The aim of this work was to analyze temporal trends in clinical presentation, treatment methods, and outcomes of patients in Poland with non–ST-segment elevation myocardial infarction (NSTEMI) from 2004 to 2010. A total of 90,153 patients with NSTEMI enrolled in the Polish Registry of Acute Coronary Syndromes (PL-ACS) from 2004 to 2010 were analyzed. The main outcome measure was all-cause mortality after 12 months, identified from official mortality records. The percentage of admissions for NSTEMI among all acute coronary syndromes increased from 24% in 2004 to 38% in 2010 (p <0.0001). From 2004 to 2010, the percentage of invasive treatment for NSTEMI increased significantly, almost threefold, to 83% (p <0.0001). The frequency of recurrent myocardial infarction and stroke during hospitalization decreased significantly over the years, while the frequency of major bleeding increased. Twelve-month mortality decreased significantly throughout the time period, from 19.1% to 14.5%, but was stable in patients treated invasively and slightly higher in the last years in patients treated noninvasively. The invasive treatment of NSTEMI (relative risk 0.62, 95% confidence interval 0.57 to 0.67, p <0.0001), together with the pharmacotherapy recommended by the guidelines, had a significant impact on reducing 12-month mortality in a multifactor analysis. In conclusion, the distinct improvement in the short- and long-term prognoses of patients with NSTEMI may be in part the result of the popularization of invasive treatment and the optimization of pharmacotherapy.
In recent years, the European Society of Cardiology guidelines for treating patients with non–ST-segment elevation acute coronary syndromes (ACS) have focused on the prompt implementation of invasive treatment strategies, especially in patients with non–ST-segment elevation myocardial infarction (NSTEMI). The frequency of invasive treatment for ACS differs among countries, but there has been a constant increase in recent years in the percentage of patients referred for urgent coronary angiography, including NSTEMI. In Poland, the number of invasive wards has recently increased significantly (to >120 centers), which should result in a stable increase in the availability of invasive treatment. The mortality of patients with NSTEMI is similar to that of patients with ST-segment elevation myocardial infarction, so it is important to implement appropriate treatment methods, as recommended by the guidelines. The aim of this work was to analyze temporal trends in clinical presentation, treatment methods, and outcomes of patients with NSTEMI in Poland from 2004 to 2010.
Methods
We used data from the Polish Registry of Acute Coronary Syndromes (PL-ACS). The method and the analysis of the first 100,193 patients have been previously described. In brief, PL-ACS is an ongoing, nationwide, multicenter, prospective, observational study of consecutively hospitalized patients with the entire spectrum of ACS in Poland. The registry is a joint initiative of the Silesian Center for Heart Diseases and the Polish Ministry of Health. The National Health Fund, a nationwide public health insurance institution in Poland, provides logistic support. All Polish citizens are required to have National Health Fund insurance policies. The pilot phase of the registry commenced in October 2003 in Silesia. In the following months, all other regions were opened.
Hospitals were invited to enter the registry if they had 1 of the following wards: coronary care, cardiology, cardiac surgery, internal medicine, or an intensive care unit. They were also invited to join if they hospitalized ≥10 patients with ACS per year.
A detailed protocol with inclusion and exclusion criteria, methods and logistics, and definitions of all fields in the registry data set was prepared before the registry was started. However, the protocol was revised in May 2005 to be compatible with the Cardiology Audit and Registration Data Standards. Nevertheless, the PL-ACS case report form covers only part of the Cardiology Audit and Registration Data Standards data set.
According to the protocol, all admitted patients with suspected ACS were screened for eligibility to enter the registry, but they were not enrolled until ACS were confirmed. The patients were then classified as having unstable angina, NSTEMI, or ST-segment elevation myocardial infarction. NSTEMI was defined as the absence of ST-segment elevation consistent with infarction of ≥2 mm in contiguous chest leads and/or ST-segment elevation of ≥1 mm in ≥2 standard leads or a new left bundle branch block and the presence of positive cardiac necrosis markers. If a patient was hospitalized during the same ACS episode in >1 hospital (transferred patient), all hospitals were required to complete the registry data. These hospitalizations were linked together during data management and were subsequently analyzed as a single case of ACS.
