TEE for Noncardiac Surgery
Ben Sommer1
Albert C. Perrino, Jr2
Scott T. Reeves2
1OUTLINE AUTHOR
2ORIGINAL CHAPTER AUTHORS
▪ KEY POINTS
The value of transesophageal echo cardiography (TEE) during noncardiac surgery is well established.
The most common indications for TEE during noncardiac surgery are as a rescue technique in the hemodynamically unstable patient and as a monitor in patients at risk for cardiovascular complications.
Assessments of preload and systolic function are the most valued functions of intraoperative TEE during noncardiac surgery.
Quantitative assessments of ventricular function are preferred to visual estimates.
The increasingly elderly and high-risk patient population undergoing vascular, laparoscopic, orthopedic, neurosurgical, and hepatic procedures warrants expanded use of TEE.
I. INTRODUCTION
Limited availability of echocardiographic systems and clinicians trained in TEE initially slowed the growth of TEE in noncardiac procedures.
TEE can provide rapid diagnosis in a patient not responding to standard therapies. This warrants TEE availability to most anesthetized patients.
II. INDICATIONS
Indications for TEE remain only partially defined.
Well-conducted outcome trials examining the effectiveness of TEE during noncardiac surgery are lacking and unlikely to be forthcoming.
The lack of supporting evidence is often owing to the absence of relevant studies rather than to existing evidence of ineffectiveness.
Category I indication (supported by strong evidence or expert opinion): intraoperative evaluation of acute persistent and life-threatening hemodynamic disturbances in which ventricular function and its determinants are uncertain and have not responded to treatment.
Category II indication (supported by weaker evidence and expert consensus): perioperative use in patients with increased risk of hemodynamic disturbances.
Categories I and II together remain by far the most frequent reasons for the use of intraoperative TEE during noncardiac surgery.
TEE has been shown to change intraoperative management, either surgical or medical, in up to 40% of patients. These changes include changes in medical therapy, confirming or invalidating a diagnosis, unplanned surgical reinterventions, substitution for a pulmonary artery (PA) catheter, and positioning of intravascular devices.1,2,3,4
TEE has value both as a diagnostic tool and as an intraoperative monitor over and above that achievable with radial and pulmonary arterial catheters.
TEE has value in monitoring and detecting myocardial ischemia, fluid status, and global ventricular function.
III. APPROACH
Optimization of ventricular performance during noncardiac surgery
Assessing preload
Assessing stroke volume (SV)
Echocardiographic techniques for SV measurement
Right heart SV calculation
Alternative approaches to optimizing fluid status
Completing the exam
IV. OPTIMIZATION OF VENTRICULAR PERFORMANCE DURING NONCARDIAC SURGERY
The principles underlying optimization of ventricular performance using TEE remain guided by the Frank-Starling relationship.5,6
The value of the Frank-Starling relationship is that it provides and interactive approach to optimizing the relationship between preload and systolic output.
The necessary parameters for deriving Frank-Starling relationship, preload and SV, are easily monitored intraoperatively with TEE.
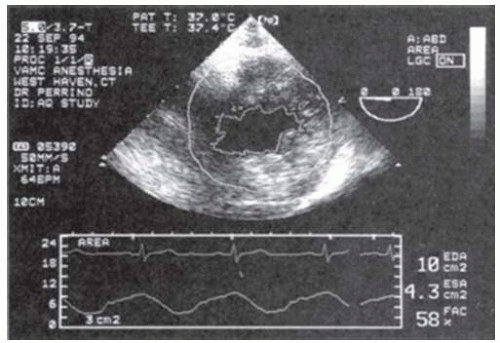
A. Assessing preload (Fig. 16-1)
TEE is superb for both quantitative assessment and monitoring the adequacy of preload throughout surgery.7,8,9,10,11
The most popular approach to measure left ventricular (LV) preload is by determination of the LVEDA from the TG midpapillary SAX view.
LVEDA has been validated to accurately track changes in intraoperative fluid status and is simply calculated from manual tracings of still frame echoes at end-diastole.
Normal values for LVEDA are typically 12 to 18 cm2.
B. Assessing stroke volume
Doppler techniques are preferred for SV determination.
SV is calculated as the time-velocity integral (TVI) multiplied by the cross-sectional area (CSA) of the conduit:
SV = TVI × CSA
Cardiac output is determined from the product of SV and heart rate.
Echocardiographic techniques for SV measurement:
SV and CO measurements are best measured at the left ventricular outflow tract (LVOT) or at the aortic valve.12,13,14
Several studies have confirmed that the CO measurement obtained by TEE compare favorably to those obtained by thermodilution.13,14
LVOT or transaortic flows are most reliably obtained from the TG LAX and the deep TG LAX views.
CSA of the LVOT is best obtained from the ME LAX view.
CSA is calculated from a measurement of the LVOT diameter as
CSAlvot = II (D/2)2
C. Generation of the Frank-Starling curve
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree