies (see Ch. 4), support the notion that inspiratory muscle strength, and hence the relative intensity of inspiratory muscle work, makes a fundamental contribution to dyspnoea in people with asthma.
Because exercise is a trigger for asthma in around 90% of people with asthma (Wilkerson, 1998) there is an understandable anxiety regarding exercise that might translate into avoidance of physical activity, and poor aerobic fitness (Welsh et al, 2004). However, there remains no clear consensus regarding levels of physical activity and fitness, especially in children with asthma (Wilkerson, 1998), though there is some evidence to suggest that the aerobic fitness of adults with asthma is generally low (Satta, 2000). Thus, poor aerobic conditioning may exacerbate hyperinflation-related increases in the work of breathing during exercise by increasing the ventilatory requirement and exacerbating hyperinflation.
In summary, patients with asthma have an increased demand for inspiratory muscle work, which is proportional to the severity of their airway obstruction. It is not clear whether they have any primary weakness of their inspiratory muscles, but there is evidence of steroid-induced myopathy of the inspiratory muscles in steroid-dependent asthma. Furthermore, secondary weakness due to the influence of hyperinflation is well established, and linked strongly to dyspnoea. In the section ‘Respiratory muscle involvement in exercise limitation’, respiratory muscle-induced limitations to exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with asthma.
Bronchiectasis
Bronchiectasis is a chronic lung disease that is not normally included within the umbrella of COPD, but which overlaps with it (Neves et al, 2011); indeed one study found that 50% of patients with COPD also had bronchiectasis (Patel et al, 2004). It is characterized by irreversible widening of the medium-sized airways accompanied by inflammation, chronic infection and destruction of the bronchial walls (Neves et al, 2011). Both the pathology and the functional manifestations of bronchiectasis have similarities with those of COPD, including inflammatory cell profiles, protease release and consequent airway obstruction (Neves et al, 2011). In both conditions, these factors lead to detrimental changes in breathing mechanics, attendant exertional dyspnoea and exercise intolerance. Symptomology is also similar to COPD – including cough, sputum production and wheeze (Neves et al, 2011). Expiratory flow limitation (identified using the negative expiratory pressure technique) is present at rest in 39% of patients with bronchiectasis, which is a lower prevalence than in patients with COPD (Koulouris et al, 2003). The explanation for the latter finding may be that around half of patients had both obstructive and restrictive defects, i.e., restriction acted as a confounding influence; the presence of flow limitation was correlated with the MRC dyspnoea score, which in turn was correlated with exercise tolerance (Koulouris et al, 2003). Thus, the mechanical changes associated with bronchiectasis increase the demand for inspiratory muscle work, which is manifested symptomatically as exertional dyspnoea.
Compared with healthy people of a similar age, patients with moderate-to-severe bronchiectasis exhibit lower maximal inspiratory and expiratory muscle strength (around 20% and 40% lower, respectively) (Newall et al, 2005; Moran et al, 2010). The origin of this weakness is unclear, but is most likely due to a combination of primary weakness and functional weakness due to hyperinflation. Thus, in common with patients with COPD, patients with bronchiectasis have an imbalance in the demand / capacity relationship of the respiratory muscles. This imbalance will also be considered in the section ‘Respiratory muscle involvement in exercise limitation’, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with bronchiectasis.
Cystic fibrosis
Respiratory failure is the most common cause of death in patients with cystic fibrosis (CF) (Taylor-Cousar, 2009), and dyspnoea is one of their main complaints (Leroy et al, 2011); it has also been suggested that the deterioration of lung function in patients with CF have is insufficient to explain their exertional dyspnoea. Patients with CF have an elevated work of breathing (Dunnink et al, 2009), and this has been identified as an important contributor to dyspnoea (Leroy et al, 2011). There appears to be no evidence of inspiratory muscle weakness in patients with CF; indeed, some authors have reported that patients with CF have superior strength (Dufresne et al, 2009; Dunnink et al, 2009) and diaphragm thickness (Dufresne et al, 2009). The elevated airway resistance of patients with CF appears to contribute to their diaphragm hypertrophy (Dufresne et al, 2009). However, patients with the lowest fat-free mass exhibit a loss of diaphragm thickness (Ionescu et al, 1998; Enright et al, 2007). Furthermore, although indices of inspiratory muscle strength have been found to be normal or superior in patients with CF, loss of maximal inspiratory muscle work capacity has been reported (Ionescu et al, 1998; Enright et al, 2007), suggesting that there is a deterioration in the metabolic properties of the inspiratory muscles. This finding is suggestive of an imbalance between demand and capacity since the preservation of inspiratory muscle strength is accompanied by an increased demand for inspiratory muscle work, and dyspnoea. The fact that respiratory failure is the primary cause of death highlights the important influence of the imbalance between demand and capacity. This will also be considered in the section ‘Respiratory muscle involvement in exercise limitation’, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with CF.
Restrictive chest wall disorders
Conditions such as kyphoscoliosis, fibrothorax, thoracoplasty, flail chest and ankylosing spondylitis all induce chest wall restriction, creating a restrictive pulmonary defect in which total respiratory system elastance and resistance are elevated (Donath & Miller, 2009). In the case of severe kyphosis and / or scoliosis, thoracic volume may also be reduced by collapse of the vertebral column and the cranial displacement of the abdominal contents. As a consequence, breathing pattern tends to be rapid and shallow, creating a higher than normal ratio of dead space to tidal volume (VD / VT) ratio and necessitating an increase in ![]() E. This exacerbates the already elevated work of inhalation (Donath & Miller, 2009), and attendant dyspnoea. Furthermore, inspiratory muscle function also tends to be impaired (Lisboa et al, 1985; Cejudo et al, 2009), owing to changes in chest wall and diaphragm configuration. In kyphoscoliosis, inspiratory muscle strength has been shown to correlate with forced vital capacity (FVC), as well as to arterial blood gases, such that weakest patients exhibited the worst FVC and blood gases (Lisboa et al, 1985). Ultimately, the outcome of these conditions can be respiratory failure and the requirement for mechanical ventilation. The imbalance in the demand / capacity relationship of the respiratory muscles will also be considered in the section ‘Respiratory muscle involvement in exercise limitation’. See Chapter 4 for a description of the evidence supporting breathing exercises.
E. This exacerbates the already elevated work of inhalation (Donath & Miller, 2009), and attendant dyspnoea. Furthermore, inspiratory muscle function also tends to be impaired (Lisboa et al, 1985; Cejudo et al, 2009), owing to changes in chest wall and diaphragm configuration. In kyphoscoliosis, inspiratory muscle strength has been shown to correlate with forced vital capacity (FVC), as well as to arterial blood gases, such that weakest patients exhibited the worst FVC and blood gases (Lisboa et al, 1985). Ultimately, the outcome of these conditions can be respiratory failure and the requirement for mechanical ventilation. The imbalance in the demand / capacity relationship of the respiratory muscles will also be considered in the section ‘Respiratory muscle involvement in exercise limitation’. See Chapter 4 for a description of the evidence supporting breathing exercises.
Interstitial lung disease (ILD) is an umbrella term for a group of lung disorders that share a number of pathophysiological characteristics and clinical features. The principal feature of ILD is exercise intolerance due to exertional dyspnoea and perceptions of fatigue. Exercise intolerance is correlated with quality of life (Holland, 2010), which makes it an important therapeutic target.
The reduced lung compliance in ILD leads to impairment of vital capacity, and a rapid and shallow breathing pattern that worsens during exercise (Javaheri & Sicilian, 1992). This pattern exacerbates the existing ventilation / perfusion (![]() /
/ ![]() ) mismatch, due to its effect upon the VD / VT ratio. There is also an impairment of diffusing capacity, and the combination with
) mismatch, due to its effect upon the VD / VT ratio. There is also an impairment of diffusing capacity, and the combination with ![]() /
/ ![]() mismatching can precipitate substantial arterial desaturation (Miki et al, 2003). These changes also increase the ventilatory demand of exercise and hence the work of breathing.
mismatching can precipitate substantial arterial desaturation (Miki et al, 2003). These changes also increase the ventilatory demand of exercise and hence the work of breathing.
Sarcoidosis involves multiple organs, but pulmonary manifestations typically predominate (Lynch et al, 2007) in the form of an ILD. Dyspnoea is the most common presentation in patients with early to moderately advanced disease (Baydur et al, 2001). Sarcoidosis is associated with reduced inspiratory and expiratory muscle strength (~ 20% reduction), as well as impaired endurance (Wirnsberger et al, 1997; Baydur et al, 2001; Spruit et al, 2005), and respiratory muscle function correlates more closely with dyspnoea during activities of daily living than pulmonary function (Baydur et al, 2001); indeed dyspnoea can be present in the absence of any lung function defects (Baydur et al, 2001). The underlying mechanisms for respiratory muscle dysfunction in sarcoidosis are unclear, but two case reports indicate that granulomatous involvement of respiratory muscles is present (Dewberry et al, 1993; Pringle & Dewar, 1997). At the time of writing there have been no studies of respiratory muscle training in patients with sarcoidosis or other ILD.
Chronic heart failure and pulmonary hypertension
Patients with chronic heart failure (CHF) present with dyspnoea, exercise intolerance and fatigue. Chronic heart failure is a complex condition that generates a number of interrelated pathophysiological changes that affect skeletal muscle, the vasculature, neurohormonal systems and the lungs (Brubaker, 1997).
Inspiratory muscle dysfunction has not been assessed as widely or with the same rigour in CHF as in COPD. For example, there are no biopsy studies of diaphragm composition, and only one study has examined diaphragm twitch pressure (Hughes et al, 1999). Notwithstanding this, the evidence of inspiratory muscle weakness is consistent and compelling (Ribeiro et al, 2009). It has been suggested that inspiratory muscle weakness may be part of the generalized atrophy that is common in CHF, but there is some evidence that there may be selective weakness of the inspiratory muscles (Ribeiro et al, 2009). Indeed, inspiratory muscle strength has been shown to have prognostic value (Frankenstein et al, 2008, 2009), which underscores its importance. Furthermore, inspiratory muscle weakness is correlated with a number of indices of haemodynamic dysfunction, including cardiac output and the severity of pulmonary hypertension (Filusch et al, 2011).
Patients with CHF tend to adopt a rapid, shallow and constrained breathing pattern during exercise (Johnson et al, 2000). This appears to be an adaptive response to changes in the demand / capacity relationship of the inspiratory muscles. Lung compliance is reduced by pulmonary oedema and pulmonary fibrosis (Wright et al, 1990), which increases the work of breathing (Cross et al, 2012). An interesting feature of the rapid, shallow breathing pattern is that it coexists with expiratory flow limitation and a reduction in end-expiratory lung volume. The result is an increase in both the elastic and resistive work of breathing, the latter being present during both phases of respiration, whilst the former is seen only during inspiration (Cross et al, 2012). Unlike patients with COPD and asthma, patients with CHF do not hyperinflate in order to decrease their expiratory flow limitation (Johnson et al, 2000). Instead, unpleasant breathing sensations are minimized by adopting a rapid, shallow breathing pattern. This strategy suggests that the sensations associated with hyperinflation are more unpleasant than those associated with expiratory flow limitation and rapid, shallow breathing. This is entirely reasonable, given that hyperinflation in the presence of pulmonary oedema and fibrosis would increase inspiratory elastic work considerably (Cross et al, 2012). The mechanisms underlying the greater resistive work of breathing in CHF are uncertain, but may be related to worsening of pulmonary congestions and / or bronchoconstriction during exercise (Cross et al, 2012).
