T-Z
Tonsillitis
Tonsillitis—inflammation of the tonsils—can be acute or chronic. The uncomplicated acute form usually lasts 2 to 5 days. The presence of proven chronic tonsillitis justifies tonsillectomy, the only effective treatment. Tonsils tend to hypertrophy during childhood and atrophy after puberty.
CAUSES AND INCIDENCE
Viral or bacterial infections and immunologic factors can lead to tonsillitis and its complications. Tonsillitis generally results from infection with beta-hemolytic streptococci but can result from other bacteria or viruses or from oral anaerobes. It commonly affects children between ages 5 and 10.
SIGNS AND SYMPTOMS
Signs and symptoms of tonsillitis include:
• mild to severe sore throat (parents of a child too young to complain of throat pain may report that the child has stopped eating)
• muscle and joint pain
• chills
• malaise
• headache
• pain that’s frequently referred to the ears
• a constant urge to swallow
• a constricted feeling in the back of the throat
• fever of 100° F (37.8° F) or higher
• swollen, tender lymph nodes in the submandibular area
• inflammation of the pharyngeal wall
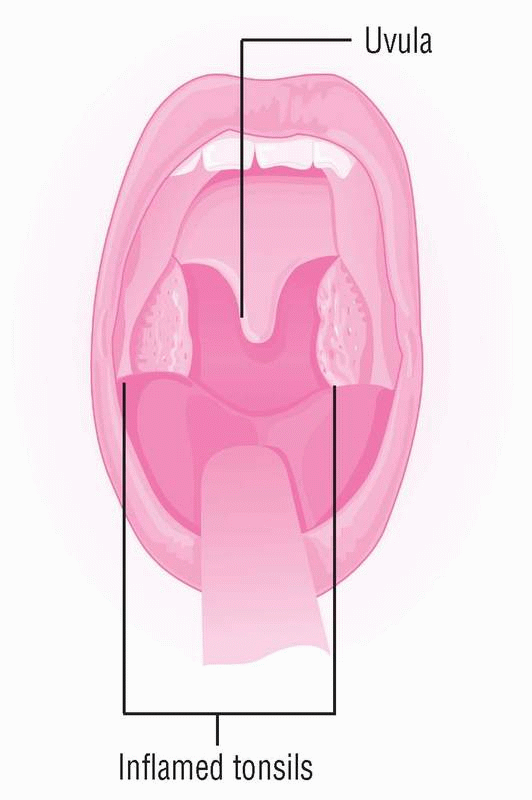
• swollen tonsils that project from between the pillars of the fauces and exude white or yellow follicles (see Looking at tonsillitis)
• purulent drainage that becomes apparent when you apply pressure to the tonsillar pillars
• edematous and inflamed uvula
• purulent drainage in the tonsillar crypts.
COMPLICATIONS
• Chronic upper airway obstruction
• Sleep apnea or sleep disturbances
• Cor pulmonale
• Failure to thrive
• Eating or swallowing disorders
• Febrile seizures
• Otitis media
• Cardiac valvular disease
• Peritonsillar abscesses
• Subacute bacterial endocarditis
• Cervical lymph node abscesses
• Streptococcal toxic shock syndrome
• Pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS)
DIAGNOSIS
• A throat culture may determine the infecting organism and indicate appropriate antibiotic therapy; the culture may also show leukocytosis.
• Differential diagnosis rules out infectious mononucleosis and diphtheria.
TREATMENT
Treatment for acute tonsillitis requires rest, adequate fluid intake, analgesics and, for bacterial infection, antibiotics. When the causative organism is group A beta-hemolytic streptococcus, penicillin is the drug of choice (another broad-spectrum antibiotic may be substituted). Most oral anaerobes also respond to penicillin. To prevent complications, antibiotic therapy should continue for 10 to 14 days.
Chronic tonsillitis (six infections per year or four infections each year for 2 years) or the development of complications (obstructions from tonsillar hypertrophy or peritonsillar abscess) may require a tonsillectomy, but only after the patient has been free from tonsillar or respiratory tract infections for 3 to 4 weeks.
Drugs
• Anti-infectives, such as erythromycin, clarithromycin (Biaxin), azithromycin (Zithromax), and clindamycin (Cleocin), to combat infection
• Analgesics for pain
SPECIAL CONSIDERATIONS
• Despite dysphagia, urge the patient to drink plenty of fluids, especially if he has a fever. Offer a child flavored drinks and ices. Suggest gargling with warm salt water to soothe the throat, unless it exacerbates pain. Make sure the patient and his parents understand the importance of completing the prescribed course of antibiotic therapy.
• Before tonsillectomy, explain to the adult patient that a local anesthetic prevents pain but allows a sensation of pressure during surgery. Warn the patient to expect considerable throat discomfort and some bleeding postoperatively. Watch for continuous swallowing, a sign of heavy bleeding.
• For the pediatric patient, keep your explanation simple and nonthreatening. Show him the operating and recovery areas, and briefly explain the facility routine. Most facilities allow one parent to stay with the child.
• Postoperatively, maintain a patent airway. To prevent aspiration, place the patient on his side. Monitor vital signs frequently, and check for bleeding. Immediately report excessive bleeding, increased pulse rate, or dropping blood pressure. After the patient is fully alert and the gag reflex has returned, allow him to drink water. Later, urge him to drink plenty of nonirritating fluids, to ambulate, and to take frequent deep breaths to prevent pulmonary complications. Give pain medication as needed.
• Before discharge, provide the patient or his parents with written instructions on home care. Tell them to expect a white scab to form in the throat between 5 and 10 days postoperatively, and to report bleeding, ear discomfort, or a fever that lasts longer than 3 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree