Fig. 10.1
The Vanderbilt hybrid operating room: a combined surgical operating room and catheterization laboratory
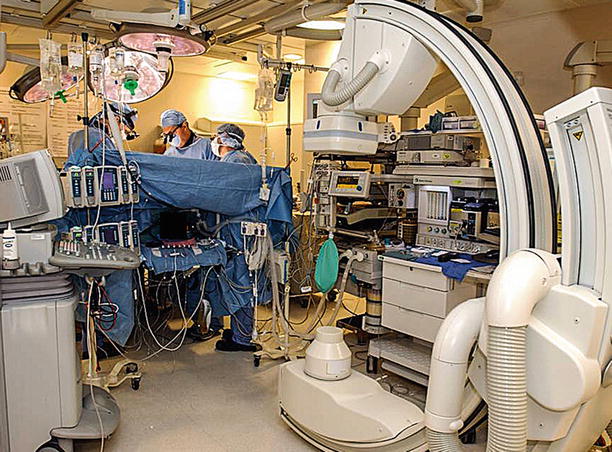
Fig. 10.2
The Vanderbilt hybrid operating room: view from the anesthesia side. The C-arm radiographic equipment can be deployed easily for either a completion angiogram or percutaneous procedure
Currently, in our hybrid OR we perform the following procedures: (1) completion angiography after coronary artery bypass grafting (CABG), (2) combined CABG and percutaneous coronary interventions (PCI), (3) combined minimally invasive valve surgery and PCI, and (4) combined MIDCAB and PCI operations. By analyzing our clinical outcomes continuously, we have found “one-stop” hybrid therapy to be reasonable, safe, feasible, and to result in excellent outcomes. The hybrid operating room is the perfect venue for performing combinations of robotic mitral and coronary surgery with percutaneous interventions.
Operative Set-Up
Effective planning and design of an integrated hybrid OR is a complex process that requires several months of collaboration between clinicians and technicians as well as representatives from the hospital administration, engineering, architecture, and OR staff as well as imaging equipment vendors. This process addresses major design considerations that include financial, space, imaging system, and operating room table requirements.
A newly built hybrid OR costs between one and four million dollars, depending upon the amount of structural reconstruction and equipment needed [3, 4]. This significant investment requires careful evaluation of the financial and social returns as well as commitment from the hospital administration. Experts recommend spatial dimensions of at least 750–900 ft2 with a floor to ceiling height of at least 10 ft to install state-of-art imaging systems that are capable of performing 3-D rotational angiography, CT scanning, and intravascular ultrasound [3, 4]. Ceiling-mounted imaging systems have the advantage of keeping the floor space maximized for anesthesia equipment and personnel, conventional OR traffic, and patient flow. Disadvantages of these systems include impairment of installation conventional OR lighting equipment and can affect air filtration systems. Floor-mounted systems have advantages and disadvantages as well. The newer generation of floor-mounted systems can be built farther from the operating table, thereby not impeding conventional OR traffic and patient flow (Fig. 10.3). A multi-functional operating table is fundamental to a successful hybrid OR and must provide both ideal imaging capabilities and operating room flexibility. Current carbon-fiber imaging tables are not flexible and sometimes require inflatable cushions for proper patient positioning during surgery. The newer generation of OR imaging tables have the capability to rotate side-to-side and to move into both standard Trendelenburg and reversed positions. These tables have special rails for mounting conventional retractors and camera holders. In order to perform 3-D imaging, the C-arm must be integrated fully with the table. Current flexible OR tables are not integrated with the C-arm, precluding 3-D imaging. However, operating table technology is advancing continuously, and the results are very promising.
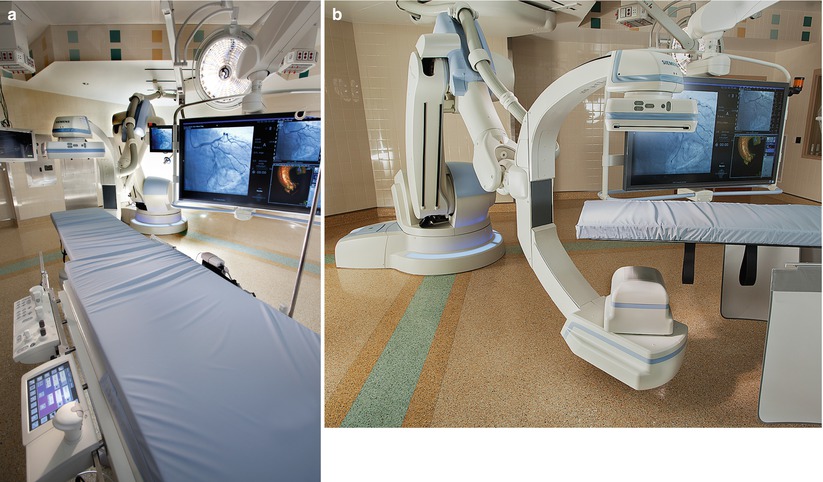
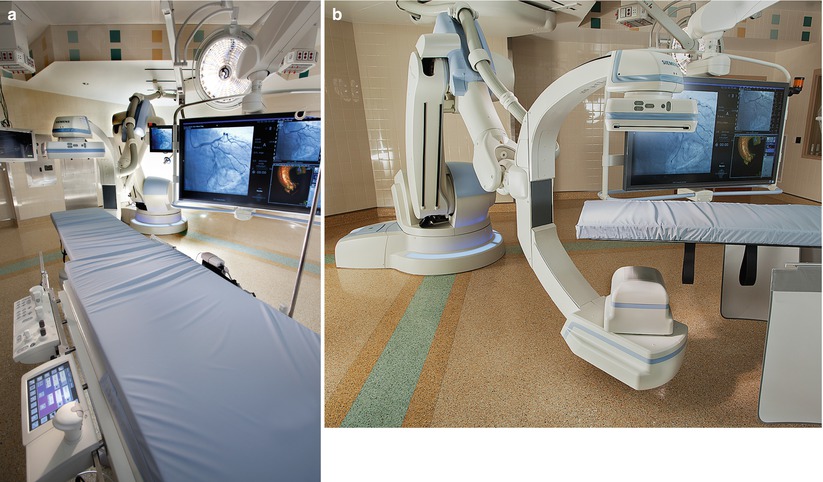
Fig. 10.3
Floor mounted siemens artis Zeego® multi-axial imaging system: (a) This is an example of a modern floor mounted imaging system in a hybrid operating room. (b) This device operates robotically to render 18° of imaging freedom around the operating/catheterization table. Multiple images can be reconstituted to provide 3-D reconstructions of radiographic targets (East Carolina Heart Institute)
Operative Technique: Hybrid Coronary Artery Revascularization
Initial outcomes with our “one stop” hybrid coronary revascularization procedures are encouraging. Although median sternotomy has been the incision of choice for patients with left anterior descending coronary artery (LAD) disease, we have evolved to using minimally invasive methods. In the hybrid operating room we perform direct vision off-pump MIDCAB operations as well as those under robotic guidance. Herein, we describe our MIDCAB technique using robotic assisted camera positioning.
Using a beanbag, patients were positioned on the operating table with the left chest elevated 25°. After general anesthesia, the arms were abducted and secured over the head. After standard sterile preparation, a 5-mm trocar was inserted along the posterior axillary line at the nipple level. After left lung deflation, the chest is insufflated with carbon dioxide (10–12 Torr) while monitoring patient hemodynamics. After the endoscopic camera is positioned inside the chest, the left internal mammary artery is inspected first. Two additional 5-mm ports then are placed slightly more anteriorly and 4–6-cm from the initial incision. These ports are used to insert robotic graspers, dissectors, and the electrocautery. The left internal thoracic artery is harvested using both the electrocautery and harmonic scalpel. Visualization is facilitated by the AESOP (Automated Endoscopic System for Optimal Positioning) device, which provides robot-assisted voice activated camera control [Intuitive Surgical, Sunnyvale, Calif.]. AESOP is a surgeon-controlled robotic arm that can maneuver and position an endoscope in minimally invasive heart surgery. Other endoscopic camera holders can be used as well. After the ITA is freed from the chest wall, heparinized (ACT > 300), and clipped both proximally and distally, it is transected. After localizing the LAD with the thoracoscope and placing a site-specific needle through the anterior chest wall, the MIDCAB procedure is performed through a 4–6-cm anterior chest wall incision. Pericardial sutures are placed for exposure, and the LAD is identified directly and is opened with a #15 scalpel blade and Potts scissors. We place a 2.5-mm intra-coronary shunt to maintain distal flow during the off-pump ITA to LAD anastomosis, which is done using a running 7-0 polypropylene suture. Heparin then is reversed with protamine and during this time the chest is closed. A 28 French tube is placed in the left chest for drainage. A completion on-table angiogram then is performed to assure anastomotic patency. For patients who undergo a planned hybrid procedure (a PCI followed by a MIDCAB), the cardiac surgeon and the interventional cardiologist review the coronary angiogram together in advance.
If a combined surgical and percutaneous intervention is technically feasible, the hybrid approach is presented to the patient and specific consent is obtained. These patients receive preoperative 300 mg of clopidogrel orally in the holding area. For these procedures vascular access is gained with a percutaneous femoral sheath and then the PCI procedure is performed. Thereafter, the additional drape is removed, and the surgical operation is performed. At the end of the surgery, the sheath typically is removed after heparin reversal with protamine. A Syvek patch (Marine Polymer Technologies, Danvers, Mass.) is applied to the groin followed by 12 min of manual compression.
Completion Angiography
At Vanderbilt, from April 2005 to June 2007, 366 consecutive patients underwent CABG surgery followed by intraoperative completion angiography. Before chest closure either an interventional cardiologist or a surgeon performed coronary graft angiography. If angiographic defects were identified, either a surgical or percutaneous revision was done. Repeat angiography then was performed to ensure defect correction before chest closure. In our series angiographic defects were divided into three categories that were based on the location within either the graft or target vessel: (1) conduit defects, (2) anastomotic defects, and (3) target vessel errors. Defect repairs were subdivided into two categories: (1) minor defects—a minor but important adjustment of the graft without additional cardiopulmonary bypass or aortic cross-clamping; (2) major defects requiring either an open chest PCI or surgical revision that may require cardiopulmonary bypass and/or aortic cross-clamping or off-pump surgical revision of the anastomosis. For unplanned hybrid procedures, that is those in whom the decision to perform a PCI was based on intra-operative findings, patients received 300 mg of clopidogrel via nasogastric tube at the time of an open-chest PCI.
Operative Technique: Hybrid Mitral Valve Surgery and PCI
Outcomes have been promising in patients who have undergone concomitant PCI and mitral valve operations. In a planned hybrid procedure, 300 mg of clopidogrel is given in the holding area. After appropriate anesthesia, a single lumen endotracheal tube is placed, and a pacing Swan-Ganz pulmonary artery catheter is introduced. A trans-esophageal echocardiogram is performed in every patient. Patients are positioned with the right side of the chest elevated slightly. External defibrillator (ZOLL Medical Corporation, Chelmsford, MA) patches are placed to subtend the mass of the heart. Before heparin administration, a femoral arterial sheath is placed using the Seldinger technique. Then the PCI is performed to address significant coronary lesions. Thereafter, femoral vessels are exposed through a transverse incision, and after full systemic heparinization, the artery is cannulated using either an 18 or 16 French straight perfusion cannula (Edwards Life Sciences, Irvine, Calif.). In patients either with grade four or five aortic atherosclerosis or suspected aorto-iliac disease, either axillary arterial or direct aortic cannulation is performed. Using the Seldinger technique the femoral vein is cannulated with a 28 French venous catheter. In patients requiring tricuspid valve surgery or another right heart procedure, the superior vena cava is cannulated also to maximize venous drainage. Patients are placed on cardiopulmonary bypass (CPB) using vacuum-assisted drainage. To induce fibrillatory arrest, patients are cooled to below 28 °C. If cooling does not induce fibrillatory arrest, rapid pacing is added to activate ventricular fibrillation. The left atrium is then opened in the atrio-ventricular groove, and the mitral valve is exposed using a specially designed hand held atrial retractor, inserted through the incision. We perform either the mitral valve repair or replacement under direct vision using long-shafted instruments (Edwards Lifesciences Inc, Irvine Calif.). To treat concomitant atrial fibrillation, we perform at least a left sided cryo-MAZE procedure using the malleable Cryocath™ probe (Medtronic, Inc., Minneapolis, Minn.). Moreover, any co-existing patent foramen ovale is closed at this time. Mitral valve bioprosthesis replacements typically are performed using either a Mosaic™ (Medtronic Inc., Minneapolis, MN) or a Biocor™ porcine prosthetic valve (St. Jude Medical, Minneapolis, MN). These prostheses facilitate minimally invasive valve operations because of their retractable commissural posts, which helps during valve insertion and positioning. To displace intra-cardiac air, carbon dioxide is insufflated into the thorax throughout the procedure. A left atrial pump sucker is positioned in the left superior pulmonary vein to maintain a clear operative field. Upon completion of the valve procedure, lungs are inflated to flush any residual pulmonary vein air through the atriotomy suture line.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