There are also a number of abnormalities that increase the ventilatory requirement of exercise in CHF, and thus increase the demands imposed upon the respiratory muscles. For example, diffusion impairment is present in 67% of patients with severe CHF (Wright et al, 1990). This may be due to pulmonary fibrosis, but may also be due to the influence of an impaired cardiac output upon ventilation/perfusion mismatching (Lewis et al, 1996), which elevates the physiological dead space. Furthermore, rapid, shallow breathing increases dead space ventilation further, because it generates a higher than normal ratio of dead space to tidal volume (VD / VT). Higher dead space necessitates an increase in ![]() E in order to minimize changes in blood gases. A further corollary of rapid, shallow breathing is that the higher inspiratory flow rate increases the relative functional demands upon the inspiratory muscles, which must operate on a weaker part of their force–velocity relationship (see Ch. 4, Fig. 4.1).
E in order to minimize changes in blood gases. A further corollary of rapid, shallow breathing is that the higher inspiratory flow rate increases the relative functional demands upon the inspiratory muscles, which must operate on a weaker part of their force–velocity relationship (see Ch. 4, Fig. 4.1).
Elevated peripheral chemoreflex sensitivity is found in as many as 40% of patients with CHF, and may contribute to the exaggerated exercise hyperpnoea, as well as sympathoexcitation (Chua et al, 1997). Recently, it was found that peripheral chemoreflex sensitivity to carbon dioxide is significantly higher in patients with CHF who have inspiratory muscle weakness than in those who do not (Callegaro et al, 2010). The study authors hypothesized that the elevated chemoreflex sensitivity was secondary to the sympathoexcitation resulting from metaboreflex activation in weakened / fatigued inspiratory muscles. This is consistent with the finding that ventilatory and cardiovascular responses to locomotor muscle metaboreflex activation are increased in patients with CHF (Piepoli et al, 1996). Thus, exaggerated responses to chemoreflex and metaboreflex stimulation during exercise most likely conspire to exacerbate an already elevated ventilatory demand.
For reasons that are not yet fully understood, MIP is an independent risk factor for myocardial infarction and cardiovascular disease death (van der Palen et al, 2004). One study has also shown that patient survival was lower in those patients with low MIP (Meyer et al, 2000).
Finally, pulmonary arterial hypertension (PAH) is worthy of mention at this point; the condition is associated with heart failure, but may also be idiopathic. The symptomatology and respiratory manifestations of PAH are similar to those of CHF, including respiratory muscle weakness (Meyer et al, 2005). Furthermore, there is evidence that inspiratory muscle strength may influence exercise tolerance in patients with PAH (Kabitz et al, 2008a).
Thus patients with CHF and / or PAH have an increased demand for inspiratory muscle work and a reduced capacity to supply this demand due to muscle dysfunction. In the section ‘Respiratory muscle involvement in exercise limitation’ the implications of this in the context of respiratory muscle-induced limitations to exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with CHF.
Neurological and neuromuscular disease
Spinal cord injury
Respiratory complications remain a major cause of morbidity and mortality in people with spinal cord injury (SCI) (Schilero et al, 2009), the underlying cause for these complications is poor cough function, which leads to mucus retention, atelectasis and infections (Schilero et al, 2009). The extent and severity of respiratory system compromise following SCI depend upon a number of factors including the level of the lesion, the completeness of the lesion and the ensuing temporal adaptations to the lesion. Furthermore, there is an elevated prevalence of obstructive sleep apnoea (OSA) in people with high spinal cord lesions (see also the section on OSA below), which may precipitate an increase in cardiovascular disease risk (Schilero et al, 2009).
Figure 3.2 summarizes the spinal innervation levels of the respiratory muscles, as well as indicating the distinctions between paraplegia and tetraplegia. Lesions above the level of the phrenic motor neurons (C3–C5) induce paralysis of all respiratory muscles, whereas in lower cervical lesions (C5–C8) the functions of the diaphragm and sternocleidomastoid are preserved. However, in the latter there is still a loss of inspiratory accessory muscle function (external intercostals and scalenes), as well as the primary muscles of expiration (internal intercostals and abdominals). Lesions in the thoracic region result in progressively less extensive denervation of the intercostal muscles as the level becomes more caudal, but any lesion above T6 results in complete loss of anterior abdominal wall innervation. Lesions between T6 and L3 result in partial denervation of the anterior abdominal wall, becoming less extensive at more caudal levels. Innervation of the posterior abdominal wall originates between T12 and L4, but these muscles make only a minor contribution to breathing.
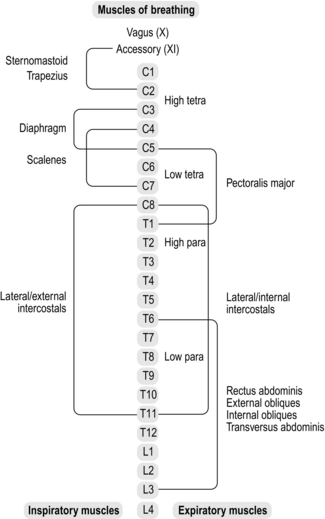
Figure 3.2 Levels of innervation of the respiratory muscles. Para = paraplegia; tetra = tetraplegia.
Maximal respiratory mouth pressures are correlated with the level of lesion for people with complete motor lesions, but not for those with incomplete lesions (Mateus et al, 2007). As one might expect, decrements in strength are greater for the expiratory muscles than for the inspiratory muscles, at equivalent lesion levels, the most severe compromise being for lesions at C4–C5 (maximal expiratory pressure 18% of predicted). In contrast, inspiratory muscle strength is least affected, and for lesions ranging from T1 to L6 is almost normal (85% predicted).
The loss of respiratory pressure-generating capacity has a predictable effect upon lung function, inducing a reduction in forced vital capacity (FVC) to between 49% (C4–C5) and 68% of predicted normal values (T7–L3) (Mateus et al, 2007). Forced expiratory volume in 1 second (FEV1) is also reduced, but this is not an indication of obstruction but rather a reflection of a lower inspiratory capacity (initiating the expiratory effort from a lower lung volume). Indeed, the ratio of FVC to FEV1 is supranormal (90–95%). Notwithstanding this, there is evidence of increased bronchomotor tone, as well as airway hyperresponsiveness, which has been attributed to a loss of sympathetic innervation to the lungs (Schilero et al, 2005).
Respiratory mechanics are altered considerably, especially in tetraplegia. The systems that normally operate to optimize pressure and volume changes during breathing are disrupted, leading to mechanical inefficiency. For example, the normally efficient action of the diaphragm is impaired by paradoxical movement of the rib cage. This paradox may be reduced with time (Scanlon et al, 1989); the improvement has been attributed to ankylosis of the rib cage joints and intercostal spasticity (Estenne & De Troyer, 1985), but the penalty for this is an increased oxygen cost of breathing (Silver, 1963), increased breathing effort perception, a rapid shallow breathing pattern, and possibly increased diaphragm fatigability (Hopman et al, 1997). The increase in abdominal compliance also impairs the efficiency of the diaphragm by reducing the stability of the visceral fulcrum, and inducing a longer resting length. The former also reduces expansion of the lower ribs, generating inhomogeneity of changes in pleural pressure and gas distribution (Estenne & De Troyer, 1985), which is exacerbated by paradoxical movement of the rib cage (Hiraizumi et al, 1986). The resulting ventilation / perfusion mismatching may contribute to inefficient gas exchange.
As one might expect, decrements in pulmonary function are most severe during the acute phase, with some recovery of function over the 12 months following injury. However, recovery shows large inter-individual variation, and has been attributed to improvements in respiratory muscle function and changes in rib cage stability (Schilero et al, 2009).
Respiratory symptoms are common in patients with SCI, with dyspnoea being the most prevalent complaint. Dyspnoea is present in 73% of people with a lesion at C5, but only 29% in those with a lesion below T8 (Spungen et al, 1997). Other symptoms appear to be related to cough and phlegm, which are present in about a quarter of people with SCI, and with no correlation to level of injury. Increasing abdominal compliance, by means of a strapping, in people with lesions between C5 and T6 has been found to reduce breathing effort perception, most likely because of a concomitant increase in diaphragm length and function (Hart et al, 2005).
The prevalence of OSA in patients with SCI is at least twice that observed in the general population, is most prevalent in those with a cervical SCI, and also in the acute phase following injury (Schilero et al, 2009). A number of putative mechanisms have been suggested to explain the high prevalence of OSA in people with SCI, including disruption of the normal coordination between upper airway and respiratory pump muscles, thickening of the oropharyngeal wall and increased adiposity of the neck leading to reduced upper airway patency (Schilero et al, 2009).
The role of the respiratory muscle denervation in exercise tolerance will also be considered in the section ‘Respiratory muscle involvement in exercise limitation’, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with SCI.
Other NMDs
Weakness of both inspiratory and expiratory muscles is common in NMD, and leads to a restrictive pattern of pulmonary dysfunction, especially in advanced disease (Gibson et al, 1977). Because physical activity is limited by generalized deterioration of muscle function, dyspnoea is not always present. However, ventilatory limitation due to respiratory muscle weakness may be exacerbated by disease-specific factors that elevate the ventilatory demand, such as an early onset of the anaerobic threshold, particularly where mitochondrial myopathy is present (Flaherty et al, 2001). In addition, the adoption of a rapid, shallow breathing pattern generates a higher than normal ratio of dead space to tidal volume (VD / VT), increasing the demand for minute ventilation (![]() E), and the associated work of breathing. There may also be ventilation / perfusion mismatching and impaired gas exchange (Rochester, 1993). In advanced disease, respiratory muscle weakness, muscle fibrosis and microatelectasis may lead to chronic hypoventilation and hypercapnia. Under these conditions, there is a high risk of inspiratory muscle fatigue in response to small changes in the requirement for inspiratory muscle work, e.g., in the event of pulmonary complications (Kang, 2006). A recent study found that in patients with ALS, a supine Borg score ≥ 3 was associated with impaired inspiratory muscle strength and a lower vital capacity. The authors suggested that this simple assessment might provide a useful test of inspiratory muscle weakness in ALS (Just et al, 2010). Furthermore, respiratory muscle strength correlates with capability of daily living in the self-care and social function domains of a quality of life questionnaire (PEDI) in children with cerebral palsy (Wang et al, 2012), and with physical functioning domains of a quality of life questionnaire (SF-36) in patients with myotonic dystrophy (Araujo et al, 2010). These findings suggest a link between respiratory muscle strength and quality of life in children and adults with NMD.
E), and the associated work of breathing. There may also be ventilation / perfusion mismatching and impaired gas exchange (Rochester, 1993). In advanced disease, respiratory muscle weakness, muscle fibrosis and microatelectasis may lead to chronic hypoventilation and hypercapnia. Under these conditions, there is a high risk of inspiratory muscle fatigue in response to small changes in the requirement for inspiratory muscle work, e.g., in the event of pulmonary complications (Kang, 2006). A recent study found that in patients with ALS, a supine Borg score ≥ 3 was associated with impaired inspiratory muscle strength and a lower vital capacity. The authors suggested that this simple assessment might provide a useful test of inspiratory muscle weakness in ALS (Just et al, 2010). Furthermore, respiratory muscle strength correlates with capability of daily living in the self-care and social function domains of a quality of life questionnaire (PEDI) in children with cerebral palsy (Wang et al, 2012), and with physical functioning domains of a quality of life questionnaire (SF-36) in patients with myotonic dystrophy (Araujo et al, 2010). These findings suggest a link between respiratory muscle strength and quality of life in children and adults with NMD.
Sleep-disordered breathing is also secondary to inspiratory muscle weakness via its influence upon vital capacity (Ragette et al, 2002). Furthermore, upper airway muscle involvement in NMD can result in obstructive respiratory events during sleep (Aboussouan, 2009). Aspiration and difficulties with swallowing are also related to the impairment of bulbar muscle function (Aboussouan, 2009). Poor cough function and respiratory muscle weakness conspire to make respiratory complications a leading cause of morbidity and mortality in NMD (Macklem, 1986).
Acute respiratory failure is a common complication of a number of acute onset neuromuscular conditions, such as Guillain–Barré syndrome, myasthenia gravis and polymyositis (Mehta, 2006), as well as in chronic conditions following development of respiratory complications. Multiple factors underlie the development of respiratory failure, but the principal contributors are weakness and fatigue of upper airway, inspiratory and expiratory muscles, as well as the influence that these impairments have upon cough efficacy and the development of infection (Mehta, 2006). See also the section ‘Mechanical ventilation’, below.
Thus, the picture in NMD is one of multifactorial defects in respiratory and upper airway function, and imbalance in the demand / capacity relationship of the respiratory muscles that can quickly result in respiratory failure (Macklem, 1986). In the section ‘Respiratory muscle involvement in exercise limitation’, the implications of these changes for exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with NMD.
Obesity
The influence of obesity upon respiratory muscle function stems primarily from the mechanical impedances imposed by fat deposition upon the movement of the chest wall and diaphragm (Salome et al, 2010). Fat deposited on the chest wall decreases respiratory system compliance, creating a restrictive pulmonary defect. Fat deposited within the abdominal cavity reduces its compliance and impedes diaphragm movement into the abdominal compartment. Respiratory system compliance of obese people is approximately half that of lean people, and reduces still further in obese people when supine (Naimark & Cherniack, 1960).
The effect of obesity upon lung volumes is primarily to reduce functional residual capacity (FRC) and end-expiratory lung volumes (EELV) (Babb et al, 2008b), owing to increased respiratory system recoil. This increases the likelihood of expiratory flow limitation (Ferretti et al, 2001). In addition, when breathing closer to residual volume, airway calibre is smaller and thus airway resistance is greater. For example, compared with overweight people (BMI 27 kg·m− 2), airway resistance was 56% greater in obese people (body mass index [BMI] 46 kg·m− 2); airway resistance was also correlated with the reduction in FRC (Zerah et al, 1993). Total lung capacity and residual volume tend to be preserved, but inspiratory reserve volume tends to increase and expiratory reserve volume to decrease (due to the reduction in EELV). However, in extreme obesity TLC may be impaired by the inability of the inspiratory muscles to overcome the increased compliance of the chest wall and abdominal compartment, or by a reduction in thoracic volume due to ingress of adipose tissue (Salome et al, 2010). Overall, the effects of obesity are to roughly double the work of breathing (Naimark & Cherniack, 1960; Pelosi et al, 1996; Kress et al, 1999), with most of the increase deriving from the increased elastic work (Pelosi et al, 1996).
The relative overloading of the respiratory pump in obesity is also reflected in a reduced maximum voluntary ventilation (MVV), the decline being greater with higher BMIs. However, this decline in MVV is greater than the declines in FEV1 and FVC would predict (Weiner et al, 1998), which points strongly to a deficit in the function of the inspiratory muscles. Airway function is impaired slightly, with FEV1 and FVC tending to decrease with increasing BMI (Salome et al, 2010). Since both indices decrease to the same extent, the impairment in FEV1 is most likely secondary to the decrease in FVC, and not to a direct effect of obesity upon airway diameter (Salome et al, 2010). Changes in breathing mechanics mean that obesity leads to a reduction in EELV during exercise, with the consequence that some expiratory flow limitation may result (Rubinstein et al, 1990).
Respiratory muscle strength and endurance appear to be well preserved in some obese adults (Yap et al, 1995; Weiner et al, 1998; Collet et al, 2007), but studies have reported a small (~ 10%) impairment of respiratory muscle strength and endurance (Weiner et al, 1998; Chlif et al, 2005). Interestingly, even in those with relatively well-preserved respiratory muscle function, weight loss following bariatric surgery improves inspiratory and expiratory muscle strength by around 20% (Weiner et al, 1998). One thing is clear: inspiratory muscle function is inversely related to BMI. A significant negative correlation has been observed by some investigators (Chlif et al, 2005), whilst others have noted that inspiratory muscle strength was slightly lower (~ 15%) in patients with a BMI > 49 kg·m− 2 than in those with a BMI < 49 kg·m− 2 (Collet et al, 2007).
Dyspnoea is a common complaint amongst obese individuals, both at rest and during exercise. This may be in part due to inspiratory muscle weakness (Chlif et al, 2007, 2009), but alterations in respiratory system mechanics also contribute. Breathing is associated with a rapid, shallow pattern, an increased ventilatory drive to the inspiratory muscles and an increased inspiratory muscle work (Chlif et al, 2007; Chlif et al, 2009). An increased oxygen cost of breathing has been implicated specifically in the dyspnoea associated with obesity (Babb et al, 2008a).
Another important factor to be borne in mind with regards to the influence of obesity upon breathing is the existence of co-morbidities. For example, it is increasingly common for obesity to be present with COPD (Franssen et al, 2008). There is also a well-established causal relationship between obesity and obstructive sleep apnoea (Schwartz et al, 2010), as well as hypoventilation syndrome (Anthony, 2008). Less well established, but an area of growing interest, is the apparent association between obesity and asthma, with some researchers suggesting that there may be a causal relationship between the two conditions (Sood, 2005), in which obesity is the antecedent (Ford, 2005). A putative underlying mechanism for the development of asthma, as well as the exacerbation of existing disease, is the production of pro-inflammatory cytokines by adipose tissue (Sood, 2010).
Thus, obese patients have an increased demand for inspiratory muscle work, which arises from complex changes in respiratory system mechanics. Furthermore, in those with inspiratory muscle weakness there is also a reduced capacity to supply this elevated demand. In the section ‘Respiratory muscle involvement in exercise limitation’, respiratory muscle-induced limitations to exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for obese people.
Ageing
The process of normal ageing is associated with a number of changes that affect breathing (Janssens et al, 1999). Thus deterioration in pulmonary mechanics, lung function, locomotor efficiency and respiratory muscle function, as well as remodelling of pulmonary vasculature, all impact upon the demand / capacity relationship of the respiratory muscles.
The senescent changes to the pulmonary system have been dubbed ‘senile emphysema’ (Janssens et al, 1999) and are present from the age of 50 years, becoming most apparent at around 80 years (Britto et al, 2009). The most important of these changes are a decrease in the static recoil of the lung, a decrease in chest wall compliance and a reduction in the strength of the respiratory muscles (Janssens et al, 1999). Accordingly, many of the factors that increase the demand for inspiratory muscle pressure generation in COPD are also common to normal ageing. These include dynamic hyperinflation (Deruelle et al, 2008), and an increase in mechanical ventilatory constraints during exercise (DeLorey & Babb, 1999). Older people also adopt a rapid, shallow breathing pattern, and exhibit a greater dead space to tidal volume ratio (VD / VT), which necessitates an increase in ![]() E (DeLorey & Babb, 1999). There is also remodelling of the pulmonary vasculature, leading to increased vascular stiffness, resistance and pressure (Taylor & Johnson, 2010). These changes reduce pulmonary capillary blood volume and increase heterogeneity in the distribution of ventilation and perfusion. The resultant reduction in membrane diffusing capacity is consistent with a reduction in alveolar–capillary surface area (Taylor & Johnson, 2010). These changes make a small additional contribution to the ventilatory demand. In addition, the mechanical efficiency of exercise appears to be lower in older people (McConnell & Davies, 1992).
E (DeLorey & Babb, 1999). There is also remodelling of the pulmonary vasculature, leading to increased vascular stiffness, resistance and pressure (Taylor & Johnson, 2010). These changes reduce pulmonary capillary blood volume and increase heterogeneity in the distribution of ventilation and perfusion. The resultant reduction in membrane diffusing capacity is consistent with a reduction in alveolar–capillary surface area (Taylor & Johnson, 2010). These changes make a small additional contribution to the ventilatory demand. In addition, the mechanical efficiency of exercise appears to be lower in older people (McConnell & Davies, 1992).
The term sarcopenia first appeared in the literature in the early 1990s to describe the age-related loss of muscle mass (Rogers & Evans, 1993). Respiratory muscles are also affected by this process, and their strength is correspondingly lower in older people (McConnell & Copestake, 1999); indeed, respiratory muscle strength is strongly and independently correlated with hand grip strength (Enright et al, 1994). Furthermore, respiratory muscle strength is also independently related to decline in mobility in older people (Buchman et al, 2008).
Finally, the influence of co-morbidities must also be borne in mind, since the majority of older people are not without disease. Accordingly, the age-related changes described above serve to exacerbate disease-related impairments. The picture in older people is therefore one of an emerging load / capacity imbalance within the respiratory muscles that worsens progressively with advancing age, and is exacerbated by chronic disease. In the section ‘Respiratory muscle involvement in exercise limitation’, the implications of these changes for exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for older people.
Miscellaneous conditions
The underlying cause of respiratory muscle weakness in the conditions described below is diverse, ranging from the existence of a ‘myopathic muscle milieu’ (e.g., corticosteroid treatment), to profound disuse (mechanical ventilation). Where applicable, the evidence supporting the application of specific respiratory muscle training to these conditions will be described in Chapter 4.
Diabetes
Type 1 and 2 diabetes are associated with inspiratory and expiratory muscle weakness (~ 20% and ~ 10% impairment, respectively) (Heimer et al, 1990; Kaminski et al, 2011); in type 1, there is also impaired inspiratory muscle endurance (Heimer et al, 1990), vital capacity and FEV1 (Innocenti et al, 1994). The reductions in lung volumes are at least partially explained by inspiratory muscle weakness (Wanke et al, 1991). However, loss of lung elasticity, and consequent airway collapse and obstruction, is also implicated (Goldman, 2003). The observation of a reduction in dynamic lung compliance is consistent with peripheral airway obstruction (Mancini et al, 1999). Biochemical changes in lung connective tissue have been suggested to underlie changes in elastic properties (Irfan et al, 2011). There is also a decrease in the pulmonary diffusing capacity, which may have its origins in pulmonary capillary damage induced by microvascular complications (Saler et al, 2009). Functionally, the structural changes to the lung parenchyma result in an elevated work of breathing (Wanke et al, 1992) and there is an increase in the magnitude of the ventilatory response to exercise, which is tachypnoeic in the presence of autonomic neuropathy (Tantucci et al, 1996). These factors most likely contribute to the greater intensity of dyspnoea during exercise (Wanke et al, 1992) and during hypoxia-induced hyperpnoea (Scano et al, 1999). Diabetic neuropathy has also been linked to inspiratory muscle weakness and autonomic dysfunction, as evidenced by a reduction in heart rate variability (Kaminski et al, 2011).
Putative underlying mechanisms for the inspiratory muscle weakness in patients with diabetes are divided broadly into two types: (1) biochemical and (2) neural. For example, inspiratory muscle strength is correlated with carnitine levels (Kilicli et al, 2010), which are lower in people with diabetes. In addition, there is evidence from rodent models of diabetes that the characteristics of resting membrane and action potentials are altered (van Lunteren & Moyer, 2003), and that responsiveness of the diaphragm to magnetic stimulation of the phrenic nerves is impaired in patients with diabetic polyneuropathy (Kabitz et al, 2008b). Impaired endurance of the inspiratory muscles may be explained by the many muscle metabolic abnormalities that arise because of insulin resistance and / or hyperglycaemia (Sun et al, 2008). In the section ‘Respiratory muscle involvement in exercise limitation’, the implications of these changes for exercise tolerance will be considered, and Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with diabetes.
Renal failure
Respiratory system involvement in renal failure is extremely complex (Prezant, 1990), deriving from both the disease and its treatment. It has been known for many years that uraemic patients possess impaired inspiratory muscle strength and a restrictive pulmonary defect (Gomez-Fernandez et al, 1984). The latter is most likely due to the effects of hypervolaemia, which induces pulmonary hypertension and oedema. Impairment of vital capacity is reversible with dialysis, implicating hypervolaemia as a major contributory factor (Kovelis et al, 2008). Since respiratory muscle strength does not appear to improve post-dialysis, primary weakness is implicated. Furthermore, patients who have been receiving dialysis for the longest showed the most impaired inspiratory muscle function (Kovelis et al, 2008). This supports the notion of progressive development of primary weakness (Bark et al, 1988; Karacan et al, 2006; Kovelis et al, 2008). For this reason, estimates of the magnitude of impairment differ between studies, ranging from deficits of ~ 40% and 50% for inspiratory and expiratory muscle strength respectively (Bark et al, 1988), to ~ 10% (Kovelis et al, 2008). Interestingly, respiratory muscle dysfunction is partially reversible following renal transplantation (Guleria et al, 2005). Chapter 4 will review the evidence supporting specific respiratory muscle training for patients with renal failure.
Cancer
One of the most common chronic symptoms in patients with cancer is exertional dyspnoea, which is present in up to 10% of survivors of childhood cancers and up to 70% of patients with advanced cancer (Travers et al, 2008). Generally, pulmonary function is relatively normal in patients with cancer (Travers et al, 2008), and there are no major mechanical abnormalities. However, there are exceptions, and pulmonary function may be impaired in specific cancers affecting the thorax (e.g., lung and breast), especially following locoregional adjuvant radiotherapy (Spyropoulou et al, 2009). There are many ways in which cancer and / or its treatment might cause dyspnoea, but one unifying mechanism that has been suggested to underlie exertional dyspnoea in patients with cancer is respiratory muscle weakness (Feathers et al, 2003; Travers et al, 2008). Since pulmonary function does not correlate with dyspnoea, inspiratory muscle weakness is likely to be an important contributor to the symptom (Travers et al, 2008). In the section ‘Respiratory muscle involvement in exercise limitation’, the implications of these changes for exercise tolerance will be considered. At the time of writing there have been no studies of respiratory muscle training in patients with cancer.
Anorexia nervosa
Anorexia nervosa is associated with generalized muscle wasting and specific weakness of the respiratory muscles (Birmingham & Tan, 2003; Gardini Gardenghi et al, 2009) including the diaphragm (Murciano et al, 1994). In addition, there is evidence of impaired spirometric function that is correlated with body mass (Ziora et al, 2008). Furthermore, malnourishment appears to induce changes to the lung parenchyma resulting in impaired diffusion capacity (Gardini Gardenghi et al, 2009) and / or emphysema-like changes to the lung structure (Coxson et al, 2004), as well as an increase in residual volume (Gonzalez-Moro et al, 2003). Functionally, there is impaired exercise tolerance (Biadi et al, 2001), perhaps due in part to dyspnoea (Birmingham & Tan, 2003). Case study evidence suggests that inspiratory muscle function may take longer to recover following refeeding than other muscles, leading to prolongation of dyspnoea symptoms and exercise intolerance (Birmingham & Tan, 2003).
The underlying causes for the spirometric changes are thought to be a combination of a restrictive defect caused by inspiratory muscle weakness (Ziora et al, 2008) and the effects of undernutrition on the lung parenchyma. Animal models of anorexia have demonstrated decreased production of lung surfactant (D’Amours et al, 1983), as well as the total protein, connective tissue and elastic content of the lungs of young animals (Sahebjami & MacGee, 1985), which is not completely reversible by refeeding (Sahebjami & Domino, 1992). In the section ‘Respiratory muscle involvement in exercise limitation’, the implications of these changes for exercise tolerance will be considered. At the time of writing there have been no studies of respiratory muscle training in patients with anorexia nervosa.
Myopathic pharmacological agents
The myopathic influence of orally administered corticosteroids was discussed briefly in relation to patients with COPD and asthma. Steroid-induced myopathy is a well-established phenomenon in patients receiving high doses of corticosteroids (Perkoff et al, 1959). The first study to examine the independent effects of costicosteroid treatment and disease progression demonstrated that, in non-respiratory patients, 1 to 1.5 mg·kg− 1 per day of prednisolone induced significant reductions in the strength (~ 30%) and endurance (~ 50%) of the inspiratory muscles over an 8-week treatment period (Weiner et al, 1993; Weiner et al, 1995). Although these changes show some reversal following cessation of treatment, function may take as long as 6 months to normalize (Weiner et al, 1993).
There have also been a number of case reports of colchicine-induced myopathy following prolonged treatment (Wilbur & Makowsky, 2004) including one report in which the predominant clinical feature was respiratory muscle weakness, as indicated by severe dyspnoea, orthopnoea, tachypnoea and thoracoabdominal paradox (Tanios et al, 2004). Cessation of treatment resulted in an improvement in respiratory muscle function, which more than doubled from pre-cessation levels of ~ 25–30 cmH2O (Tanios et al, 2004).
Most recently, statin-induced myopathy has come under scrutiny, as it is estimated that 5–10% of patients receiving statins develop myopathy (Rallidis et al, 2011). At least one case study report has demonstrated an association between respiratory symptoms, inspiratory muscle dysfunction and statin administration (Chatham et al, 2009). See Chapter 4 for a description of the evidence supporting specific inspiratory muscle training.
Surgery
Post-operative pulmonary complications (PPC) are common in patients undergoing cardiothoracic, abdominal and other major surgeries. Because of variations in both the nature of surgeries and the definition of PPC, estimates of the incidence vary from 2% to 40% (Canet & Mazo, 2010). The substantial contribution made by PCC to the morbidity and mortality associated with surgery and anaesthesia has led to interest in predicting those patients at risk of developing a PPC. Three main factors contribute to risk, and their interaction appears to determine its level: (1) general health status, (2) effects of anaesthesia and (3) surgical trauma (Canet & Mazo, 2010).
General health status has a predictable influence upon risk, especially where patients have pre-existing respiratory and cardiovascular dysfunction (Canet & Mazo, 2010). Anaesthesia induces a range of pre- and post-operative changes that increase the risk of PCC (Canet & Mazo, 2010). For example, atelectasis is universal, arising from physical compression of the lungs, absorption of alveolar air and impairment of surfactant function. These changes induce ventilation/perfusion mismatching, which increases dead space and hypoxaemia (Canet & Mazo, 2010). Post-operative drugs such as anaesthetics and analgesics also affect upper airway and accessory muscle function, increasing the risk of PCC (Canet & Mazo, 2010). As one might expect, the site of surgery has a potent influence upon the development of PPC. Predictably, thoracic and abdominal surgeries are associated with the highest risk of PPC (10–40%; Duggan & Kavanagh, 2010), and give rise to post-operative respiratory muscle dysfunction. The origin of the resulting muscle dysfunction is complex, but includes factors such as changes in thoracoabdominal mechanics and loss of muscular integrity (Siafakas et al, 1999). In addition, post-operative pain can limit respiratory movements, which can also be impaired by reflex inhibition of respiratory muscle activity, especially the diaphragm (Sharma et al, 1999). The latter arises because of feedback stimulated by mechanical disturbance of the viscera (Canet & Mazo, 2010). Finally, procedures lasting more than 3 hours have a higher risk of PCC (Duggan & Kavanagh, 2010), which may be partially due to the effects of inspiratory muscle inactivity during mechanical ventilation upon inspiratory muscle function (see the section ‘Mechanical ventilation’). See Chapter 4 for a description of the evidence supporting specific inspiratory muscle training for the prevention of PPC.
Mechanical ventilation
The primary reason for admission to intensive care is the need for mechanical ventilation, which imposes a considerable burden upon both patients and healthcare systems (Bissett et al, 2012). Mechanical ventilation is a double-edged sword for the respiratory muscles. On the one hand it can provide much needed rest for overloaded muscles, but on the other the imposed rest can lead to rapid atrophy and loss of respiratory muscle function (Petrof et al, 2010). The latter can lead to prolongation of mechanical ventilation, and difficulty weaning patients from the ventilator (Callahan, 2009). Weaning typically accounts for 40–50% of the total duration of mechanical ventilation and 30% of patients fail to wean at the first attempt (Moodie et al, 2011). Indeed, patients who experience weaning failure are characterized by their rapid, shallow breathing pattern and a diaphragm tension–time index (TTI) that is close to the threshold for fatigue (Karakurt et al, 2011); multiple logistic regression analysis with the weaning outcome as the dependent variable has revealed TTI, and the ratio of breathing frequency to VT, as significant predictors of weaning outcome (Vassilakopoulos et al, 1998). Patients who are weaned successfully from mechanical ventilation have been shown to possess higher MIP than those who do not (Epstein et al, 2002; Carlucci et al, 2009), and low MIP is an independent predictor of prolonged weaning (De Jonghe et al, 2007). However, a recent systematic review failed to find evidence that superior inspiratory muscle strength leads to a shorter duration of mechanical ventilation, improved weaning success or improved survival; the authors highlighted the need for further research (Moodie et al, 2011). It has been suggested that discrepancies relating to the influence of MIP upon these factors may reflect the inadequacy of MIP as a prognostic index of the respiratory muscle contribution to complex phenomena such as weaning (Bissett et al, 2012).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