All-cause mortality data with the accompanying exact dates of deaths were obtained from official mortality records from the National Health Fund. Vital status at 12 months after NSTEMI was available for all patients.
Continuous parameters are expressed as either mean ± SD or median (interquartile range), depending on data distribution. Quality parameters are expressed as percentages. In addition, the absolute percentage difference is given for 2009 to 2010 versus 2004 to 2005 with a 95% confidence interval. The significance of the time trends in the studied years was evaluated using the Cochran-Armitage test for parametric variables and the Jonckheere-Terpstra test for continuous variables. The significance of the trend in years and the invasive and pharmacologic treatment methods was tested with multifactor Cox proportional-hazards regression, taking into account the differences in patients’ initial characteristics. The results are expressed as relative risk and 95% confidence intervals. A 2-tailed p value ≤0.05 was considered significant. Calculations were made using Statistica version 7.1 (StatSoft, Inc., Tulsa, Oklahoma), MedCalc (MedCalc Software, Mariakerke, Belgium), and SPSS version 17.0 (SPSS, Inc., Chicago, Illinois).
Results
From 2004 to 2010, a total of 90,153 patients hospitalized for NSTEMI in 464 Polish hospitals, of which 103 (22%) were invasive cardiology centers, were enrolled in PL-ACS. The percentage of NSTEMI admissions among all patients with ACS (a total of 273,639 patients) increased from 24% in 2004 to 38% in 2010 (p <0.0001).
Table 1 lists and Figure 1 depicts the changes in clinical characteristics of patients with NSTEMI over time. The mean patient age remained unchanged. The percentage of hospitalized women, patients with hypercholesterolemia, smokers, patients with histories of myocardial infarction, and patients with coronary artery bypass grafts decreased significantly. In 2009 and 2010, patients with either cardiac arrest before admission or significant hemodynamic disorders (pulmonary edema and cardiogenic shock) on admission were significantly less frequently admitted than in 2004 and 2005. However, the admission frequency of patients with post–percutaneous coronary intervention (PCI) NSTEMI and diabetes, hypertension, and obesity increased.
| Variable | 2004–2005 (n = 20,192) | 2009–2010 (n = 24,890) | % Difference in Frequency (95% Confidence Interval) | p Value for Trend, 2004–2010 |
|---|---|---|---|---|
| Age (years) | 67.7 ± 11.8 | 67.8 ± 11.6 | — | 0.35 |
| Women | 40.7% | 38.6% | −2.1 (−3.0 to −1.2) | <0.0001 |
| Diabetes mellitus | 27.3% | 30.1% | 2.8 (1.9 to 3.6) | <0.0001 |
| Hypertension | 70.4% | 75.7% | 5.3 (4.4 to 6.1) | <0.0001 |
| Hypercholesterolemia | 44.2% | 42.1% | −2.1 (−3.1 to −1.2) | <0.0001 |
| Current smoking | 25.4% | 22.4% | −3.0 (−4.1 to −2.0) | <0.0001 |
| Obesity (body mass index ≥30 kg/m 2 ) | 19.9% | 20.5% | 0.6 (−0.1 to 1.4) | 0.019 |
| Previous myocardial infarction | 25.1% | 17.8% | −7.3 (−8.0 to −6.5) | <0.0001 |
| Previous PCI | 2.8% | 8.3% | 5.5 (5.1 to 5.9) | <0.0001 |
| Previous coronary artery bypass grafting | 5.2% | 3.7% | −1.5 (−1.9 to −1.1) | <0.0001 |
| Cardiac arrest before admission | 2.2% | 1.2% | −1.0 (−1.2 to −0.7) | <0.0001 |
| Killip class 2 on admission | 11.0% | 14.4% | 3.4 (2.8 to 4.0) | <0.0001 |
| Killip class 3 on admission | 7.2% | 3.8% | −3.4 (−3.8 to −3.0) | <0.0001 |
| Killip class 4 on admission | 3.9% | 2.1% | −1.8 (−2.1 to −1.5) | <0.0001 |
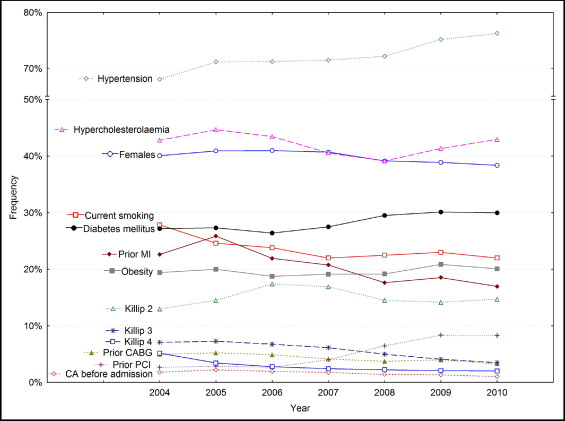
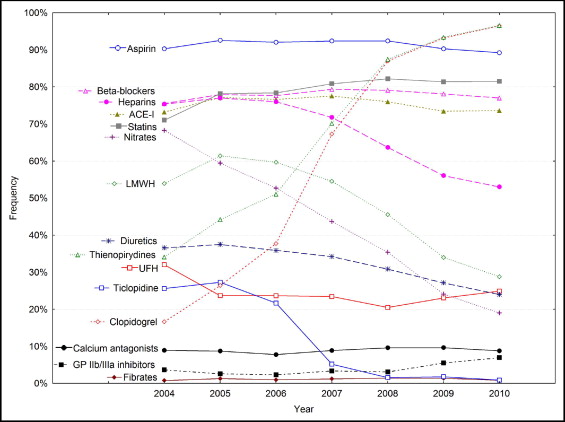
Table 2 lists and Figure 2 depicts the medications administered during hospitalization in patients with NSTEMI. Interestingly, there was a significant increase in the use of thienopyridines (from 42% in 2004 and 2005 to 95% in 2009 and 2010). From 2007 to 2010, the primary drug administered during treatment was almost exclusively clopidogrel. Twice as many patients were treated with glycoprotein IIb/IIIa inhibitors than at the start of the registry (6% vs 3% in 2004 and 2005). In 2009 and 2010, patients were significantly less frequently treated with heparins (with the exception of heparin during PCI), nitrates, and diuretics. There was an increase in the frequency of use of statins and a slight decrease in the frequency of use of angiotensin-converting enzyme inhibitors.
| Variable | 2004–2005 (n = 20,192) | 2009–2010 (n = 24,890) | % Difference in Frequency (95% Confidence Interval) | p Value for Trend, 2004–2010 |
|---|---|---|---|---|
| Aspirin | 92.0% | 89.8% | −2.2 (−2.7 to −1.7) | <0.0001 |
| Thienopyridines | 41.8% | 94.8% | 53.1 (52.5 to 53.6) | <0.0001 |
| Ticlopidine | 26.9% | 1.4% | −25.5 (−25.8 to −25.2) | <0.0001 |
| Clopidogrel | 24.0% | 94.7% | 70.7 (70.1 to 71.2) | <0.0001 |
| Glycoprotein IIb/IIIa inhibitors | 2.9% | 6.2% | 3.3 (3.0 to 3.7) | <0.0001 |
| Heparins | 76.6% | 54.7% | −21.9 (−22.8 to −21.1) | <0.0001 |
| Low–molecular weight heparin | 59.6% | 31.6% | −28.0 (−28.9 to −27.1) | <0.0001 |
| Unfractionated heparin | 25.7% | 23.9% | −1.8 (−2.6 to −1.0) | <0.0001 |
| β blockers | 77.3% | 77.6% | 0.3 (−0.5 to 1.0) | 0.25 |
| Angiotensin-converting enzyme inhibitors | 76.2% | 73.5% | −2.7 (−3.5 to −1.9) | <0.0001 |
| Statins | 76.5% | 81.5% | 5.0 (4.2 to 5.7) | <0.0001 |
| Calcium antagonists | 8.8% | 9.3% | 0.5 (−0.0 to 1.0) | 0.0010 |
| Nitrates | 61.6% | 21.8% | −39.8 (−40.7 to −39.0) | <0.0001 |
| Fibrate | 1.16% | 1.14% | −0.01 (−0.2 to 0.2) | 0.52 |
| Diuretics | 37.3% | 25.7% | −11.6 (−12.4 to −10.7) | <0.0001 |
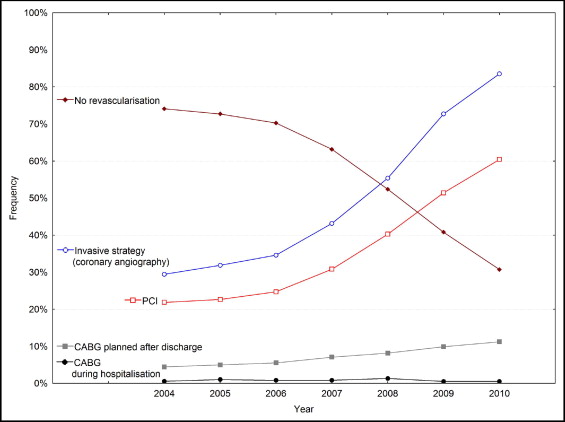
From 2004 to 2010, the percentage of patients treated invasively increased significantly, almost threefold, up to 83% in 2010 ( Table 3 , Figure 3 ) . There was a similar increase in the frequency of PCI and qualification of patients for coronary artery bypass grafting, although the percentage of bypass graft procedures performed during the initial hospitalization remained low, at <1% of patients. As a result, the percentage of patients without revascularization decreased significantly, from approximately 75% in 2004 to approximately 30% in 2010. Prehospital delay (time from onset of pain to hospital admission) did not change over the studied period in patients admitted to hospitals with no possibility of invasive treatment. The prehospital delay was approximately 5 to 6 hours ( Figure 4 ) . In patients admitted to invasive centers, the delay was approximately 2 hours longer and increased significantly from approximately 7 to 8 hours in 2009 and 2010 (p <0.0001). The door–to–coronary angiography time decreased significantly from 2.8 to 1.6 hours (p <0.0001).
| Variable | 2004–2005 (n = 20,192) | 2009–2010 (n = 24,890) | % Difference in Frequency (95% Confidence Interval) | p Value for Trend, 2004–2010 |
|---|---|---|---|---|
| Invasive strategy (coronary angiography) | 31.3% | 77.7% | 46.4 (45.6 to 47.2) | <0.0001 |
| PCI | 22.5% | 55.6% | 33.1 (32.3 to 33.9) | <0.0001 |
| Coronary artery bypass grafting during hospitalization | 0.9% | 0.5% | −0.4 (−0.7 to −0.2) | <0.0001 |
| Coronary artery bypass grafting planned after discharge | 4.9% | 10.5% | 5.7 (5.2–6.1) | <0.0001 |
| No revascularization | 73.1% | 36.2% | −36.9 (−37.7 to −36.0) | <0.0001 |
The frequency of recurrent myocardial infarction and stroke during hospitalization decreased significantly over the years, while the frequency of major bleeding increased ( Table 4 , Figure 5 ) . In-hospital mortality decreased by half over the study period. The length of hospitalization also decreased significantly. Twelve-month mortality in the entire group decreased significantly, by approximately 5%, but was stable in patients treated invasively and slightly higher in the last years for patients treated noninvasively ( Table 5 , Figure 5 ). The invasive treatment of NSTEMI, together with pharmacotherapy recommended by the guidelines, significantly reduced 12-month mortality in the multifactor analysis ( Figure 6 ) . In this analysis, the year of hospitalization was not a significant prognostic factor, although after removing the invasive treatment strategy from the model, a later year of hospitalization had a significant impact on decreasing 12-month mortality (relative risk per each subsequent year 0.93, 95% confidence interval 0.95 to 0.97, p <0.0001).



