Chapter 1 The ABCDs of Emergency Cardiovascular Care
Introduction
Heart disease is the leading cause of death for both men and women in the United States. In 2005, approximately 920,000 persons in the United States had a myocardial infarction (heart attack).1 In the United States, someone has a heart attack every 34 seconds.2 It has been estimated that about 300,000 individuals in the United States experience a cardiac arrest each year and fewer than 15% survive.3–5
Risk Factors for Coronary Artery Disease
[Objective 1]
Cardiovascular disease (CVD) is a collection of conditions that involve the circulatory system, which contains the heart (cardio) and blood vessels (vascular), and that include congenital CVDs. Approximately one in three American adults has one or more types of CVD.2 Heart disease is a broad term that refers to conditions that affect the heart. Coronary heart disease (CHD) refers to disease of the coronary arteries and their resulting complications, such as angina pectoris and acute myocardial infarction. According to the Centers for Disease Control and Prevention, CHD is the most common type of heart disease.6 Coronary artery disease (CAD) affects the arteries that supply the heart muscle with blood.
The prevention of CVD requires the management of risk factors. Risk factors are traits and lifestyle habits that may increase a person’s chance of developing a disease. More than 300 risk factors have been associated with CHD and stroke. Major risk factors meet three criteria7:
Some risk factors can be modified, which means that they can be changed or treated. Risk factors that cannot be modified are called “nonmodifiable” or “fixed” risk factors. Contributing risk factors are thought to lead to an increased risk of heart disease, but their exact role has not been defined (Table 1-1).
TABLE 1-1 Cardiovascular Disease Risk Factors
| Nonmodifiable (Fixed) Factors | Modifiable Factors | Contributing Factors |
|---|---|---|
Sudden Cardiac Death
[Objectives 2, 3, 4]
Cardiovascular collapse is a sudden loss of effective blood flow that is caused by cardiac and/or peripheral vascular factors that may reverse spontaneously (such as syncope) or only with interventions (such as cardiac arrest).8 Cardiopulmonary (cardiac) arrest is the absence of cardiac mechanical activity, which is confirmed by the absence of a detectable pulse, unresponsiveness, and apnea or agonal, gasping breathing. The term cardiac arrest is more commonly used than cardiopulmonary arrest when referring to a patient who is not breathing (or who is only gasping) and who has no pulse. Gasping is abnormal breathing and should not be interpreted as a sign of effective breathing.
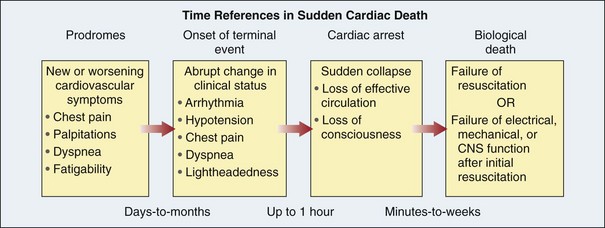
Sudden cardiac death (SCD) is a natural death of cardiac cause that is preceded by an abrupt loss of consciousness within one hour of the onset of an acute change in cardiovascular status.8 Approximately half of cardiac deaths occur before patients reach a hospital.9,10 SCD is often the patient’s first and only symptom of heart disease.11–13 For others, warning signs may be present up to 1 hour before the actual arrest (Figure 1-1). Because of irreversible brain damage and dependence on life support, some patients may live days to weeks after resuscitation from the cardiac arrest before biologic death occurs. These factors influence the interpretation of the 1-hour definition of SCD.8
Heart rhythms that may be observed in a cardiac arrest include the following:
Chain of Survival
[Objective 5]
The Chain of Survival represents the ideal series of events that should take place immediately after the recognition of the onset of sudden cardiac illness. The Chain consists of five key steps that are interrelated. Following these steps gives the victim the best chance of surviving a heart attack or sudden cardiac arrest. The links in the Chain of Survival for adults include early recognition and activation, early CPR, early defibrillation, effective advanced life support (ALS), and integrated post–cardiac arrest care.14 Because time is critical when dealing with a victim of SCD, a weak or missing link in the Chain of Survival can reduce the likelihood of a positive outcome.
Early Recognition and Activation
The first link in the Chain of Survival is early recognition and activation. Although warning signs are often absent, the sudden onset of chest pain, difficulty breathing, or palpitations and other symptoms of abnormal heart rhythms may precede the onset of cardiac arrest.8 In a 2005 study1, a telephone survey of U.S. civilian adults was conducted and respondents were questioned about their awareness of the five major warning signs and symptoms of a heart attack. Respondent awareness of each of the warning signs varied: pain or discomfort in the jaw, neck, or back (48%); feeling weak, lightheaded, or faint (62%); chest pain or discomfort (92%); pain or discomfort in the arms or shoulder (85%); and shortness of breath (93%). Only 27% were aware of all major symptoms and knew to call 9-1-1 if they thought someone was having a heart attack. The results of this study emphasize the importance of teaching the public to recognize the early warning signs of a heart attack and the need for prompt attention, and to subsequently improve the rate of survival from cardiac arrest.
When a cardiac emergency occurs, the individual must identify his or her signs and symptoms, recognize that they are related to a heart condition, and seek medical assistance. Time delays occur from the call for assistance to the arrival of assistance and from the arrival of assistance to arrival at the hospital. Studies have found that about one third to one half of patients delay for more than 4 hours before calling for help, and that even greater delays in seeking help occur among female patients, older patients, nonwhite patients, and those who have a history of angina, heart failure, diabetes, and hypertension.15
Public education must include the early recognition of a patient’s cardiac emergency and knowledge of how to gain rapid access to the emergency medical services (EMS) system (usually by telephone) via EMS dispatchers. When a call is placed to 9-1-1 (or similar emergency number), rapid recognition by EMS dispatchers of the bystander’s description of a potential heart attack or cardiac arrest is important (Figure 1-2). Dispatchers quickly send appropriately trained and equipped EMS personnel to the scene. With appropriate training, EMS dispatchers provide telephone instructions to bystanders. They can ask bystanders to find out if the patient is unresponsive and if normal breathing is present. They can also provide telephone CPR instructions when needed until EMS personnel arrive.
Patients who experience a cardiac arrest in the hospital often show signs of deterioration several hours before the arrest.16 Early recognition of the critically ill patient and activation of a Medical Emergency Team (MET) (also known as a Rapid Response Team) may prevent the development of cardiac arrest and improve patient outcome. A MET typically consists of a physician and nurse with critical care training who are available at all times. They are summoned by other hospital staff based on well-defined criteria for activation of the team.
Early Cardiopulmonary Resuscitation
[Objective 5]
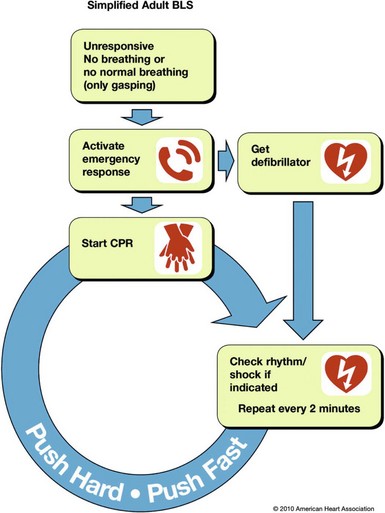
Cardiopulmonary resuscitation is a part of BLS. BLS includes the recognition of signs of cardiac arrest, heart attack, stroke, and foreign body airway obstruction (FBAO); the relief of FBAO; CPR; and defibrillation with an automated external defibrillator (AED) (Box 1-1).
Box 1-1 Components of Basic Life Support
Blood flow through the vessels of the body (including the coronary vessels) is determined by driving pressure and vascular resistance to flow.17 Aortic blood pressure and right atrial pressure determine the driving pressure through the coronary arteries. In the coronary arteries, vascular resistance is determined by the diameter of the coronary vessels and the degree of external compression caused by myocardial contraction (systole) and relaxation (diastole). Most coronary blood flow occurs during diastole because the coronary vessels are compressed as the myocardium contracts (systole). Under normal conditions, the coronary arteries can dilate or constrict to adjust (autoregulate) blood flow at the level of the arterioles in accordance with tissue needs. In the coronary circulation, autoregulation maintains constant blood flow at perfusion pressures (mean arterial pressure) between 60 and 180 mm Hg when other influencing factors are held constant.18
During cardiac arrest, compressing the chest compresses the heart and increases intrathoracic pressure, creating blood flow and enabling the delivery of oxygen to the brain and heart. When performing chest compressions, systole is the chest compression phase and diastole is the release phase.19 Myocardial blood flow is dependent on coronary perfusion pressure, which is generated when performing external chest compressions. Coronary perfusion pressure is a key determinant of the success of resuscitation, and adequate cerebral and coronary perfusion pressures are critical to neurologically normal survival.19 Because it takes time to build up cerebral and coronary perfusion pressures, the stopping of chest compressions for even a few seconds causes cerebral and coronary perfusion pressures to fall quickly and dramatically, thereby reducing blood flow to the brain and heart. When chest compressions are stopped during cardiac arrest, no blood flow is generated; this is referred to as no flow time. Even after compressions are resumed, several chest compressions are needed to restore coronary perfusion pressure.
Researchers have confirmed that when an adult develops VF and suddenly collapses, his or her lungs, pulmonary veins, left heart, aorta, and the arteries contain oxygenated blood.19,20 The delivery of oxygen to tissues with CPR is limited more by blood flow and low cardiac output than by arterial oxygen content.21,22 The low cardiac output associated with CPR results in low oxygen uptake from the lungs, which in turn reduces the need to ventilate the patient during this low-flow state.23
After a bystander or healthcare professional determines that CPR is indicated, chest compressions should be the initial action performed (instead of opening the airway or giving ventilations) when starting CPR in victims of sudden cardiac arrest (Figure 1-3).24 Performing chest compressions before ventilations enables better delivery of the oxygen that is already present in the lungs and arterial circulation to the heart and brain.25
It has been estimated that cardiac output is approximately 25% to 33% of normal during CPR.14 Therefore the quality of chest compressions is an important factor in the effectiveness of CPR (Figure 1-4).22 High-quality chest compressions require the following24:
Early Defibrillation
When an individual experiences a cardiac arrest, the likelihood of successful resuscitation is affected by the speed with which CPR and defibrillation are performed. When a cardiac arrest is witnessed and the patient’s heart rhythm is VF, the patient’s survival rate decreases 7% to 10% per minute until defibrillation if no CPR is provided.26,27 The decrease in survival rates is less rapid (averaging 3% to 4% per minute from collapse to defibrillation) when bystander CPR is provided.27,28 Although early defibrillation can improve outcome,29,30 most patients do not receive or are not candidates for early defibrillation.5
Since 1995, the American Heart Association has promoted the development of lay rescuer AED programs to improve survival from out-of-hospital sudden cardiac arrest. An automated external defibrillator is a machine with a sophisticated computer system that analyzes the patient’s heart rhythm (Figure 1-5). The AED uses an algorithm to distinguish shockable rhythms from nonshockable rhythms. If the AED detects a shockable rhythm, it provides visual and auditory instructions to the rescuer to deliver an electrical shock. Defibrillation performed by citizens (such as flight attendants, casino security officers, athletic or golf club employees, and ushers at sporting events) at the scene is called public access defibrillation. AEDs permit bystanders to perform three of the five links of the Chain of Survival. In the first few minutes after defibrillation, the cardiac rhythm may be slow and the pumping effectiveness of the patient’s heart may be inadequate. CPR may be needed for several minutes after defibrillation until adequate heart function resumes.28
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree