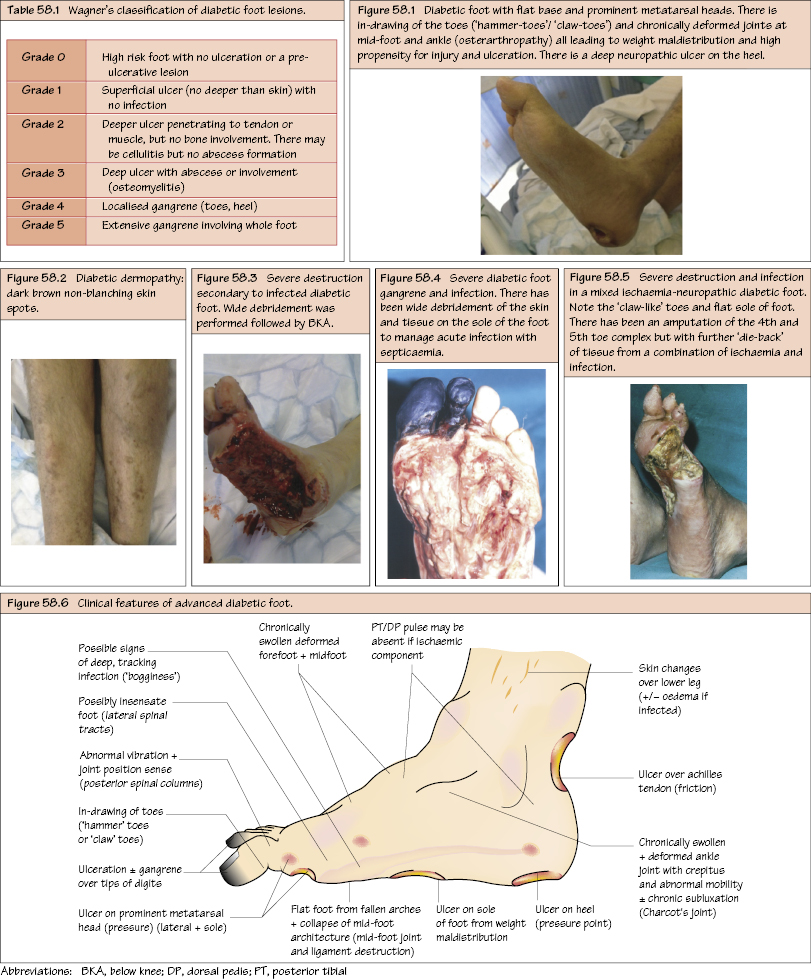
The Diabetic Foot The diabetic foot represents a special problem for vascular surgeons and is truly a condition requiring a multidisciplinary team approach, including diabetology, ophthalmology, nephrology, podiatry, tissue viability and diabetic nurse specialists. Most common aetiology in both diabetic foot and diabetic ulceration. Pathophysiology. Diabetic neuropathy is complex. Often there is loss of the posterior spinal columns resulting in decreased joint position and vibration sense. Eventually there is a loss of the lateral spinal tracts leading to decreased sensation loss for pain and temperature, leaving the foot vulnerable to even trivial injury. In addition, microvascular disease affecting the peripheral nerves (including mononeuritis multiplex) leads to further loss of sensation and protective reflexes. Autonomic neuropathy, although leading to vasodilatation in the feet, also gives rise to microvascular shunting within cutaneous tissue, which is also thought to contribute to skin vulnerability, leading to ulceration and poor healing ability. Pathophysiology. Both macrovascular and microvascular
Aetiology
Neuropathy
Clinical Features
Vasculopathy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


