Synovial Sarcoma
Borislav A. Alexiev, M.D.
Jennifer M. Boland, M.D.
Allen P. Burke, M.D.
Terminology
Synovial sarcoma is a malignant mesenchymal tumor that displays a variable degree of epithelial differentiation, which may include gland formation, and has a specific chromosomal translocation t(X;18) (p11;q11). Synovial sarcomas of the thorax are rare, but most frequently occur in the mediastinum, followed by the pleura, lung parenchyma, pericardium, and myocardium. Synovial sarcomas of the pleura are discussed in Chapter 96, Part 1.
Incidence and Clinical
Synovial sarcoma accounts for up to 8% to 10% of all histologic types of soft tissue sarcoma, and can occur in almost any part of the body (i.e., it is unrelated to the synovium). It has been reported in children and adults, with a male-to-female ratio of 2:1, and most often affects the deep soft tissues of the extremities.
Primary synovial sarcoma of the mediastinum is rare, with ˜50 reported cases.1 The anterior mediastinum is the most common compartment involved, although it can also occur in the posterior mediastinum/paraspinal region and often presents with nonspecific regional symptoms including chest pain (69%), shortness of breath (63%), pericardial or pleural effusion (22%), and cough (16%).1,2
Gross Pathology
Synovial sarcoma is usually grossly circumscribed, although this may be deceptive as it may microscopically invade adjacent mediastinal structures. The cut surface is soft or firm, pink-tan to yellow-grey, and can be multinodular and cystic. Hemorrhage, necrosis, and calcifications may be present.
Microscopic Pathology
Histologically, synovial sarcoma may be monophasic fibrous (spindle cells only), biphasic (spindle cells and gland formation), or poorly differentiated, which have been divided into small, large and spindle cell variants, the latter with abundant necrosis and prominent hemangiopericytoma-like vascular pattern.3
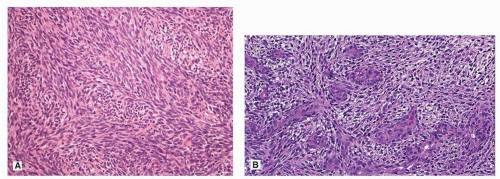
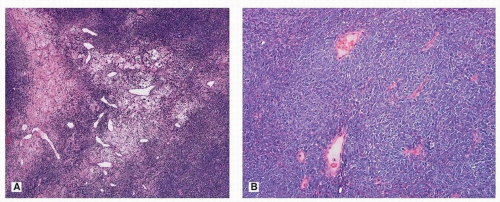
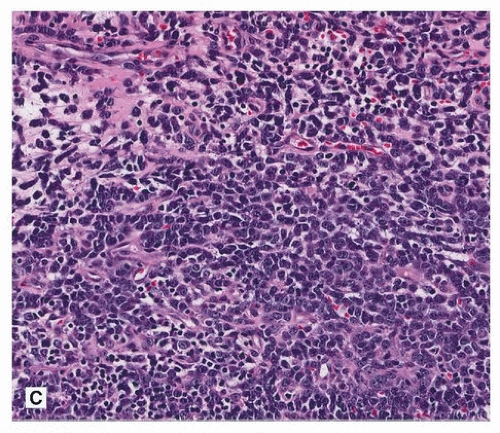
It seems that monophasic examples outnumber biphasic tumors in the mediastinal location. The monophasic subtype is composed of uniform spindle cells, which are arranged in sheets, fascicles or herringbone patterns (Fig. 136.1). The tumor characteristically has a “staghorn” or “hemangiopericytoma-like” vascular pattern. The monomorphic spindle cells have sparse cytoplasm with ovoid, hyperchromatic nuclei, and inconspicuous nucleoli. The nuclear-to-cytoplasmic ratio is high, and nuclear overlapping is commonly observed. In biphasic synovial sarcoma, spindle cell and epithelial components are present in varying proportions. The spindle cells in biphasic synovial sarcoma are identical to the spindle cells in the monophasic subtype. The epithelial cells may be arranged in solid nests, cords, or glands. Some glandular lumina may contain mucin. The amount of stromal collagen is variable, but usually scant. Myxoid change, calcifications, and ossification may be present. Mast cells can be abundant. Poorly differentiated areas may be present in synovial sarcoma, usually admixed with more classic-appearing areas of monophasic or biphasic synovial sarcoma, but some examples may be entirely poorly differentiated. Poorly differentiated areas may show a small round blue cell, fascicular spindle cell, or epithelioid morphology (Fig. 136.2). Poorly differentiated areas typically have nuclear crowding, nuclear membrane irregularity, irregularly clumped chromatin,
prominent nucleoli, and high mitotic activity (>15 mitoses/10 HPFs), but usually retain some degree of nuclear monotony that is typical of translocation-associated sarcomas.
prominent nucleoli, and high mitotic activity (>15 mitoses/10 HPFs), but usually retain some degree of nuclear monotony that is typical of translocation-associated sarcomas.
Immunohistochemical Findings
Synovial sarcomas characteristically express epithelial markers (EMA and cytokeratins), usually in a focal manner. EMA is expressed more often and more widely than are cytokeratins, especially in the monophasic and poorly differentiated subtypes.2,3,4,5 It should be noted that the absence of discernable EMA and cytokeratin expression does not exclude the diagnosis of synovial sarcoma if the morphology is typical, especially on small biopsies where sampling is an issue. Because of the variability in immunohistochemical and histologic findings, molecular testing is invaluable to confirm the diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree