2
The ECG in Patients with Palpitations and Syncope
Between Attacks
THE CLINICAL HISTORY AND PHYSICAL EXAMINATION
PALPITATIONS
‘Palpitations’ mean different things to different patients, but a general definition would be ‘an awareness of the heartbeat’. Arrhythmias, fast or slow, can cause poor organ perfusion and so lead to syncope (a word used to describe all sorts of collapse), breathlessness and angina. Some rhythms can be identified from a patient’s description, such as:
• A patient recognizes sinus tachycardia because it feels like the palpitations that he or she associates with anxiety or exercise.
• Extrasystoles are described as the heart ‘jumping’ or ‘missing a beat’. It is not possible to distinguish between supraventricular and ventricular extrasystoles from a patient’s description, although they can be differentiated from an ECG.
• A paroxysmal tachycardia begins suddenly and sometimes stops suddenly. The heart rate is often ‘too fast to count’. Severe attacks are associated with dizziness, breathlessness and chest pain.
Table 2.1 compares the symptoms associated with sinus tachycardia and a paroxysmal tachycardia, and shows how a diagnosis can be made from the history. Note that a heart rate between 140/min and 160/min may be associated with either sinus or paroxysmal tachycardia.
Table 2.1
Diagnosis of sinus tachycardia or paroxysmal tachycardia from a patient’s symptoms
| Symptoms | Sinus tachycardia | Paroxysmal tachycardia |
| Timing of initial attack | Attacks probably began recently | Attacks probably began in teens or early adult life |
| Associations of attack | Exercise, anxiety | Usually no associations, but occasionally exercise-induced |
| Rate of start of palpitations | Slow build-up | Sudden onset |
| Rate of end of palpitations | ’Die away’ | Classically sudden, but often ‘die away’ |
| Heart rate | < 140/min | > 160/min |
| Associated symptoms | Paraesthesia due to hyperventilation | Chest pain Breathlessness Dizziness Syncope |
| Ways of terminating attacks | Relaxation | Breath holding Valsalva’s manoeuvre |
DIZZINESS AND SYNCOPE
These symptoms may have a cardiovascular or a neurological cause. Remember that cerebral hypoxia, however caused, may lead to a seizure, and that can make the differentiation between cardiac and neurological syncope very difficult. Syncope is defined as ‘a transient loss of consciousness characterized by unresponsiveness and loss of postural tone, with spontaneous recovery and not requiring specific resuscitative intervention’.
Figure 2.1 shows an EEG that was being recorded in a 46-year-old woman with episodes of limb shaking, suspected of being generalized tonic-clonic seizures. She lost awareness during events, and had violent limb shaking for several seconds as she came round. She felt nauseated, but was rapidly reorientated. By chance, she had one of her ‘attacks’ while her EEG was being recorded, and from the ECG being routinely recorded in parallel, it became clear that the problem was not seizures, but periods of asystole – in this case lasting about 15 s. The numbered arrows in Figure 2.1 mark significant features. The recording begins with a routine period of hyperventilation, with the EEG showing an eye blink in the anterior leads and the ECG showing sinus rhythm. There are then (at arrow 1 on the record) one (or possibly two) ventricular extrasystoles, followed by a narrow complex beat (probably sinus) and another ventricular extrasystole, with a different configuration from the previous ones. Asystole follows, and after 7–8 s (at arrow 2) there is global EEG slowing, and the patient became unresponsive. After 4 s (at arrow 3), there is global attenuation (reduction in signals) in the EEG and after another 3 s, there is an escape beat whose morphology suggests a ventricular origin. This is followed by a beat with a narrow QRS complex and possibly an inverted T wave, and then there is gross artefact due to the ECG lead being checked. During that period, sinus rhythm was restored. There was then (at arrow 4) global EEG slowing for 5 s, followed by (at arrow 5) violent limb thrashing for about 12 s as the patient regained consciousness – these movements were not clonic, and were thought to represent anxiety or fear. Normal EEG and ECG activity were then resumed (at arrow 6).
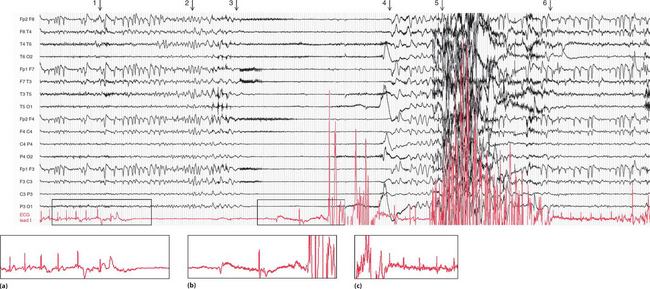
Fig. 2.1 EEG recorded during a syncopal attack
Note
•EEG and ECG lead I (lower trace)
• Paper speed five times normal ECG speed
• (b) Asystole followed by an escape beat, a narrow complex beat, and gross artefact
• (c) Sinus rhythm restored, with a period of limb thrashing before resumption of a normal record
Courtesy of Dr A. Michell, Addenbrooke’s Hospital, Cambridge
Some causes of syncope are summarized in Box 2.1.
Table 2.2 shows some clinical features of syncope, and possible causes.
Table 2.2
Diagnosis of causes of syncope
| Symptoms and signs | Possible diagnosis |
| Family history of sudden death | Long QT syndrome, Brugada syndrome, hypertrophic cardiomyopathy |
| Caused by unpleasant stimuli, prolonged standing, hot places (situational syncope) | Vasovagal syncope |
| Occurs within seconds or minutes of standing | Orthostatic hypotension |
| Temporal relation to medication | Orthostatic hypotension |
| Occurs during exertion | Obstruction to blood flow (e.g. aortic stenosis, pulmonary hypertension) |
| Occurs with head rotation or pressure on neck | Carotid sinus hypersensitivity |
| Confusion for more than 5 min afterwards | Seizure |
| Tonic-clonic movements, automatism | Seizure |
| Frequent attacks, usually unobserved, with somatic symptoms | Psychiatric illness |
| Symptoms or signs suggesting cardiac disease | Cardiac disease |
PHYSICAL EXAMINATION
If the patient has no symptoms at the time of the examination, look for:
• Evidence of any heart disease that might cause an arrhythmia
• Evidence of non-cardiac disease that might cause an arrhythmia
• Evidence of cardiovascular disease that might cause syncope without an arrhythmia
• Evidence (from the history or examination) of neurological disease.
THE ECG
Even when the patient is asymptomatic, the resting ECG can be very helpful, as summarized in Table 2.3.
Table 2.3
ECG features between attacks of palpitations or syncope
| ECG appearance | Possible cause of symptoms |
| ECG completely normal | Symptoms may not be due to a primary arrhythmia – consider anxiety, epilepsy, atrial myxoma or carotid sinus hypersensitivity |
| ECGs that suggest cardiac disease | Left ventricular hypertrophy or left bundle branch block – aortic stenosis Right ventricular hypertrophy – pulmonary hypertension Anterior T wave inversion – hypertrophic cardiomyopathy |
| ECGs that suggest intermittent tachyarrhythmia | Left atrial hypertrophy – mitral stenosis, so possibly atrial fibrillation Pre-excitation syndromes Long QT syndrome Flat T waves suggest hypokalaemia Digoxin effect – ?digoxin toxicity |
| ECGs that suggest intermittent bradyarrhythmia | Second degree block First degree block plus bundle branch block Digoxin effect |
SYNCOPE DUE TO CARDIAC DISEASE OTHER THAN ARRHYTHMIAS
The ECG may indicate that syncopal attacks have a cardiovascular cause other than an arrhythmia.
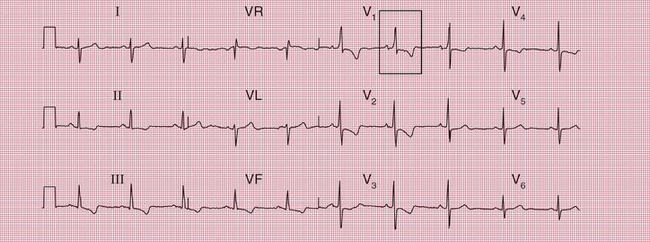
ECG evidence of left ventricular hypertrophy or of left bundle branch block may suggest that syncope is due to aortic stenosis. The ECGs in Figures 2.2 and 2.3 were recorded from patients who had syncopal attacks on exercise due to severe aortic stenosis.
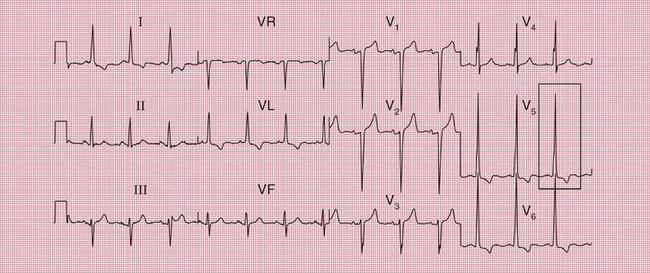

Fig. 2.2 Left ventricular hypertrophy
Note
• Bifid P waves suggest left atrial hypertrophy (best seenin leads V4–V5)
• Tall R waves and deep S waves
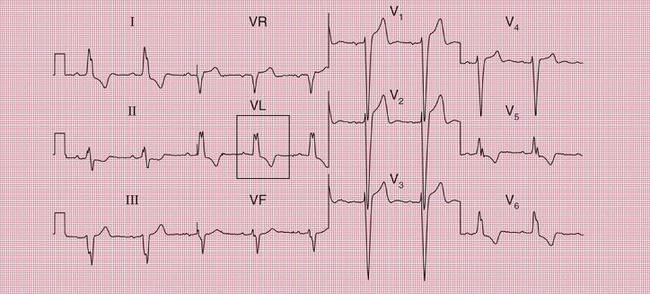

Fig. 2.3 Left bundle branch block
Note
ECG evidence of right ventricular hypertrophy suggests thromboembolic pulmonary hypertension. The ECG in Figure 2.4 is that of a middle-aged woman with dizziness on exertion, due to multiple pulmonary emboli.
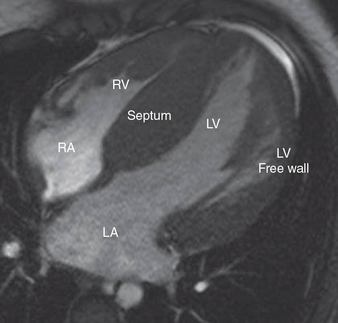
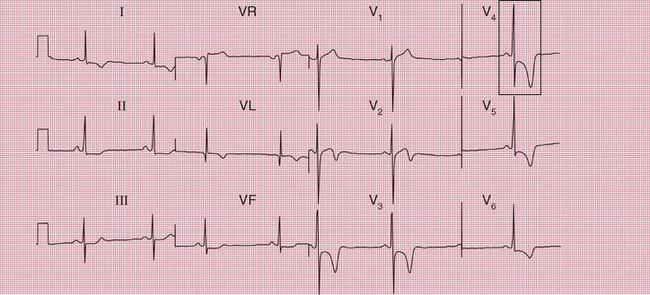
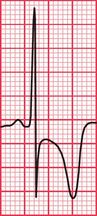
Syncope due to hypertrophic cardiomyopathy ( Fig. 2.5) may be associated with a characteristic ECG ( Fig. 2.6) that resembles that of patients with an anterior non-ST segment elevation myocardial infarction (NSTEMI) (compare with Fig. 5.23, p. 240). With hypertrophic cardiomyopathy, the T wave inversion is usually more pronounced than with an NSTEMI, but differentiation really depends on the clinical picture, not on the ECG appearance. Hypertrophic cardiomyopathy can cause syncope due to obstruction to outflow from the left ventricle, or can cause symptomatic arrhythmias.
PATIENTS WITH POSSIBLE TACHYCARDIAS
MITRAL STENOSIS
Mitral stenosis leads to atrial fibrillation, but when the heart is still in sinus rhythm the presence of the characteristics of left atrial hypertrophy on the ECG may give a clue that paroxysmal atrial fibrillation is occurring ( Fig. 2.7).
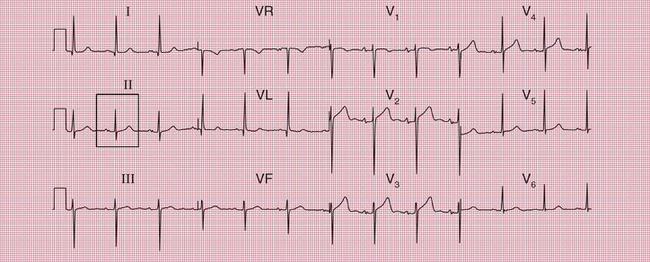
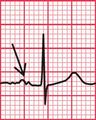
Fig. 2.7 Left atrial hypertrophy
Note
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree