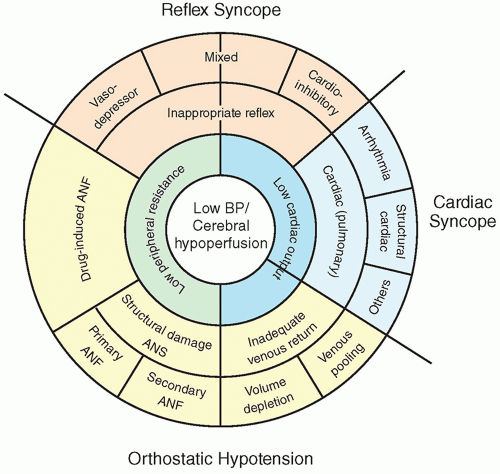
Cardiac or
cardiopulmonary syncopes, which occur when the cardiac output is dramatically decreased, can be subdivided into two categories:
arrhythmic syncope and
structural cardiac disease. The most frequent form of arrhythmic syncope is that caused by bradyarrhythmias, usually happening when the ventricular rate is lower than 30 bpm for 15 to 30 seconds.
9 Tachyarrhythmias, notably ventricular tachycardia but also supraventricular tachycardia, can also present with syncope. Particular heart diseases that lead to syncope are covered in depth in specific chapters in this book.
Some conditions may be confused with syncope.
Generalized epileptic seizures, with concomitant disorganized electrical activity of both cerebral hemispheres, cause
TLOC, but generally last longer and present with one-sided limb movements, tongue bites, and more prolonged postictal mental confusion and somnolence.
Psychogenic pseudosyncope does not have the characteristic changes in BP and heart rate that accompany syncope; it usually has increased frequency, longer duration, and patients tend to maintain their eyes closed, which is unusual in syncope.
Cerebrovascular disease, notably
subclavian steal syndrome, which was previously described as a cause of syncope, does not fit the more modern definition. This syndrome, as well as transient ischemic attacks (TIAs) arising from carotid obstructions or vertebrobasilar ischemia, does not present without focal neurologic signs, being relatively easy to distinguish from syncope in general practice.
Cataplexy, a rare diagnosis, can be distinguished because of the fact that patients with this condition do not have amnesia, being able to describe the event after recovering conscience.