Sinus tachycardia with bundle branch block
SVT with aberrancy due to conduction slowing or bundle branch block
SVT with anterograde conduction over an accessory AV pathway
Ventricular pacing
Electrolyte imbalances such as hyperkalemia
Electrocardiographic artifact
Direct proarrhythmic effect of antiarrhythmic agents
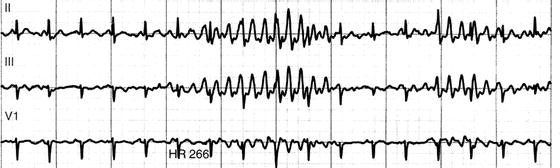
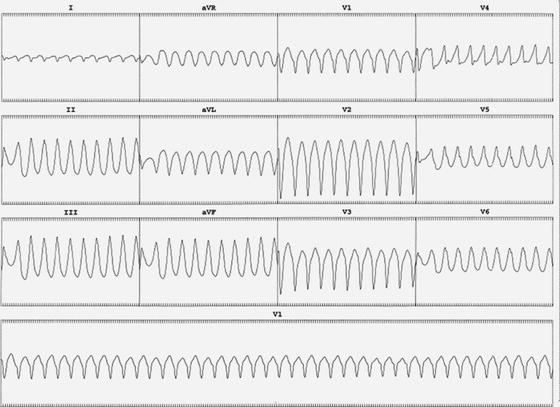
Figure 19.1 Wide complex tachycardia as captured on hospital telemetry. However, upon closer inspection, of all leads this is simply artifact.
19.3 VENTRICULAR TACHYCARDIA
Ventricular tachycardia is the cause of WCT in >80% of patients. Moreover, if faced with a WCT in the setting of a previous myocardial infarction, clinicians can assume the cause is ventricular tachycardia >96% of the time. In general, making an assumption of ventricular tachycardia when uncertainty exists can be a prudent method of treatment. Hemodynamic stability is not an indicator of SVT versus VT and should not be taken into consideration during evaluation.
19.4 SUPRAVENTRICULAR MECHANISMS
With SVT, widening of the QRS complex occurs when conduction in the normal conduction system is slowed or blocked. This condition may be pre-existing, or due to a transient bundle branch block (BBB) (Figure 19.2). A BBB occurring as a result of tachycardia is often referred to as “aberrancy.” In this situation, one bundle branch may be ready to conduct another impulse from the atrium; however, the other bundle branch has not fully repolarized, resulting in delayed conduction and a widened beat due to cell-to-cell depolarization.
Aberrancy can occur with any type of supraventricular arrhythmia. The Ashman phenomenon is a unique form of aberrancy classically seen in atrial fibrillation in which a long RR cycle is followed immediately by a short RR cycle, and the second beat of that combination typically shows a right bundle branch block (RBBB) pattern due to refractoriness in that bundle branch. When a WCT occurs in a brief salvo in the setting in atrial fibrillation, Ashman beating should be suspected (Figure 19.3).
Figure 19.2 Atrial fibrillation with aberrant conduction of one beat. The wide QRS beat occurs as the right bundle is refractory due to the short coupling interval otherwise known as a “long short sequence.”
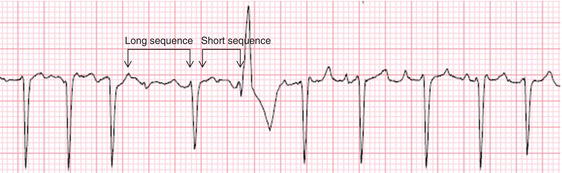
Figure 19.3 Atrial fibrillation with rapid ventricular response at approximately 159 beats/min. Ashman phenomenon is present, with RBBB starting immediately after a short RR cycle.
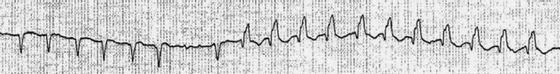
Figure 19.4 A patient with Wolf Parkinson White pattern on ECG. Note the delta wave (arrow) which depicts early ventricular depolarization down the accessory pathway, resulting in a wide QRS and short PR interval.
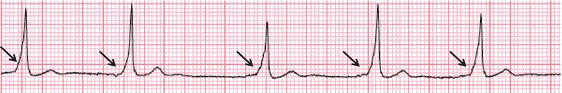
With Wolff-Parkinson-White patterns, AV conduction occurs anterogradely over two pathways: the AV node and an accessory pathway (Figure 19.4). The accessory pathway facilitates the maintenance of what are commonly known as AV reentrant (or reciprocating) tachycardias. These tachycardias can manifest with either a narrow or wide complex QRS, depending on which pathway conducts in an anterograde fashion. With orthodromic AV reentrant tachycardia (the most common type), the AV node conducts anterogradely and the accessory pathway conducts in a retrograde fashion, resulting in a narrow complex tachycardia (unless a BBB is also present). Conversely, if the accessory tract conducts in an anterograde fashion with retrograde conduction occurring over the AV node (antidromic AV reentrant tachycardia), a wide complex pre-excited SVT results which can be difficult to differentiate from VT without an electrophysiology study.
A rapid (>220 bpm) irregular WCT is pathognomonic for pre-excited atrial fibrillation due to a rapidly conducting bypass tract. Patients with WPW who present with atrial fibrillation should not be given AV nodal blocking agents as this can result in excessive ventricular rates and subsequent ventricular fibrillation.
19.5 BENIGN FORMS
It is important to recognize that benign forms of idiopathic VT do exist clinically and are amenable to catheter ablation for symptomatic relief. Ventricular tachycardia arising from the right and left outflow tracts can be commonly seen in young individuals. Recognition of idiopathic VT is important because it is typically seen in patients with structurally normal hearts and, in most cases, is not associated with an increased risk for sudden death. These arrhythmias can be identified by their characteristic 12-lead ECG and clinical presentation. Repetitive monomorphic VT is characterized by salvos of nonsustained VT or paroxysmal sustained VT often triggered by exercise or catecholamines. It typically arises from the right ventricular outflow tract (RVOT). The characteristic 12-lead ECG in RVOT VT is a WCT with a LBBB pattern and tall monophasic R waves in the inferior leads (Figure 19.5), with a transition point (R ≥ S) that occurs late in the precordial leads. In the vast majority of cases, these outflow tract VTs are associated with an excellent prognosis and ablation should be considered.
Figure 19.5 Right ventricular outflow tract tachycardia. LBBB pattern is present with tall R waves in leads II, III, aVF.
19.6 DIAGNOSIS
WCTs often arise in, and herald the onset of, an emergent situation. As such, taking a comprehensive history, performing a detailed physical examination, and inspecting prior tracings are often not feasible nor appropriate if the patient is clinically unstable. All clinicians must understand that if a patient has a history of coronary artery disease, VT is the etiology of WCT >98% of the time and emergent evaluation is necessary.
19.6.1 History
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


