The Patient with Acute Myocardial Infarction
Felix Zijlstra
The timely restoration of antegrade coronary blood flow in the infarct-related artery of a patient with acute myocardial infarction (AMI) results in myocardial salvage and improved survival (1,2). Intravenous thrombolytic therapy and immediate cardiac catheterization, followed by primary percutaneous intervention (PCI), are both widely used reperfusion therapies. A recent review of 23 randomized trials comparing these two treatment modalities favors primary PCI with regard to mortality, reinfarction, and stroke (3). Given the superior safety and efficacy of primary PCI, this treatment now is preferred when logistics allow this approach, even when this necessitates additional transportation (4). As had been shown for PCI therapy for stable and unstable angina (4), it is likely that the results from various hospitals may differ considerably (5,6). Establishing and maintaining a proficient primary PCI program takes great institutional will and effort, and even institutions with a large experience of coronary PCI for stable and unstable angina will have something of a learning curve for primary PCI. The main issues pertinent to the delivery of primary PCI therapy are discussed here, following the sequence of events from a patient’s perspective. Our approach is described with regard to the prehospital phase, the first 15 in-hospital minutes, initial pharmacologic therapy, angiography, PCI, risk stratification, rehabilitation, and secondary prevention.
PREHOSPITAL PHASE
A speedy response and early recognition of AMI by general practitioners and ambulance services are of great importance, mainly for two reasons. First, mortality in the very early hours is substantial, and many patients die before adequate medical help has been sought and delivered (7). Second, although the results of primary PCI therapy are less time dependent than the results of thrombolysis (8), in particular during the first few hours, time is muscle. This is not only so from a theoretical perspective, but has been confirmed in a recent study that showed that an increase in time delay from presentation to first balloon inflation results in worse clinical outcome, in particular in high-risk patients (9). Confirmation of the diagnosis of AMI by 12-lead electrocardiography (EKG), by either general practitioners or ambulance paramedics, allows a substantial reduction of the time delay to first balloon inflation, because the hospital and the catheterization laboratory can be prepared in advance, and the emergency room and the cardiac care unit (CCU) (with their unavoidable delays) can be skipped on the way to acute angiography. Furthermore, it gives important opportunity to start initial pharmacologic therapy and use the transportation time in this regard. A primary PCI center must therefore develop additional specific training programs for general practitioners and ambulance services. Excellent communication with these first-line providers of care for patients with AMI is of paramount importance, because this will be among the main factors determining time to therapy.
THE FIRST 15 IN-HOSPITAL MINUTES
If a definitive diagnosis has not been made before arrival at the hospital, it is very important that additional delays are avoided. A limited history and physical examination should be performed, and a 12-lead EKG should be made and interpreted within 5 to 10 minutes (7). Blood tests may be drawn, but results should not be waited on; a chest x-ray is
unnecessary. The first responsibility of the emergency room physician is to contact the catheterization laboratory and to get the patient there as soon as possible. Important organizational issues that determine the logistics in this regard are:
unnecessary. The first responsibility of the emergency room physician is to contact the catheterization laboratory and to get the patient there as soon as possible. Important organizational issues that determine the logistics in this regard are:
Who is in charge of patients with suspected cardiac symptoms in the emergency room?
Who is in charge of the CCU?
What types of nurses are staffing the emergency room?
It is a great advantage if:
The CCU is run by an interventional cardiologist.
The emergency room physicians are supervised by the head of the CCU.
The CCU, catheterization laboratory, and emergency room nurses fall within the same organizational unit and therefore know each other’s work.
Finally, a flexible attitude shared by the catheterization laboratory staff and interventional cardiologist is a prerequisite. They should be prepared to change their program at a moment’s notice—drop a nice elective case planned for intracoronary ultrasound or multiple stenting—get out of bed in the middle of the night, and do this job as quickly and proficiently as they can.
INITIAL PHARMACOLOGIC THERAPY
Adequate pain relief and supplemental oxygen are essential, not only for humanitarian reasons, but in particular because the patient has to endure angiography and angioplasty (7). Aspirin should be given, at least 300 mg soluble chewable, but because gastrointestinal symptoms are frequent, it may be preferable to give 500 mg of aspirin intravenously. Sublingual and intravenous nitroglycerine as well as intravenous β-blockers (10), unless contraindicated, should be given in an effort to lower oxygen consumption and alleviate myocardial ischemia. Intravenous heparin can be used in an attempt to increase initial patency rates of the infarct-related vessel (11), and heparin plays an important role during the PCI. Abciximab and tirofiban as pretreatment and concomitant therapy can be recommended for most patients (12, 13, 14). Clopidogrel now is used in all patients with an acute coronary syndrome, and it should be started with a loading dose of at least 300 mg (15).
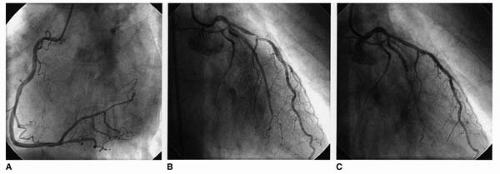 Figure 34.1. A 70-year-old man collapsed while attending a soccer game, around 3:00 PM. When an ambulance arrived, his heart rate was 80 beats per minute, with a blood pressure of 80/45 mm Hg. A 12-lead EKG showed a sinus rhythm with a bundle branch block and ST-elevation in all anterior leads. The patient was transferred to a nearby community hospital, and at 4:30 PM, the cardiologist in this local hospital decided to refer the patient for primary PCI, over a distance of 80 km. Before transportation, aspirin and clopidogrel were given, and intravenous heparin and tirofiban were started.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|