Consequently, it is likely that our evidence base to confirm or refute this hypothesis will consist of large bodies of observational data. Further registry data are now available, and their results and limitations are discussed below. In addition, some information can be gained from the results of other randomized controlled trials, which, although not designed or powered to look at neurological end points, do at least record them.
The Mechanisms of Periprocedural Stroke
If dedicated randomized data are unavailable, perhaps we should return to basic principles and look more closely at the pathophysiological mechanisms by which adverse neurological events occur during percutaneous coronary procedures. This might improve our comprehension of the potential issue and give us important clues as to which access route is preferable. At the same time, it might be possible to determine whether there is anything that we can measure to be used as a surrogate end point in a more manageable-sized study. Small studies have indeed been undertaken, employing surrogate markers to compare the risk of neurological events from the femoral and radial approaches, and these are discussed below.
There are several mechanisms by which procedure-related neurological complications may occur: air embolus, intracerebral bleeding due to antithrombotic treatment, periprocedural hypotension leading to watershed infarcts, and contrast-induced osmolar changes affecting the blood–brain barrier. The usual presumption for those events with persistent symptoms, however, is that some embolic material has become lodged in the distal cerebral vasculature. This material is often assumed to be thrombus or thrombus containing, and in some cases responds to thrombolytic therapy. Despite flushing and intensive anticoagulation, modern imaging modalities have demonstrated that thrombus can still form inside the catheter (Fig. 24.1).
Considering all these possible mechanisms together, an increased risk of neurological sequelae might be assumed from those procedures undertaken transradially during the operator’s learning curve. Such procedures tend to be longer and do involve more contrast injections and catheter exchanges, risking both air emboli and osmolar effects. With less experienced radial operators, catheters and wires in situ for longer periods might predispose to thrombus formation. In experienced hands or those who have been trained transradially from the outset, however, procedures are not longer than from the femoral approach and may often involve fewer catheter exchanges.
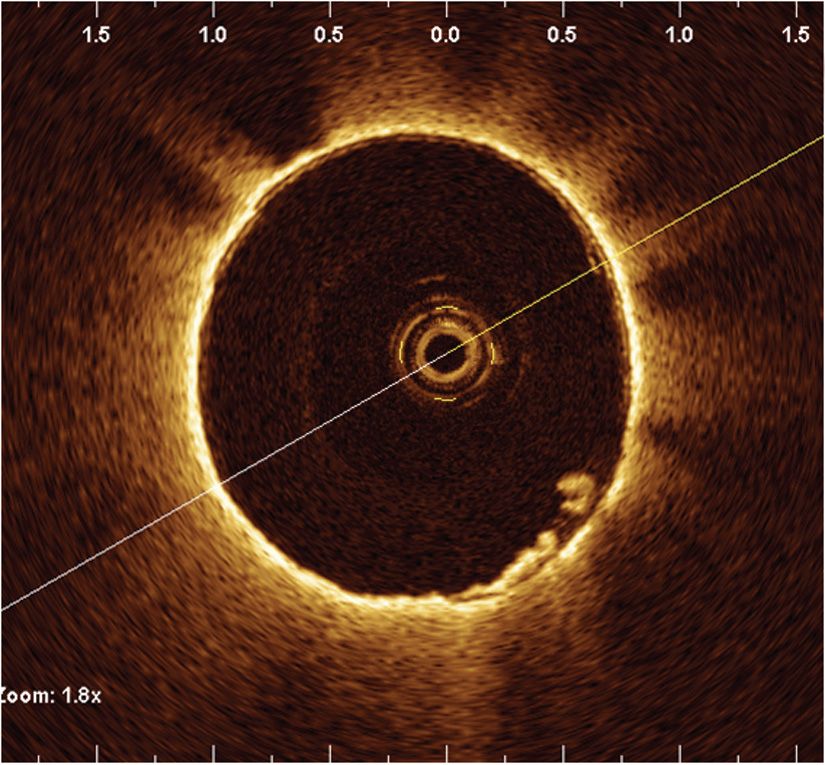
FIGURE 24-1 OCT evidence of adherent thrombus despite anticoagulation.
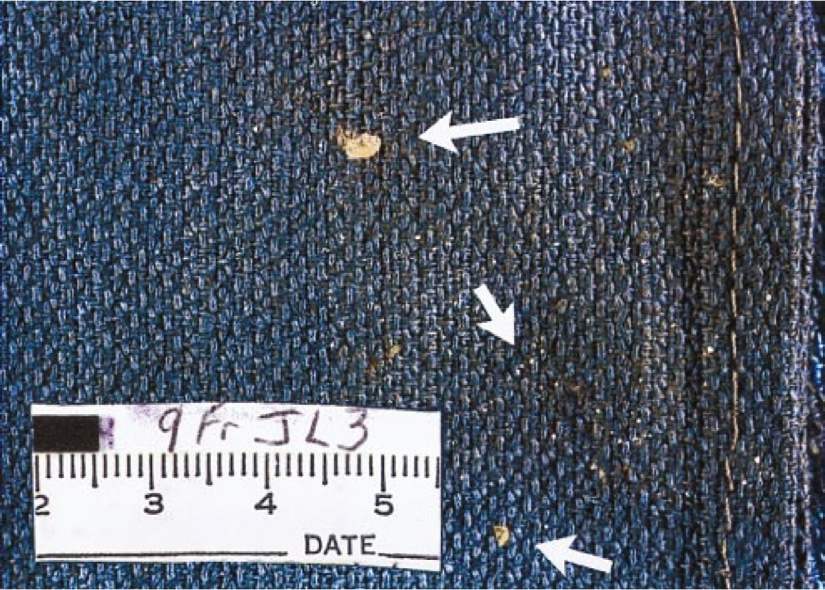
FIGURE 24-2 Debris from catheters. (From Keeley EC, Grines CL. Scraping of aortic debris by coronary guiding catheters: a prospective evaluation of 1,000 cases. J Am Coll Cardiol. 1998;32(7):1861–1865.)
In surgical patients after cardiopulmonary bypass, cholesterol emboli with varying amounts of platelets and fibrin are found in the smaller cerebral arteries postmortem. There are no data on the composition of retrieved embolic material post-PCI, but we have long since been aware of the risk of disrupting atherosclerotic material from the aortic or femoral artery wall with guidewires and catheters. This is a frequent event and is likely to be the predominant source of periprocedural emboli and, therefore, the biggest risk for neurological events (Fig. 24.2).3 The patient and procedural risk factors for stroke during catheterization also suggest that embolism of aortic atheroma is likely to be the predominant mechanism.4 Outside of the catheterization laboratory and despite anticoagulation, aortic atheroma is an independent risk factor for cryptogenic stroke,5,6 and patients known to be at highest risk of periprocedural stroke are those most likely to have aortic atheroma.4,7,8 In a study of patients undergoing both cardiac catheterization and transesophageal echocardiographies, the vast majority (93%) of patients with coronary disease also had aortic atheroma.9 The distribution of aortic atheroma in this study also provides an important clue as to where the risks lie (Fig. 24.3). The fact that the majority of atheroma and the more complex “high-risk” plaques are found in the descending aorta suggests that transradial access in which the descending aorta (and in the right radial approach, much of the arch) is avoided might, in fact, be substantially safer.
Studies Using Surrogate Markers
Already employed in studies of carotid endarterectomy and cardiac surgery, transcranial Doppler measurements confirm the systematic occurrence of cerebral microemboli during cardiac catheterization (Fig. 24.4). This noninvasive measurement has been proposed as a surrogate end point with which percutaneous coronary procedures and the risk of embolic sequelae can be compared. In the first catheter study to use transcranial Doppler, emboli counts per procedure were found to be proportionate to the number of times the aortic arch was crossed with a catheter.10 The emboli count also seemed to be related to the amount of atheroma found in the aortic arch on transesophageal echocardiography. This was a small study and certainly did not demonstrate that emboli counts were a good surrogate for clinical events, of which in fact there were none in the cohort studied.
In a subsequent study, transcranial Doppler measurements were examined alongside diffusion-weighted cerebral magnetic resonance imaging (MRI), which is currently the most sensitive tool available for early detection of cerebral infarction.11 An important revelation of this study was that the majority of transcranial Doppler signals detected are caused by microbubbles and only 8% of signals recorded were actually attributable to solid microemboli. Nevertheless, there were, in a predominantly radial study, a greater number of solid emboli with radial catheterization (median number 57 vs 36, P = 0.012). The majority of solid microemboli occurred with the passage of a catheter from the subclavian artery into the ascending aorta. About 15% of patients undergoing transradial coronary procedures had new lesions on MRI, with no new lesions seen in the 10 femoral access patients. Whether a numerical count of the Doppler signals is a good surrogate for neurological events again remains doubtful, particularly as the three patients (or 6%) who did have transient neurological symptoms were not those with higher emboli counts, nor even those with abnormal MRI scans. In addition, some caution must be applied while interpreting a small study of patients not randomized for access site.
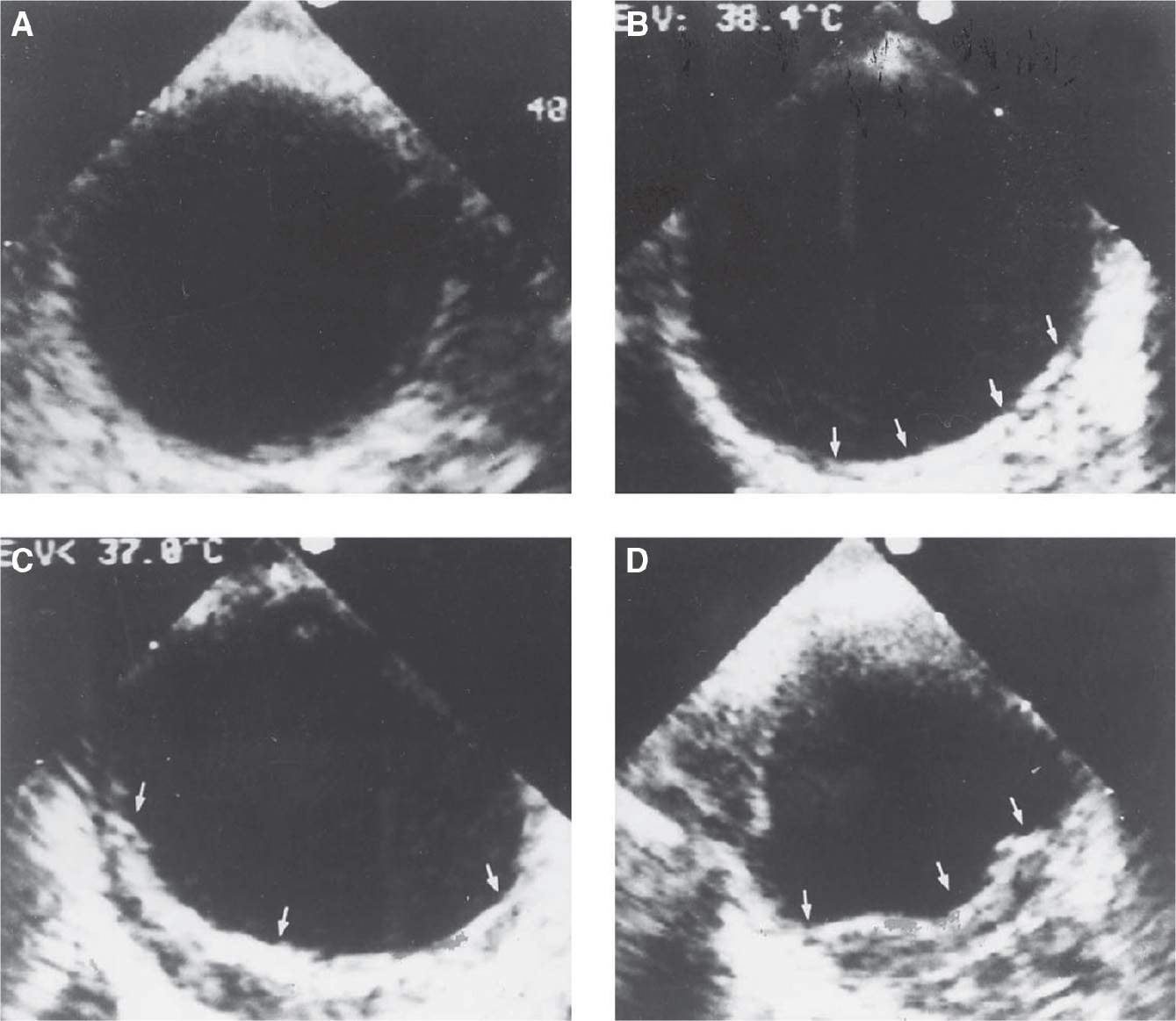
FIGURE 24-3 Location of aortic plaque at transoesophageal echocardiogram: Grade I & II (A & B): descending aorta 93%; arch 80%; ascending aorta only 37%. Complex plaque III & IV (C & D
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


