Systolic Murmurs
1. How is the sound of a systolic murmur produced?
2. List the murmurs associated with right ventricular outflow obstruction.
3. List the murmurs associated with left ventricular outflow obstruction.
4. How is the sound of a systolic regurgitation murmur produced?
5. List the systolic regurgitation murmurs.
ANATOMY AND PHYSIOLOGY
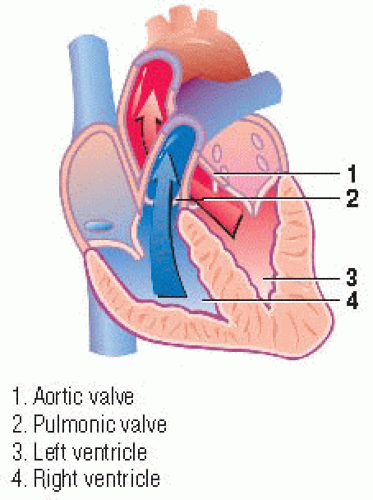
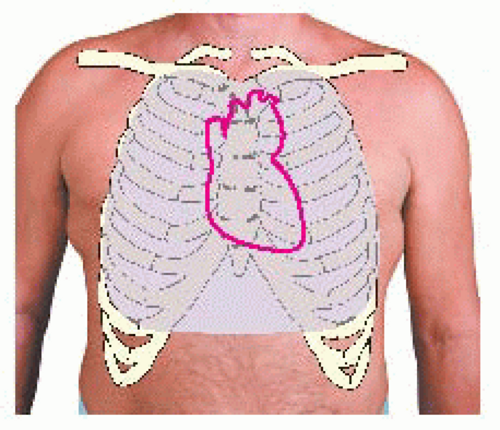
Normally, as ventricular pressures rise at the beginning of systole, the mitral and tricuspid valves close. For a brief time, while the aortic and pulmonic valves are still closed during isovolumic contraction, ventricular pressures rise sharply. When the pressure in both ventricles is high enough, the aortic and pulmonic valves open, and blood is ejected from the ventricles into the aorta and the pulmonary artery. Normally functioning valves facilitate this unidirectional blood flow.
However, aortic or pulmonic outlet abnormalities may generate forward systolic ejection murmurs. When the mitral or tricuspid valve is involved, backward, or regurgitant, murmurs may be heard during systole. All systolic murmurs occur during ventricular systole between the first and second heart sounds (S1 and S2).
Between ages 30 and 80, the left ventricular wall grows 25% thicker from its increased efforts to pump blood. Heart valves also become thicker from fibrotic and sclerotic changes. This thickening can prevent the valves from closing completely, causing systolic murmurs.
SYSTOLIC EJECTION MURMURS
During ventricular systole, the rapid ejection of blood from the ventricles causes turbulent blood flow, which produces an innocent systolic ejection murmur (SEM). (♦Sound 27) This murmur, which is considered to be normal, is usually inaudible. However, in thin-chested individuals, children, and patients with hyperdynamic states, such as anemia, thyrotoxicosis, fever, pregnancy, or arteriovenous shunts, an SEM can usually be auscultated.
An SEM, classified as benign or functional, is called an innocent or flow murmur because there’s no associated physiologic or structural abnormality. However, unusual turbulence related to dilation of the aorta or pulmonary artery may also produce an innocent SEM. Researchers believe SEMs can be caused by sclerotic changes in the aortic valve cusps.
About 50% of all persons older than age 50 have this type of murmur, which is heard more commonly in women and in patients with hypertension.
Sound characteristics
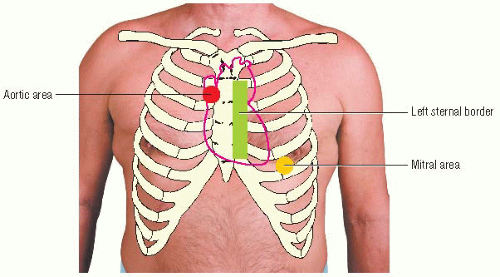
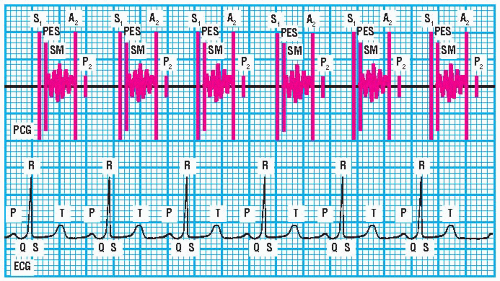
An SEM is usually heard best along the left sternal border and sometimes over the aortic and mitral areas. Its intensity is usually soft (less than a grade 3/6), and the duration of the murmur is short.
 AUSCULTATION TIP
AUSCULTATION TIPTo determine if α murmur intensifies, listen at the murmur’s border.
An SEM has a medium pitch that’s heard best using the diaphragm of the stethoscope. The quality of an SEM varies. Its timing is early systolic; it ends well before a normal S2 split. It’s heard after the QRS complex on the electrocardiogram (ECG) waveform. An SEM has a crescendo-decrescendo configuration. (♦Sound 27)
Enhancement techniques
An SEM’s intensity can be increased by maneuvers that increase blood volume or ejection velocity, such as having the patient raise his legs from a recumbent position, exercise briefly, or cough a few times.
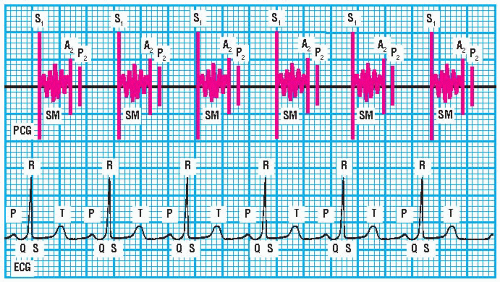 PCG and ECG showing systolic ejection murmur |
VENTRICULAR OUTFLOW OBSTRUCTION MURMURS
Right or left ventricular outflow obstructions may be supravalvular, valvular, or subvalvular. Regardless of location, the outflow obstruction causes turbulent blood flow, which produces a midsystolic ejection murmur. The murmur begins early in systole—after S1 and the opening of the diseased pulmonic or aortic valve. It ends before the S2 closure component of the diseased pulmonic or aortic valve. This murmur typically has a crescendo-decrescendo configuration that peaks in intensity in early systole, midsystole, or late systole, depending on the severity of the obstruction.
Right ventricular outflow obstruction murmurs
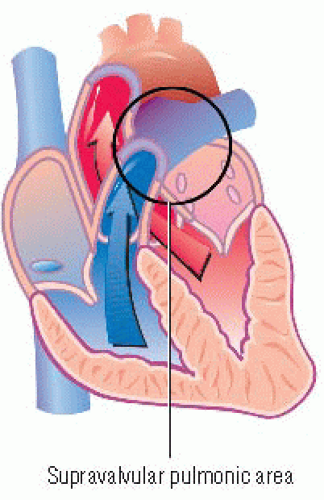
Supravalvular pulmonic stenosis murmurs
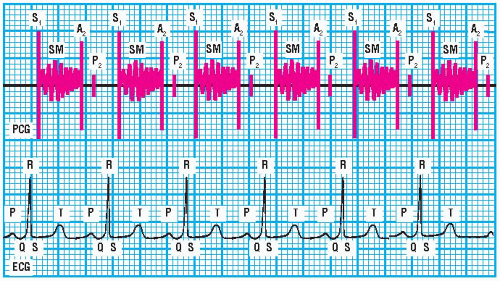
Supravalvular pulmonic stenosis, or pulmonary artery branch stenosis, is a type of right ventricular outflow obstruction that occurs above the pulmonic valve. This obstruction produces a murmur with a crescendo-decrescendo configuration that’s occasionally continuous. (♦Sound 28) The murmur is rarely accompanied by a pulmonic ejection sound (PES) and is associated with a P2 of normal intensity.
 PCG and ECG showing supravalvular pulmonic stenosis murmur |
Sound characteristics
A supravalvular pulmonic stenosis murmur is usually heard over much of the thorax. Its intensity and duration vary. It has a medium pitch that’s heard best using the diaphragm of the stethoscope, and it has a harsh quality. Its timing is systolic: it begins after S1 and ends before a normal S2 split. On the ECG waveform, the murmur begins just after the QRS complex begins and ends just before the T wave ends. It has a crescendo-decrescendo configuration that’s occasionally continuous. (♦Sound 28)
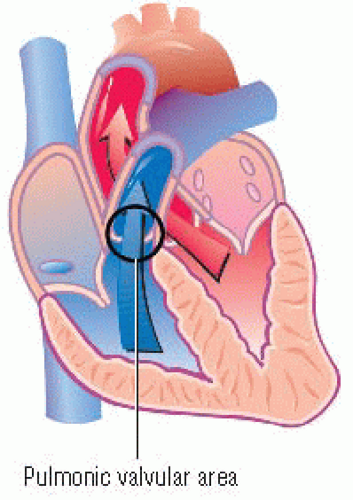
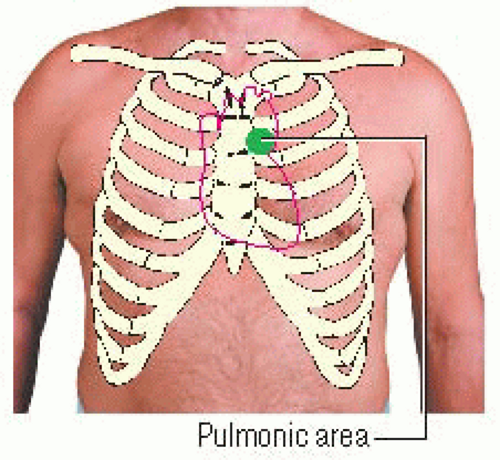
Pulmonic valvular stenosis murmurs
A pulmonic valvular stenosis murmur results from congenital pulmonic valvular stenosis and is commonly associated with other congenital defects. In mild pulmonic valvular stenosis, S1 is normal. The murmur begins after S1 with a right-sided PES as the pulmonic valve abruptly stops opening. Remember, the PES is the only right-sided heart sound that increases in intensity during expiration and becomes less audible during inspiration. The murmur intensifies after the PES and peaks in midsystole; then it begins to fade. It ends before S2. The intensity of P2 is normal. (♦Sound 29)
With severe pulmonic valvular stenosis, the pressure gradient across the pulmonic valve increases. An increased pressure gradient causes the PES to be heard earlier; it may even fuse with S1.
The right ventricular ejection time is also prolonged. Consequently, the murmur has a longer crescendo and the intensity peaks later in systole. It continues throughout A2 but ends before P2. Prolonged right ventricular ejection time also causes a delayed P2, creating a wide S2 split.
The right ventricular ejection time is also prolonged. Consequently, the murmur has a longer crescendo and the intensity peaks later in systole. It continues throughout A2 but ends before P2. Prolonged right ventricular ejection time also causes a delayed P2, creating a wide S2 split.
 PCG and ECG showing pulmonic valvular stenosis murmur |
Usually, as the stenosis becomes more severe, the murmur’s duration lengthens and its configuration becomes more asymmetrical. Consequently, P2 is delayed even more and its intensity is decreased.
Sound characteristics
A pulmonic valvular stenosis murmur is heard best near the heart’s base over the pulmonic area. It commonly radiates toward the left side of the neck or the left shoulder. The murmur’s intensity is usually soft, but it will become louder with a palpable thrill toward the left side of the neck and the left shoulder as the stenosis becomes more severe. Its duration is short, but this too will increase as the stenosis worsens. It has a medium pitch that’s heard best using the diaphragm of the stethoscope and a harsh quality. Its timing is midsystolic: it ends before a normal S2 split. It’s accompanied by a PES that diminishes or disappears with inspiration. On the ECG waveform, it begins after the QRS complex and ends before the T wave ends. The murmur has a crescendo-decrescendo configuration. A mild pulmonic valvular stenosis murmur is shaped like a diamond; a severe pulmonic valvular stenosis murmur, like a kite. (♦Sound 29)
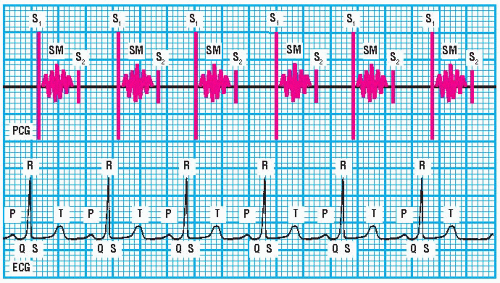
 PCG and ECG showing subvalvular pulmonic stenosis murmur |
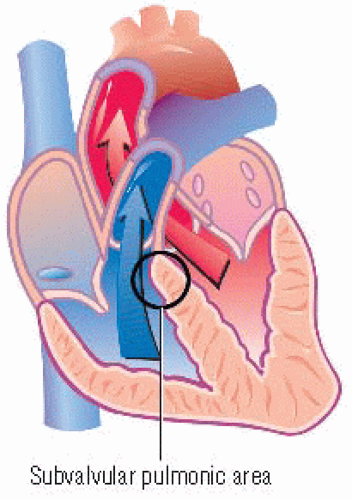
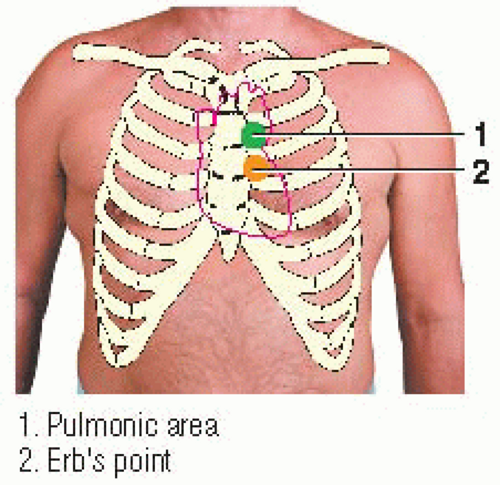
Subvalvular pulmonic stenosis murmurs
When a right ventricular outflow obstruction is beneath the pulmonic valve, or subvalvular, the midsystolic ejection murmur sounds the same as a pulmonic valvular stenosis murmur. However, it isn’t initiated by a PES. (♦Sound 30) If the subvalvular obstruction is associated with a ventricular septal defect, the murmur will be more complex in character.
Sound characteristics
A subvalvular pulmonic stenosis murmur is usually heard best over the pulmonic area and over Erb’s point; it commonly radiates toward the left side of the neck, the left shoulder, or both. Its intensity is usually soft but becomes louder as the stenosis worsens. The duration, which is short, also increases as the stenosis worsens. The murmur has a medium pitch that’s heard best using the diaphragm of the stethoscope; its quality is harsh. Its timing is midsystolic: it starts after S1 and ends before a normal S2 split. On an ECG, the murmur begins after the QRS complex and ends before the T wave ends. (♦Sound 30) This murmur isn’t initiated by a PES. It has a crescendo-decrescendo configuration.
Left ventricular outflow obstruction murmurs
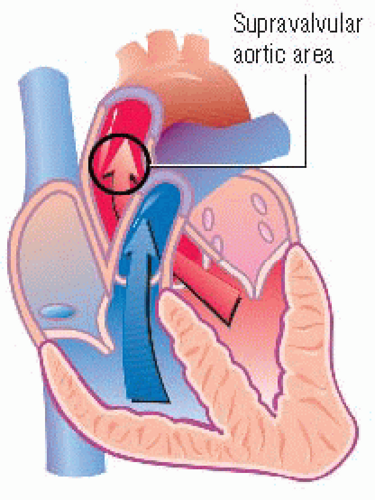
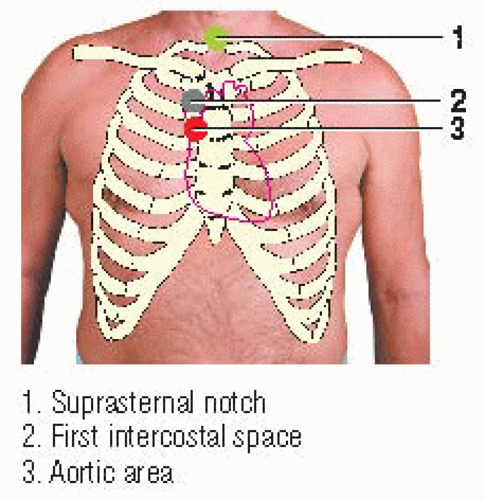
Supravalvular aortic stenosis murmurs
When a left ventricular outflow obstruction is above the aortic valve, or supravalvular, it produces a murmur with
a crescendo-decrescendo configuration. Supravalvular aortic stenosis is usually congenital. Its characteristics are similar to those of aortic valvular stenosis, except that it has no aortic ejection sound (AES), is louder, and is heard best over the suprasternal area, aortic area, or right first intercostal space. (♦Sound 31)
a crescendo-decrescendo configuration. Supravalvular aortic stenosis is usually congenital. Its characteristics are similar to those of aortic valvular stenosis, except that it has no aortic ejection sound (AES), is louder, and is heard best over the suprasternal area, aortic area, or right first intercostal space. (♦Sound 31)
 PCG and ECG showing supravalvular aortic stenosis murmur |
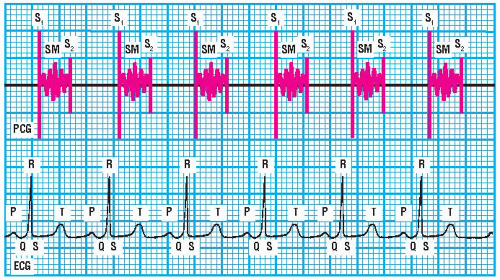
Sound characteristics
A supravalvular aortic stenosis murmur is usually heard best near the heart’s base over the right first intercostal space, over the aortic area, and over the suprasternal notch. It may radiate toward the right side of the neck, the right shoulder, or both. Its intensity, typically a grade 3/6 to 4/6, decreases in patients with left-sided heart failure. Its duration increases as the stenosis worsens. It has a medium pitch that can be heard equally well with the diaphragm or bell of the stethoscope. The murmur has a rough quality. Its timing is midsystolic: it ends before a normal S2 split. It isn’t associated with an AES. On the ECG waveform, it begins after the QRS complex and ends before the T wave ends. The murmur has a crescendo-decrescendo configuration. (♦Sound 31)
Aortic valvular stenosis murmurs
Aortic valvular stenosis may be congenital or may be acquired from degenerative or rheumatic heart disease. If it’s acquired from rheumatic heart disease, the mitral valve is commonly affected as well. Aortic stenosis produces an SEM that begins after S1 and ends before S2. (♦Sound 32) After S1, the left ventricular pressure rises. The stenotic aortic valve halts its opening motion and produces a loud AES that’s heard best near the heart’s apex over the mitral area. The AES is followed by the murmur, which gradually intensifies until midsystole to late systole and then fades, ending before a faint A2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree