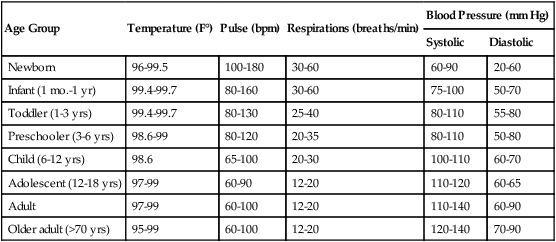
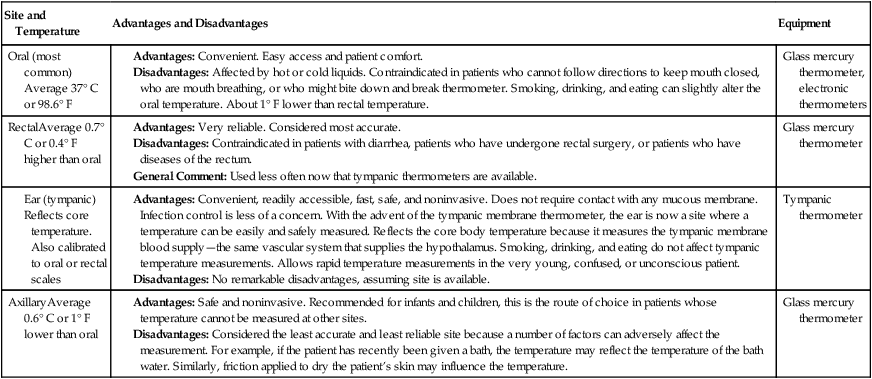
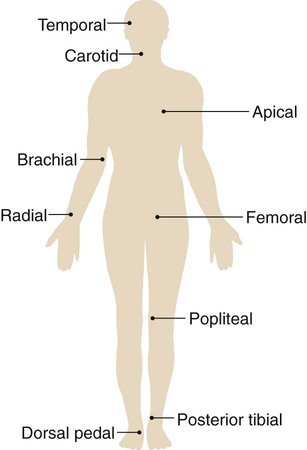
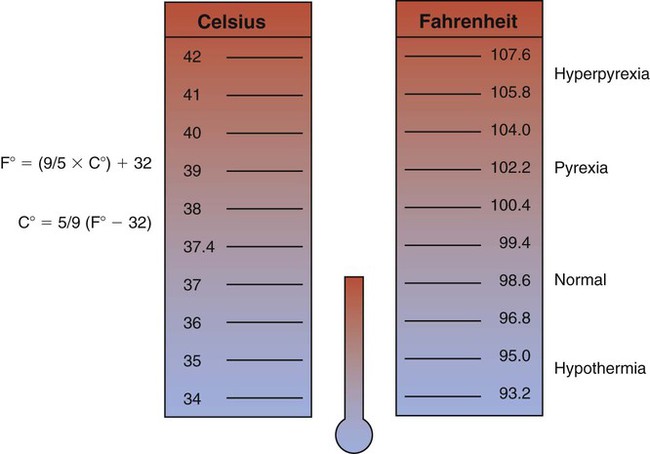
After reading this chapter, you will be able to: • Describe the major components of a patient’s vital signs, including: • Describe the systematic examination of the chest and lungs, including: • Discuss in more depth the common clinical manifestations observed during inspection, including normal ventilatory pattern and the common pathophysiologic mechanisms that affect the ventilatory pattern. • Describe the function of the following accessory muscles of inspiration: • Describe the function of the following accessory muscles of expiration: • Discuss the effects of pursed-lip breathing. • Describe the pathophysiologic basis for substernal and intercostal retractions. • Discuss splinting caused by chest pain or decreased chest expansion including pleuritic chest pain and nonpleuritic chest pain. • List abnormal chest shape and configuration. • List abnormal extremity findings, and include: • Altered skin color (e.g., cyanotic, pale, with prominent venous distention) • Presence or absence of digital clubbing • Presence or absence of peripheral edema • Presence or absence of distended neck veins • Describe how the following correlates to normal and abnormal sputum production, including: • Normal histology and mucous production of the tracheobronchial tree • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. The four major vital signs—body temperature (T), pulse (P), respiratory rate (R), and blood pressure (BP)—are excellent bedside clinical indicators of the patient’s physiologic and psychologic health. In many patient care settings, the oxygen saturation as measured by pulse oximetry (Spo2) is considered to be the fifth vital sign. Table 2-1 shows the normal values that have been established for various age groups. Table 2-1 Average Range for Vital Signs According to Age Group As shown in Figure 2-1, the normal body temperature is positioned within a relatively narrow range. A patient who has a temperature within the normal range is said to be afebrile. A body temperature above the normal range is called pyrexia or hyperthermia. When the body temperature rises above the normal range, the patient is said to have a fever or to be febrile. An exceptionally high temperature, such as 41° C (105.8° F), is called hyperpyrexia. Hypothermia is a core temperature below normal range. Hypothermia may occur as a result of (1) excessive heat loss, (2) inadequate heat production to counteract heat loss, and (3) impaired hypothalamic thermoregulation. Box 2-1 lists the clinical signs of hypothermia. Hypothermia may be caused accidentally or may be induced. Accidental hypothermia is commonly seen in the patient who (1) has had an excessive exposure to a cold environment; (2) has been immersed in a cold liquid environment for a prolonged time; or (3) has inadequate clothing, shelter, or heat. A reduced metabolic rate may compound hypothermia in older patients. In addition, older patients often take sedatives, which further depress the metabolic rate. Box 2-2 lists common therapeutic interventions for patients with hypothermia. Table 2-2 lists several factors that affect body temperature. Knowing these factors can help the practitioner to better assess the significance of expected or normal variations in a patient’s body temperature. Table 2-2 Factors Affecting Body Temperature Because body temperature is usually measured orally, the practitioner must be aware of certain external factors that can lead to false oral temperature measurements. For example, drinking hot or cold liquids can cause small changes in oral temperature measurements. The most significant temperature changes have been reported after a patient drinks ice water. Drinking ice water may lower the patient’s actual temperature by 0.2° to 1.6° F. Before taking an oral temperature, the practitioner should wait 15 minutes after a patient has ingested ice water. Oral temperature may increase in the patient receiving heated oxygen aerosol therapy and decrease in the patient receiving a cool mist aerosol. Table 2-3 lists the body temperature sites, their advantages and disadvantages, and the equipment used. Table 2-3 A pulse is generated through the vascular system with each ventricular contraction of the heart (systole). Thus a pulse is a rhythmic arterial blood pressure throb created by the pumping action of the ventricular muscle. Between contractions, the ventricle rests (diastole) and the pulsation disappears. The pulse can be assessed at any location where an artery lies close to the skin surface and can be palpated against a firm underlying structure, such as muscle or bone. Nine common pulse sites are the temporal, carotid, apical, brachial, radial, femoral, popliteal, pedal (dorsalis pedis), and posterior tibial area (Figure 2-2). The normal pulse rate (or heart rate) varies with age. For example, in the newborn the normal pulse rate range is 100 to 180 beats per minute (bpm). In the toddler the normal range is 80 to 130 bpm. The normal range for the child is 65 to 100 bpm, and the normal adult range is 60 to 100 bpm (see Table 2-1). Finally, the stimulation of the sympathetic nervous system increases the force of ventricular contraction, increasing the volume of blood ejected from the heart and creating a stronger pulse. Stimulation of the parasympathetic nervous system decreases the force of the ventricular contraction, thus leading to a decreased volume of blood ejected from the heart and a weaker pulse. Clinically the strength of the pulse may be recorded on a scale of 0 to 4+ (Box 2-3). The normal respiratory rate varies with age. For example, in the newborn the normal respiratory rate varies between 30 and 60 breaths per minute. In the toddler, the normal range is 25 to 40 breaths per minute. The normal range for the preschool child is 20 to 25 breaths per minute, and the normal adult range is 12 to 20 breaths per minute (see Table 2-1). Ideally the respiratory rate should be counted when the patient is not aware. One good method is to count the respiratory rate immediately after taking the pulse, while leaving the fingers over the patient’s artery. As respirations are being counted, the practitioner should observe for variations in the pattern of breathing. For example, an increased breathing rate is called tachypnea. Tachypnea is commonly seen in patients with fever, metabolic acidosis, hypoxemia, pain, or anxiety. A respiratory rate below the normal range is called bradypnea. Bradypnea may occur with hypothermia, head injuries, and drug overdose. Table 2-4 provides an overview of common normal and abnormal breathing patterns. Table 2-4 Common Normal and Abnormal Breathing Patterns The normal blood pressure in the aorta and large arteries varies with age. For example, in the newborn the normal systolic blood pressure range is 60 to 180 mm Hg. In the toddler the normal range is 80 to 110 mm Hg. The normal range for the child is 100 to 110 mm Hg, and the normal adult range is 110 to 140 mm Hg (see Table 2-1). The numeric difference between the systolic and diastolic blood pressure is the pulse pressure. For example, a systolic pressure of 120 mm Hg and a diastolic pressure of 80 mm Hg equal a pulse pressure of 40 mm Hg. Table 2-5 presents factors that affect the blood pressure. Table 2-5 Factors Affecting Blood Pressure Oxygen saturation, often considered the fifth vital sign, is used to establish an immediate baseline Spo2 value. It is an excellent monitor by which to assess the patient’s response to respiratory care interventions. In the adult, normal Spo2 values range from 95% to 99%. Spo2 values of 91% to 94% indicate mild hypoxemia. Mild hypoxemia warrants additional evaluation by the respiratory practitioner but does not usually require supplemental oxygen. Spo2 readings of 86% to 90% indicate moderate hypoxemia. These patients often require supplemental oxygen. Spo2 values of 85% or lower indicate severe hypoxemia and warrant immediate medical intervention, including the administration of oxygen, ventilatory support, or both. Table 2-6 presents the relationship of Spo2 to Pao2 for the adult and newborn. Table 2-7 provides an overview of the signs and symptoms of inadequate oxygenation. Table 2-6 Spo2 and Pao2 Relationship for the Adult and Newborn Table 2-7 Signs and Symptoms of Inadequate Oxygenation
The Physical Examination and Its Basis in Physiology
Vital Signs
Age Group
Temperature (F°)
Pulse (bpm)
Respirations (breaths/min)
Blood Pressure (mm Hg)
Systolic
Diastolic
Newborn
96-99.5
100-180
30-60
60-90
20-60
Infant (1 mo.-1 yr)
99.4-99.7
80-160
30-60
75-100
50-70
Toddler (1-3 yrs)
99.4-99.7
80-130
25-40
80-110
55-80
Preschooler (3-6 yrs)
98.6-99
80-120
20-35
80-110
50-80
Child (6-12 yrs)
98.6
65-100
20-30
100-110
60-70
Adolescent (12-18 yrs)
97-99
60-90
12-20
110-120
60-65
Adult
97-99
60-100
12-20
110-140
60-90
Older adult (>70 yrs)
95-99
60-100
12-20
120-140
70-90
Body Temperature
Factors Affecting Body Temperature
Age
Temperature varies with age. For example, the temperature of the newborn infant is unstable because of immature thermoregulatory mechanisms. However, it is not uncommon for the elderly person to have a body temperature below 36.4° C (97.6° F). The normal temperature decreases with age.
Environment
Normally, variations in environmental temperature do not affect the core temperature. However, exposure to extreme hot or cold temperatures can alter body temperature. If an individual’s core temperature falls to 25° C (77° F), death may occur.
Time of day
Body temperature normally varies throughout the day. Typically, an individual’s temperature is lowest around 3:00 am and highest between 5:00 pm and 7:00 pm. Approximately 95% of patients have their highest temperature around 6:00 pm. Body temperature often fluctuates by as much as 2° C (1.8° F) between early morning and late afternoon.
Exercise
Body temperature increases with exercise because exercise increases heat production as the body breaks down carbohydrates and fats to provide energy. During strenuous exercise, the body temperature can increase to as high as 40° C (104° F).
Stress
Physical or emotional stress may increase body temperature because stress can stimulate the sympathetic nervous system, causing the epinephrine and norepinephrine levels to increase. When this occurs, the metabolic rate increases, causing an increased heat production. Stress and anxiety may cause a patient’s temperature to increase without underlying disease.
Hormones
Women normally have greater fluctuations in temperature than do men. The female hormone progesterone, which is secreted during ovulation, causes the temperature to increase 0.3° to 0.6° C (0.5° to 1° F). After menopause, women have the same mean temperature norms as men.
Body Temperature Measurement
Pulse
Rate
Strength
Respiration
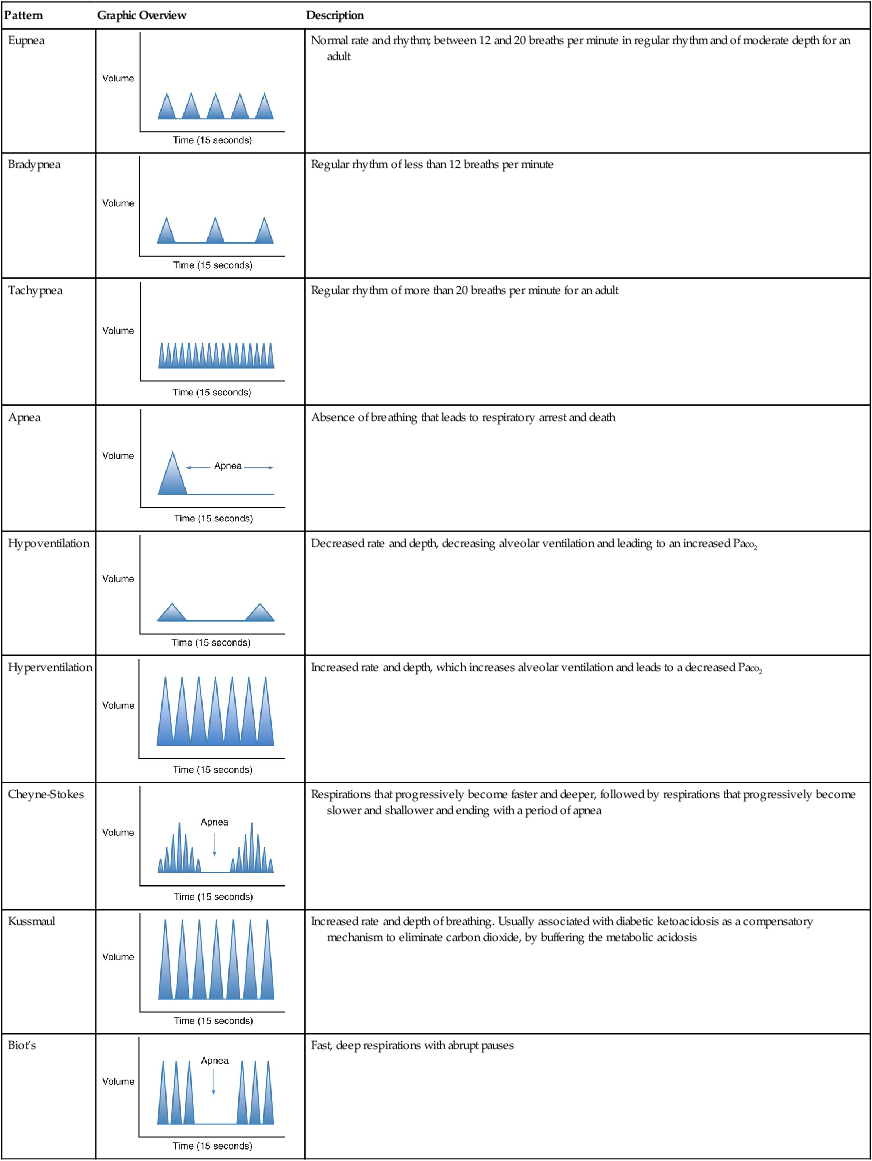
Pattern
Graphic Overview
Description
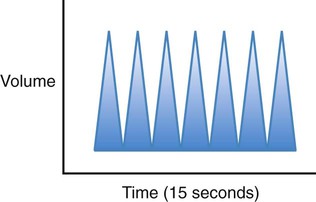
Eupnea
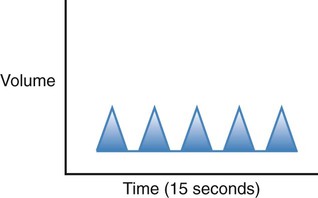
Normal rate and rhythm; between 12 and 20 breaths per minute in regular rhythm and of moderate depth for an adult
Bradypnea
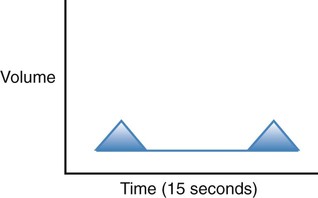
Regular rhythm of less than 12 breaths per minute
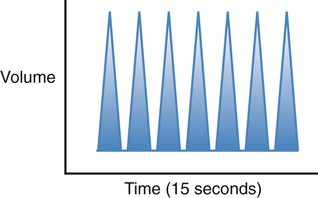
Tachypnea
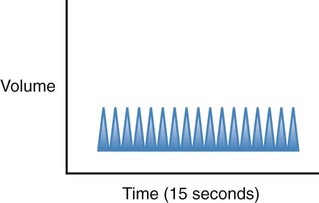
Regular rhythm of more than 20 breaths per minute for an adult
Apnea
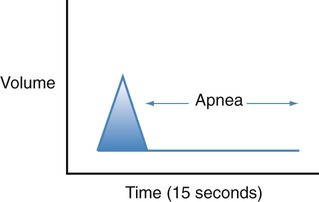
Absence of breathing that leads to respiratory arrest and death
Hypoventilation
Decreased rate and depth, decreasing alveolar ventilation and leading to an increased Paco2
Hyperventilation
Increased rate and depth, which increases alveolar ventilation and leads to a decreased Paco2
Cheyne-Stokes
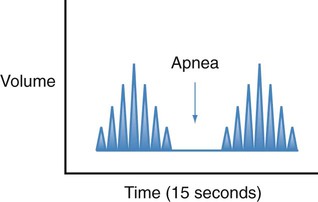
Respirations that progressively become faster and deeper, followed by respirations that progressively become slower and shallower and ending with a period of apnea
Kussmaul
Increased rate and depth of breathing. Usually associated with diabetic ketoacidosis as a compensatory mechanism to eliminate carbon dioxide, by buffering the metabolic acidosis
Biot’s
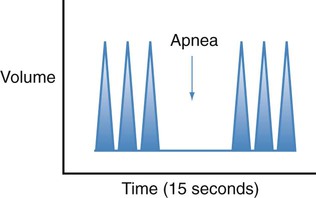
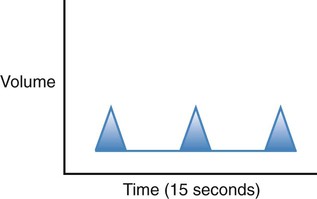
Fast, deep respirations with abrupt pauses
Blood Pressure
Resistance
Age
Blood pressure gradually increases throughout childhood, and correlates with height, weight, and age. In the adult, the blood pressure tends to gradually increase with age.
Exercise
Vigorous exercise increases cardiac output and thus blood pressure.
Autonomic nervous system
Increased sympathetic nervous system activity causes an increased heart rate, an increased cardiac contractility, changes in vascular smooth muscle tone to enhance blood flow to vital organs and skeletal muscles, and an increased blood volume. Collectively, these actions cause an increased blood pressure.
Stress
Stress stimulates the sympathetic nervous system and thus can increase blood pressure.
Circulating blood volume
A decreased circulating blood volume, either from blood or fluid loss, causes blood pressure to decrease. Common causes of fluid loss include abnormal, unreplaced fluid losses such as in diarrhea or diaphoresis, and overenthusiastic use of diuretics. Inadequate oral fluid intake can also result in a fluid volume deficit. Excess fluid, such as in congestive heart failure, can cause the blood pressure to increase.
Medications
Any medication that affects one or more of the previous conditions may cause blood pressure changes. For example, diuretics reduce blood volume; cardiac pharmaceuticals may increase or decrease heart rate and contractility; pain medications may reduce sympathetic nervous system stimulation; and specific antihypertension agents may exert their effects as well.
Normal fluctuations
Under normal circumstances, blood pressure varies from moment to moment in response to a variety of stimuli. For example, an increased environmental temperature causes blood vessels near the skin surface to dilate, causing blood pressure to decrease. In addition, normal respirations alter blood pressure: Blood pressure increases during expiration and decreases during inspiration. Blood pressure fluctuations caused by inspiration and expiration may be significant during a severe asthmatic episode.
Race
Black males over 35 years of age often have elevated blood pressures.
Obesity
Blood pressure is often higher in overweight and obese individuals.
Daily variations
Blood pressure is usually lowest early in the morning, when the metabolic rate is lowest.
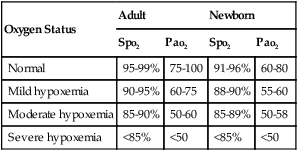
Oxygen Saturation
Oxygen Status
Adult
Newborn
Spo2
Pao2
Spo2
Pao2
Normal
95-99%
75-100
91-96%
60-80
Mild hypoxemia
90-95%
60-75
88-90%
55-60
Moderate hypoxemia
85-90%
50-60
85-89%
50-58
Severe hypoxemia
<85%
<50
<85%
<50
Central Nervous System
Apprehension
Early ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

 ) multiplied by resistance: BP =
) multiplied by resistance: BP =  + R.
+ R.