Unaffected long-QT syndrome family members (FMs) frequently experience syncope. The aims of this study were to test the hypothesis that syncope events in FMs are benign events and to compare clinical characteristics, triggers eliciting the syncope events, and long-term outcomes between FMs and those with LQT1 or LQT2 mutations from the international Long QT Syndrome Registry. A total of 679 FMs, 864 LQT1 patients, and 782 LQT2 patients were included. Seventy-eight FMs (11%) experienced cardiovascular events. Almost all cardiovascular events were nonfatal syncope; only 1 FM, with an additional mitral valve prolapse, experienced aborted cardiac arrest during exercise. The mean age at first syncope in FMs was 17 years, and female FMs experienced syncope more frequently than male FMs (14% vs 9%, p = 0.027). Syncope was more frequently triggered by exercise in LQT1 patients (43% in LQT1 patients vs 5% in FMs, p <0.001), while syncope triggered by a variety of other triggers was more frequent in FMs (54% in FMs vs 22% in LQT1 patients and 30% in LQT2 patients, p <0.001 for both). None of the FMs experienced aborted cardiac arrest or sudden cardiac death after the first syncopal episode. In conclusion, syncope is frequently present in FMs, and these syncopal events occurred more frequently in female than in male FMs, with an increased incidence in midadolescence. Triggers eliciting the syncopal events were different between FMs and patients with long-QT syndrome mutations. Hence, the type of trigger is useful in distinguishing between high- and low-risk syncope. These data indicate that FMs from families with LQTS have a benign form of syncope, most likely related to vasovagal syncope and not ventricular tachyarrhythmic syncope.
Highlights
- •
Syncope occurred in 11% of family members of patients with LQTS.
- •
These syncope events occurred mainly in female family members during midadolescence.
- •
None of the family members had life-threatening events after the syncope episodes.
- •
These data suggest that family members most likely have benign vasovagal syncope.
Long-QT syndrome (LQTS) is an inherited arrhythmogenic disorder associated with an increased risk for ventricular arrhythmias leading to (arrhythmogenic) syncope and sudden cardiac death (SCD). Risk stratification studies have shown that a history of syncope is associated with a sixfold increased risk for subsequent aborted cardiac arrest (ACA) or SCD, and recurrent syncope episodes bear an even greater risk. Increased awareness of this risk has augmented the number of patients who receive implantable cardioverter-defibrillators (ICDs). In contrast, family members (FMs) who are genotype negative for a family-associated LQTS mutation also experience a 15% rate of nonfatal syncope events but a near zero rate of life-threatening events. These FMs with syncope might also be treated with ICDs on the basis of the presence of clinical symptoms in combination with their suspected familial sensitivity for SCD. However, in the general population, vasovagal syncope is extremely common, with a lifetime cumulative incidence of ≥1 syncopal episode in teenagers up to 40% by the age of 21 years. Given the substantial complication rate of ICD implantations, adequate risk stratification is mandatory to distinguish whether a syncopal event was caused by a potentially lethal arrhythmia or whether the faint was a vasovagal episode occurring in an LQTS FM. We hypothesized that syncope events in FM are simple vasovagal syncope events, and we aimed to support this hypothesis by analyzing the characteristics of the syncope events.
Methods
The study population was drawn from subjects enrolled in the International Long QT Syndrome Registry who were genotype positive and had confirmed KCNQ1 (LQT1) or KCNH2 (LQT2) mutations. Patients were excluded if they had other LQTS-related mutations or if they had >1 mutation. First-, second-, third-, and fourth-degree genotype-negative FMs were (1) genotype-negative for a mutation in 1 of the LQTS-associated genes and (2) had corrected QT intervals ≤450 ms by Bazett’s formula. In particular, FMs of patients who had tested positive for LQTS-related mutations were excluded if they had not been tested for any gene or the test result was unknown. All subjects or their guardians provided informed consent for the genetic and clinical studies.
Information on personal history, including cardiovascular events, defined as syncope (transient loss of consciousness due to cerebral hypoperfusion with abrupt onset and offset) or ACA (requiring external defibrillation as part of the resuscitation or appropriate shock therapy in patients with ICDs) or LQTS-related SCD (abrupt in onset without evident cause, if witnessed, or death that was not explained by any other cause if it occurred in a nonwitnessed setting such as sleep), electrocardiography, and therapy was acquired at the time of enrollment. Clinical data were collected yearly on prospectively designed forms with information on medical therapy and the occurrence of LQTS-related cardiovascular events during long-term follow-up. Data regarding triggers for syncope were collected for each patient and FM as reported by the patient, if alive, by FMs, or by the primary care physician after the occurrence of an event. Additional information about the syncopal event was collected using a specific questionnaire and further corroborated by the study coordinators through the patients’ medical files and oral histories. Subsequently, the study specialists categorized each reported syncopal trigger into (1) exercise triggers, (2) arousal triggers, (3) syncope occurring during sleep or rest, and (4) other triggers.
Clinical characteristics of the genotype-negative FMs and LQT1 and LQT2 patients were compared using chi-square or Fisher’s exact tests for categorical variables and Wilcoxon’s 2-sample test for continuous variables. The characteristics of the genotype-negative FMs were further compared by the occurrence of trigger-specific syncope using chi-square or Fisher’s exact tests for categorical variables and Kruskal-Wallis tests for continuous variables. To assess the time to a first trigger-specific event by genotype (patients vs FMs) in LQT1 and LQT2, and to assess the independent contribution of gender to the first occurrence of other-trigger syncope events during follow-up, the Kaplan-Meier method was used, and significance was tested by using the log-rank test. Follow-up was censored at 40 years of age to avoid confounding by acquired cardiovascular disease. Multivariate Cox proportional-hazards regression models were used to evaluate the occurrence of trigger-specific syncopal events by genotype. Prespecified covariates in the total population model included gender, age, corrected QT duration (≥500 ms), and medical therapy with β blockers. Beta-blocker therapy was assessed as a time-dependent covariate in the multivariate model.
Results
The study population consisted of 695 genotype-negative FMs, 864 LQT1 patients, and 782 LQT2 patients. Demographic and clinical characteristics of all study subjects are listed in Table 1 . In general, LQT1 and LQT2 patients were more likely to be female and, as expected, were more frequently receiving therapy compared with FM. This notwithstanding, 51 FMs were also receiving therapy (β blockers n = 51, pacemakers n = 2, ICDs n = 3).
| Variable | Family Members (N = 695) | LQT1 Patients (N = 864) | p-Value ∗ | LQT2 Patients (N = 782) | p-Value † |
|---|---|---|---|---|---|
| Female | 319 (46%) | 488 (56%) | <0.001 | 422 (54%) | 0.002 |
| QTc (ms) | 393 ± 16 | 480 ± 47 | NA | 481 ± 54 | NA |
| Therapy | |||||
| Beta-blockers | 51 (7%) | 400 (46%) | <0.001 | 436 (56%) | <0.001 |
| Left cardiac sympathetic denervation | 0 (0%) | 7 (1%) | 0.019 | 12 (2) | 0.001 |
| Pacemaker | 2 (0%) | 18 (2%) | 0.001 | 62 (8) | <0.001 |
| Implantable cardioverter-defibrillator | 3 (0%) | 74 (9%) | <0.001 | 120 (15%) | <0.001 |
| Cardiovascular events | 78 (11%) | 302 (35%) | NA | 297 (38%) | NA |
| Syncope | 77 (11%) | 292 (34%) | 278 (36%) | ||
| Aborted cardiac arrest | 1 (0%) | 24 (3%) | 37 (5%) | ||
| Sudden cardiac death | 0 (0%) | 17 (2%) | 27 (4%) | ||
| Age at first syncope, mean (years) | 17.2 ± 9.7 | 13.1 ± 8.4 | 0.001 | 16.4 ± 8.6 | 0.58 |
| Recurrent syncope | 39 (6%) | 179 (21%) | <0.001 | 183 (23%) | <0.001 |
| Total syncopal episodes | 176 | 1022 | 932 | ||
| Number of syncope, median | 2 (1–3) | 2 (1–3.5) | 0.064 | 2.5 (1–4) | 0.002 |
∗ p-value calculated of LQT1 patients vs. family members.
A total of 78 FMs (11%) experienced cardiovascular events. Almost all cardiovascular events in FMs were nonfatal syncope (n = 77; Figure 1 ); only 1 FM experienced an ACA ( Figure 1 ). This genotype-negative female FM with a familial LQT2 mutation experienced an ACA while playing volleyball at 14 years of age. She had a baseline corrected QT interval of 400 ms and had an additional mitral valve prolapse. In contrast, 302 LQT1 patients (35%) and 297 LQT2 patients (38%) experienced the primary end point of a first cardiovascular event ( Table 1 ). ACA or SCD occurred in 41 LQT1 patients (4.7%) and 64 LQT2 patients (8.2%), and syncope was reported in 292 LQT1 patients (34%) and 278 LQT2 patients (36%).
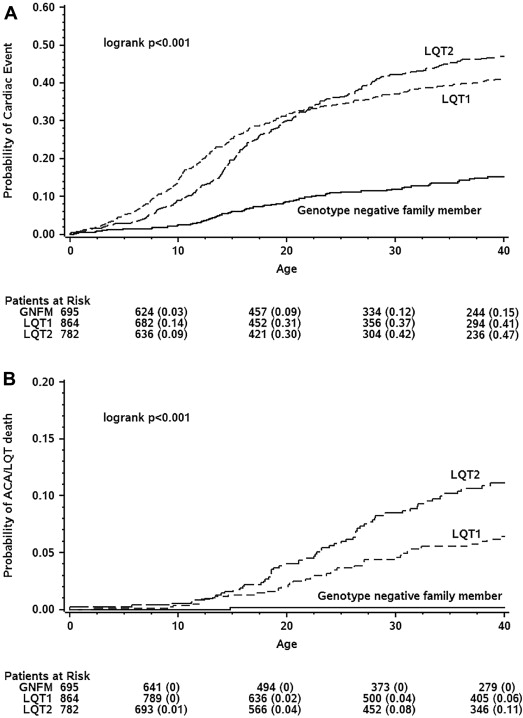
LQT1 patients were significantly younger than FMs when they experienced their first syncope events (13 vs 17 years, p <0.01). Female FMs experienced more syncopal events than men (14% vs 9%, p = 0.027). Additionally, in female FMs, there was a distinct peak of first syncope events around 15 years. Only 1 FM was receiving a β blocker during a syncope event. Half of the FMs with syncope (n = 39 [51%]) experienced ≥1 recurrent syncopal episode. Female FMs experienced a median of 1.5 (interquartile range 1 to 3), while the median number in male FMs was 2 (interquartile range 1 to 3). None of the FMs experienced ACA or SCD after the initial syncopal episode, while 28 LQT1 patients (10%) and 44 LQT2 patients (16%) did.
The first syncopal event in FMs was triggered by exercise in 4 (5.2%), by arousal in 14 (18%), during sleep in 1 (1.3%), and by other triggers in 41 (53%) ( Table 2 ). There was no difference in gender, age at first event, or degree of FM among the different types of triggers ( Appendix A ). In total, cardiovascular events (at any time) were triggered by exercise in 11 FMs (2%), by arousal in 19 FMs (3%), and by other triggers in 53 FMs (8%). Of 11 total exercise-triggered events, 4 (36%) occurred in FMs of LQT1 patients and 7 (64%) occurred in FMs of LQT2 patients (p = 0.54). Of a total of 19 arousal-triggered events 8 (42%) occurred in LQT1 FMs and 11 (58%) in LQT2 FMs (p = 0.77). There was a significant difference in distribution of the triggers in FMs compared with LQTS patients (LQT1 patients vs FMs p <0.01, LQT2 patients vs FMs p <0.01; Figure 2 ). Syncope was significantly more frequently triggered by exercise in LQT1 patients and by arousal in LQT2 patients compared with FM ( Table 2 ; extended specification in Appendix B ). This was confirmed in multivariate analysis after adjustment for relevant covariates including gender and time-dependent β-blocker use, with a hazard ratio for exercise-triggered cardiovascular events of 12.5 (p <0.01) in LQT1 patients and for arousal-triggered events of 3.4 (p <0.01) in LQT2 patients. Syncope preceded by another known trigger (other triggered) was more frequent in FMs than in LQT1 and LQT2 patients (53% in FMs vs 22% in LQT1 patients and 30% in LQT2 patients, p <0.01 for both). This group constituted a variety of triggers ( Appendix B ). Syncopal events triggered by extreme heat or dehydration or menses were more frequent in FMs. Kaplan-Meier analysis demonstrated a slight trend toward more other-triggered syncopal events in female than in male FMs (12% vs 9%, log-rank p = 0.16; Figure 3 ). Additionally, similar to the syncope events of any trigger, there was a notable steep increase in incidence of other-triggered syncopal events in female FMs from the age of 12 years.
| Variable | Family Members (N = 77) | LQT1 Patients (N = 292) | p-Value ∗ | LQT2 Patients (N = 278) | p-Value † |
|---|---|---|---|---|---|
| Exercise | 4 (5%) | 126 (43%) | <0.001 | 19 (7%) | 0.61 |
| Swimming | 1 (1.3%) | 46 (16%) | 0 (0%) | ||
| Arousal | 14 (18%) | 35 (12%) | 0.15 | 57 (21%) | 0.65 |
| Loud noise | 0 (0%) | 2 (0.7%) | 34 (11%) | ||
| Rest or sleep | 1 (1.3%) | 1 (0%) | 0.31 | 23 (8%) | 0.03 |
| Other | 41 (53%) | 64 (24%) | <0.001 | 86 (31%) | <0.001 |
| Fever/illness, | 6 (7.7%) | 10 (3%) | 13 (4.7%) | ||
| Substance abuse | 2 (2.6%) | 2 (0.7%) | 0 (0%) | ||
| Menses | 3 (3.8%) | 2 (0.7%) | 2 (0.7%) | ||
| Extreme heat/dehydration | 6 (7.5%) | 2 (0.7%) | 8 (2.9%) | ||
| Unknown or missing information on trigger type | 17 (22%) | 66 (23%) | 0.92 | 93 (33%) | 0.056 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


