(1)
Anatomy Department, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania
Abstract
Both vegetative systems, sympathetic and parasympathetic, participate in the extrinsic innervation of the heart, this being both motor and sensitive.
9.1 Cardiac Pain: Anatomical and Clinical Considerations
Both vegetative systems, sympathetic and parasympathetic, participate in the extrinsic innervation of the heart, this being both motor and sensitive.
Before commencing, some comments are mandatory:
Low pressure baroreceptors exist in the atrial wall. These receptors are part of a system of receptors of low pressure that can also be found in the venous network and are involved mainly in the control of blood volume. Stimulation of these receptors has both renal and vascular effects.
If the low pressure receptors are denervated, the false impression of low blood volume is induced and the regulating mechanisms of fluid retention and rise of blood pressure are activated.
Receptors for pain (free nerve endings) are infrequent in the working myocardium and numerous in the endocardium, and even more in the epicardium. They are also present in the arterial and periarterial wall. As a consequence, damage to the territories with large numbers of receptors is more painful than damage to the territories with lesser receptors.
Cardiac pain – referred pain: one of the rules of development is metamerism. In principle, the development of the body is segmentary. One segment called metamer is correlated with a viscerotome (the viscera with origin in this metamer), a neurotome (the nerves of the metamer), a myomer (the muscles derived from that segment) and a dermatome (a cutaneous segment innervated by the spinal nerve of the metamer).

Fig. 9.1
The superficial component of the cardiac nerve plexus on the anterior aspect of the ascending aorta

Fig. 9.2
The needle indicates a small prominance on the periaortic nervous course, which is actually a juxtavisceral nervous ganglion
Without a doubt, during development fusions occur that don’t permit to follow the exact metameric origin but as a principle, the metamer and the viscerotome derived from it have the same number and that is the number of the corresponding spinal nerve.
In the case of cardiac pain we are used to say that the pain migrates in the territories clinically known. In reality, it’s about the referred pain in the dermatome with the same number as the viscerotome and the respective neurotome [1]. The viscerotomes that participate in the development of the heart are from C2 to T4.
The cubital side of the upper limb belongs to the C8–T1 dermatome, the anterolateral aspect of the neck belongs to the C2 dermatome and the precordial and scapular regions belong to the T1–T4 dermatomes.
We state that the vegetative sensitive fibers of cardiac origin have two ascending pathways: some are reticulospinothalamic and some join the specific spinothalamic fibers that also conduct cutaneous impulses.
This being said, the explanations of the referred pain are not unitary but evocative:
The convergence phenomenon in the spinothalamic pathway (10/1 convergence of the peripheral fibers to a spinothalamic fibers). Following the common ascending pathway, nociceptive cardiac impulses are transmitted as belonging to a cutaneous territory.
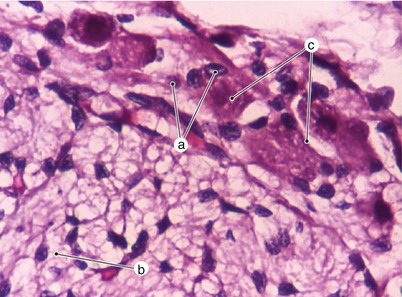
Fig. 9.3
Subepicardial ganglion in relation with the ventricular myocardium. a satellite cells nuclei, b myocardium, c neurons
Influx irradiation from the low myelinated or non-myelinated visceral sensitive fibers into surrounding cutaneous spinothalamic fibers. These fibers transmit the information into cerebral areas corresponding to a cutaneous territory.
Medullar facilitation process: pain impulses from a suffering organ diminish the excitability threshold of the surrounding somatic neurons and the somatic sensitivity arrived at these neurons, even under the pain threshold, is transmitted to the superior centers and misinterpreted as peripheral pain.
Cortical facilitation process: visceral pain projections on the cerebral cortex permit reception of cutaneous impulses under the pain threshold as false pain sensations.
Visceral pain of cardiac origin has an important biological significance. It may be accompanied by somatic and vegetative reflexes as well as relevant mood disorders. At times these may be the only signs of cardiac illness.
We emphasize that cardiac activity is under the influence of the carotid glomus regulating reflexes (there are other glomic structures, such as those in the mediastinum and pelvis that may indirectly modify the heart function).
At the end of these comments, we stress that direct links between vegetative nerve fibers and P cells have never been reported. Furthermore, neuromuscular junctions between extrinsic innervation and “working” cardiomyocytes have never been described in literature. Amyelinic nerve fibers belonging to both sympathetic and parasympathetic end in the vicinity of the myocytes (Gray’s anatomy, ed. 37, pg. 558).
9.2 Parasympathetic Innervation
The effector structures influenced by vegetative fibers are: the atrial and ventricular myocardium, the nodes of the conducting tissue and the coronary vessels muscles.
The cardiac nervous plexus at the base of the heart receives both sympathetic and parasympathetic fibers. The plexus lies around the great vessels and may be described in terms of a superficial component (between the aortic arch and the pulmonary trunk) (Figs. 9.1 and 9.2) and a deep component around the inferior vena cava and posterior to the ascending aorta. The plexus also contains ganglion cells generally considered paravisceral and intramural parasympathetic ganglia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


