The Heart in Hypertension
Introduction
A number of cardiac derangements complicate the natural history and progressive course of systemic hypertensive vascular disease. In addition, several independent comorbid diseases, each with its own natural history, can further complicate the overall clinical problem of hypertensive cardiac and vascular disease.
Left ventricular hypertrophy
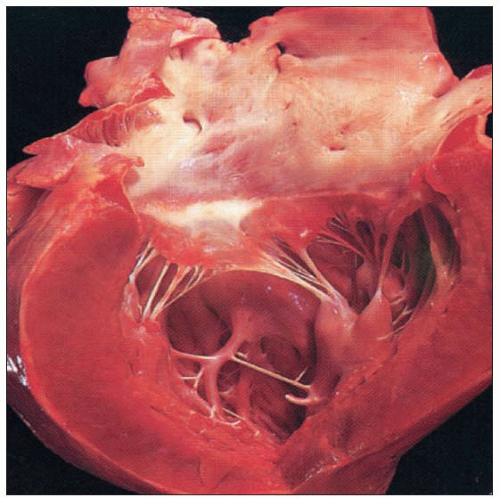
One cardiac complication of essential hypertension, perhaps the most common, is left ventricular hypertrophy (LVH) (5.1). A multiplicity of haemodynamic and non-haemodynamic factors are associated with the development of LVH in essential hypertension (5.2).
LVH predisposes the affected patient to microvascular angina pectoris, myocardial ischaemia, interstitial and perivascular fibrosis, apoptosis, infarction, cardiac dysrhythmias, cardiac failure, sudden cardiac death and inflammatory responses (Table 5.1). It is exceedingly important for the cardiovascular and primary care physician to recognize the devastating potential of each of those factors as well comorbid diseases that are associated with LVH and hypertensive heart disease. Note that not listed is myocardial infarction resulting from epicardial atherosclerosis, an independent disease with its own natural history and which is exacerbated by hypertension.
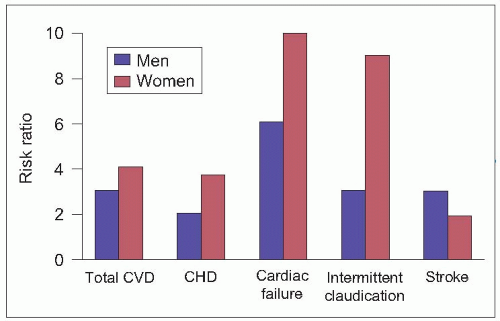
The Framingham Heart Study has shown that hypertension is a major risk factor for the development of congestive heart failure (CHF) (5.3). The cumulative incidence of CHF is higher in men than in women and increases with age (5.4). In the 1970s systolic heart failure resulting from untreated hypertension was the primary explanation; in the 1990s, diastolic dysfunction, resulting from ischaemia, fibrosis and apoptosis with remodelling, was the main explanation.
Components of hypertensive heart disease and its relationship with atherosclerotic heart disease
Hypertensive heart disease (HHD) is associated with several cardiac and vascular derangements: initiation and progression of LVH; constriction of the coronary arterioles by the same mechanisms that affect the systemic arterioles of all body organs in hypertension; acute and chronic ischaemic hypertensive heart disease with microvascular angina pectoris; endothelial dysfunction of the arterioles and ventricular endothelium; apoptosis; acute and chronic left ventricular failure; ventricular dysrhythmias; and sudden cardiac death. Each of the foregoing alterations increases the likelihood of complications and death from occlusive atherosclerosis of the epicardial coronary arteries.
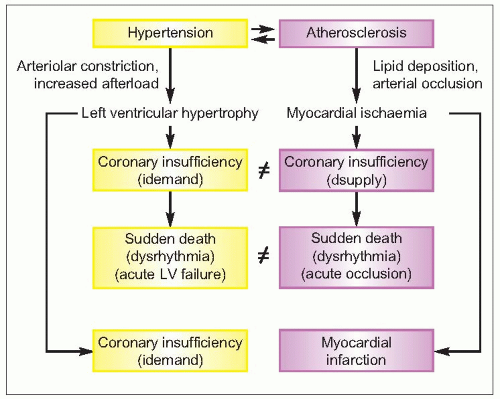
Atherosclerosis is an independent comorbid disease process that results in occlusion of the larger epicardial coronary arteries and ischaemic disease of the heart, which also frequently results in angina pectoris, myocardial ischaemia, fibrosis, infarction, left ventricular failure, cardiac dysrhythmias and sudden cardiac death. Therefore, each of the two diseases, hypertension and atherosclerosis, follows its own natural history (5.5), and each accelerates, exacerbates, and is a major underlying risk factor for, the other.
Table 5.1 Consequences of LVH in patients with essential hypertension | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 5.3 Causes of congestive heart failure. CHD, coronary heart disease; HCVD, hypertensive cardiovascular disease; RHD, rheumatic heart disease. Reproduced with permission from McKee PA, Castelli WP, McNamara OM, Kannel WB: The natural history of congestive heart failure: the Framingham Heart Study. N. Engl. J. Med. 1971;285:1795-1801. |
Note that, although the two diseases have similar effects, they differ pathophysiologically. Hypertension is related to increased oxygen demand whereas atherosclerosis relates to insufficient oxygen supply.
Diabetes mellitus
Diabetes mellitus frequently coexists with essential hypertension and may be associated with its own specific cardiac and vascular complications. Diabetes also accelerates and aggravates the development and elaboration of cardiovascular disease (CVD), having its own pathophysiological derangements, which may account for the increased risk for the development of coronary heart disease (CHD). Diabetes is also associated with other cardiac and vascular complications, including those of hypertension. Diabetes impairs tissue perfusion by enhancing the progression of atherosclerotic disease of the medium-sized and larger coronary and other arteries that constitute the microcirculation of the heart, kidneys and other organs. It causes further deterioration of tissue perfusion of kidney, heart, brain, eyes and skeletal muscle that is already impaired by the arteriolar constriction and reduced blood flow and blood flow reserve of these organs as a result of hypertensive vascular disease. In addition, diabetes causes a further degree of enlargement of the left ventricle at any given level of arterial pressure. Whether this is the result of more severe myocardial hypertrophy or of augmented myocardial fibrosis or other infiltrative disease (e.g. protein deposition) remains a subject of intense study.
Note that in the Framingham study patients with diabetes, regardless of gender, developed increased cardiovascular events during follow-up including CHD, heart failure, peripheral vascular disease and stroke (5.6).
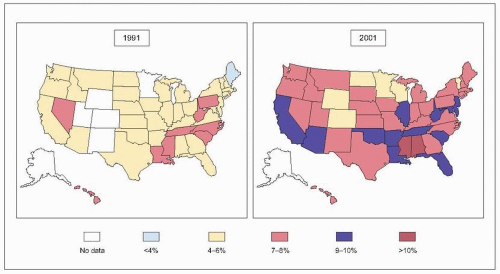
Glucose intolerance, insulin insensitivity, hypertension, atherosclerosis, hyperlipidaemia and obesity account for a metabolic syndrome (Table 5.2), which is of increasing pathophysiological, clinical and therapeutic significance. The prevalence of diabetes has increased markedly in the United States in the last 10 years (5.7).
Obesity
Another disease that commonly coexists with hypertension is exogenous obesity, yet another independent risk factor underlying atherosclerosis and CHD. Obesity exacerbates hypertensive heart disease by superimposing a significant volume overload (i.e. preload). The increased venous return to the heart (i.e. cardiopulmonary volume) is superimposed upon the pressure-overloaded left ventricle and expands intravascular volume is in direct proportion to the increase in body mass. Thus, the heart in obese patients with hypertension suffers from volume as well as pressure overload, which, in turn, promotes a dimorphic structural adaptation, one of eccentric as well as concentric LVH.
Other risk factors
Tobacco addiction and hyperlipidaemia are additional independent risk factors underlying coronary heart disease and they also compound the complexity of hypertensive heart disease. Some of these comorbid diseases and complications will be discussed in further detail below. Moreover, other comorbid cardiac diseases may include hypertrophic cardiomyopathy, idiopathic mitral valve prolapse syndrome, myocardial fibrosis or aortic valvular stenosis of the elderly and impaired coronary arterial endothelial dysfunction. And, clearly, the ageing process per se is another complicating factor.
Table 5.2 National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) criteria for the diagnosis of metabolic syndrome (defined as the presence of three or more of the following factors) | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
Haemodynamic correlates in LVH development
The mass and wall thickness of the left ventricle progressively increase in direct proportion to the unrelenting and progressive afterload imposed upon it by the added chamber stress. In addition, reduced compliance of the aorta and large arteries adds to the effect of afterload imposed on the left ventricle. Thus, although the structural changes of concentric LVH take place in response to the ever-increasing left ventricular afterload, they provide an efficient adaptive means for overcoming the physical forces necessary to maintain stable contractile function. This constitutes a positive aspect of LVH in that it delays the occurrence of left ventricular failure (in the absence of effective antihypertensive therapy). On the other hand, this beneficial feature of LVH is offset by the intrinsic risks of ischaemia, fibrosis, apoptosis and inflammatory responses, which together account for the ‘independent’ risk of heart failure associated with LVH.
Meerson theory
Felix Meerson suggested several decades ago that the initial response of the heart to pressure overload is the Frank-Starling mechanism, which accounts for ventricular hyperfunction (5.8). This functional response results in a period of stable hyperfunction that is associated with the structural adaptation of LVH. Our haemodynamic research work in naturally occurring hypertension has confirmed that the sequence postulated by Meerson occurs in patients with essential hypertension; we further confirmed these findings in the spontaneously hypertensive rat (SHR), which is probably the best experimental model of naturally occurring essential hypertension in humans.
 5.8 LVH development according to Meerson. |
Recent knowledge of LVH development
Recent molecular and cellular biological research has shown that the increased functional performance that results from pressure-overloaded LVH (i.e. the stage of Frank-Starling hyperfunction) is accompanied by a concurrent biological response by the cardiac myocytes. Thus, as the cardiac myocyte is stretched by the initial increase in pressure overload, the cell is stimulated to increase protein synthesis, and cellular hypertrophy results (5.9). Thus, the sequence of the cardiac response to pressure overload is not functional followed by structural adaptations; both responses occur simultaneously. The sequence that was postulated earlier by Meerson can now be modified. Instead of the initial hyperfunctional response being followed by structural adaptation, the initial myocytic stretch (induced by pressure overload) evokes simultaneous hyperfunctional and structural adaptive responses. More recent experimental and clinical studies have also shown that these structural changes are accompanied by other responses, such as progressive ischaemia (especially on functional demand), extracellular and perivascular fibrosis and enhanced naturally occurring cell death (apoptosis) of the ventricular myocytes, and, probably, inflammatory responses that promote cardiac failure.
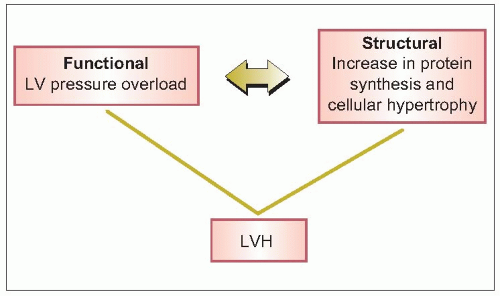 5.9 Recent knowledge of LVH development. |
Clinical correlates of LVH progression
In our earlier clinical investigative work, we demonstrated that one of the very early changes related to early development of LVH is impaired left ventricular filling during diastole. We have shown that these changes can be identified clinically and electrocardiographically by the presence of an atrial diastolic gallop rhythm (i.e. fourth heart sound or bruit de gallop) (see p. 19)(5.10, 5.11). This long-recognized heart sound is a clinical finding that is highly concordant with electrocardiographic indices of left atrial abnormality, higher arterial pressure and an increased prevalence of cardiac dysrhythmias. Indeed, further electrocardiographic studies confirmed our initial findings, enabling us to describe the structural and functional correlates in patients with essential hypertension. In those patients with only left atrial abnormality on ECG, left ventricular mass and septal and posterior wall thickness were increased, associated with the larger left atrium. Furthermore, left ventricular contractility was already impaired at this stage, and those patients with obvious LVH (by ECG) had a significantly larger left ventricle (in terms of mass as well as wall thickness) than those patients with left atrial abnormality only. Moreover, all patients with ECG-apparent LVH exhibited an enlarged left atrium on ECG. Haemodynamically, then, as one progresses from the normal subject to the patient with essential hypertension and atrial enlargement and then to the patient with obvious LVH, arterial pressure and total peripheral resistance increase pari passu, and these haemodynamic changes are associated with the structurally adaptive changes of LVH. Furthermore, left atrial enlargement associated with early LVH is accompanied by a reduction in left ventricular ejection rate, and with ECG-apparent LVH the left ventricular ejection fraction becomes impaired. Finally, these ECG correlates were confirmed echocardiographically and it was demonstrated that left atrial abnormality was associated with significant increases in left ventricular mass and wall thickness (5.12. 5.13, 5.14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree