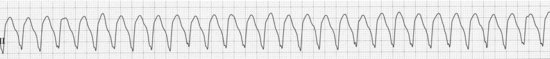
Sustained VT (call a code and worry about kaopectate later!)
DESCRIPTION
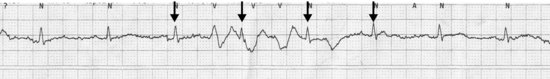
Ventricular tachycardia (VT) is a wide complex tachycardia, with the rate over 100. The beats are not preceded by P waves. If you’re lucky, or if you have very good imagination, once every 10 years or so you can actually see P waves marching through the wide complex beats. Clinicians from the Olden Days could hear a variable S1 with these dissociated P waves and did not need an ECG to decide if a patient was in ventricular tachycardia. If you can actually convince yourself P waves and QRS complexes in a short or long run of a wide complex tachycardia are dissociated, this is as close to a sure-fire proof that the rhythm is a VT as you can get. The mistake people often make is to assume that if a patient has a wide complex tachycardia over 100 and they’re awake and talking to you it can’t be VT. Wrong, dude!! It often can be hemodynamically stable, at least for a while. So don’t try to be too smart; it likely isn’t a supraventricular tachycardia with antegrade conduction over an accessory pathway: it’s usually VT.
Ventricular tachycardia can be monomorphic, where all the beats look the same, or polymorphic, where the beats keep changing shape; this can look a lot like ventricular fibrillation. If a patient has a rapid polymorphic VT and had a long QT interval before it started, you can cleverly call it torsades de pointes; see page 38.
Ventricular tachycardia is either non-sustained (it stops by itself) or sustained (get the paddles!!).
HABITAT
This can be found anywhere a patient is on telemetry, but is usually found in cardiac units after heart attacks or in patients who have two remaining functioning myocytes and an ejection fraction of 5%. Seriously, the worse the heart function the more likely you are to find VT. With an impaired ejection fraction (< 30–35%) or in the setting of acute ischemia, VT is a savage beast requiring care, respect, and appropriate treatment. However, if you encounter a few beats of VT in someone with normal heart function who is not ischemic (and if their potassium is OK and if they’re not receiving drugs that can provoke VT) it’s a pussy cat that you can usually just watch (note we did NOT say “ignore”!!). If you would like something to worry about, your friendly neighborhood electrophysiologist can enumerate a list of rare types of VT which may occur in patients with normal hearts.
CALL
Either “Aieee … get the paddles!!!” or, usually at 4:30 AM, “Doctor, Mr. Jones just had a four-beat run of VT, what do you want me to do?”
RESEMBLANCE TO OTHER ARRHYTHMIAS
There are lots of things that can look like VT but aren’t, sort of chameleon rhythms that are out to mimic VT and earn VT’s fear and respect.
Artifact mimicking VT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


