9 Tetralogy of Fallot with Absent Pulmonary Valve Syndrome
I. CASE
A. Fetal echocardiography findings
1. The fetal echo reveals situs solitus of the atria, levocardia, left aortic arch, heart rate of 140 bpm.
2. Estimated fetal gestational age (GA) is 25.5 weeks.
3. There was cardiomegaly with increased cardiothoracic ratio (50%) and dextroposition of the heart.
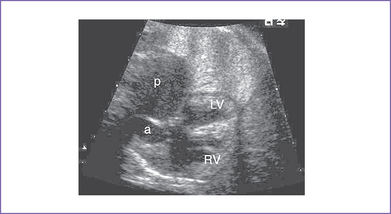
4. The four-chamber view is abnormal, with a large perimembranous subaortic ventricular septal defect (VSD), large overriding aorta, and massively dilated pulmonary artery (Fig. 9-1).
5. The pulmonary valve is dysplastic with no identifiable leaflets, small pulmonary annulus (1.7 mm), and very dilated and pulsatile main pulmonary artery and branches.
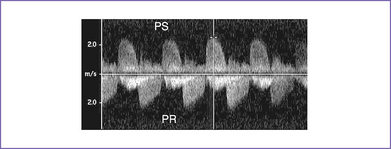
6. There is pulmonary stenosis with a peak velocity of 2.2 m/s (lower panel) and pulmonary valve regurgitation. In other words, there is to (systolic) and fro (diastolic) flow through this dysplastic valve, with severe pulmonary regurgitation (Fig. 9-2).
7. There is holosystolic tricuspid regurgitation with a dP/dt (change in pressure per change in time) of 500 mm Hg per second.
8. The foramen ovale is patent, with unrestricted right-to-left shunt.
9. Aortic valve annulus is 6 mm.
10. A ductus arteriosus cannot be identified.
11. The pulmonary venous drainage is normal.
12. Tei index (myocardial performance index).
b. Left ventricle (LV) Tei index is 0.36.
13. The umbilical artery flow pattern is normal.
14. Ductus venosus flow is abnormal, with a wave reversal (3 mm).
D. Fetal management and counseling
1. Management: Diagnosis of tetralogy of Fallot (TOF) should prompt referral for the following:
a. Thorough anatomic examination by ultrasound.
2. Follow-up included serial antenatal studies at weekly intervals.
a. Cardiac function should be monitored by Tei index, by dP/dt if sufficient tricuspid regurgitation develops (3 m/s), and by tissue Doppler (if available).
b. Development of congestive heart failure (CHF) can indicate RV dysfunction secondary to severe pulmonary regurgitation. Severe AV or semilunar valve regurgitation, particularly if it influences filling of the other ventricle, can be very poorly tolerated. Thus, Ebstein’s anomaly and absent pulmonary valves can cause CHF.
E. Delivery
1. If the fetus remains well compensated, delivery should be at term in a tertiary care center.
2. Depending upon the severity of the pathology, which can include degree of cardiomegaly and degree of pulmonary artery dilation, the baby might require ventilatory support after birth as a result of compression of the tracheobronchial tree and coexisting tracheomalacia and bronchiomalacia.
F. Neonatal management
a. Medical management of affected babies includes supporting them from a respiratory standpoint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree