Syncope
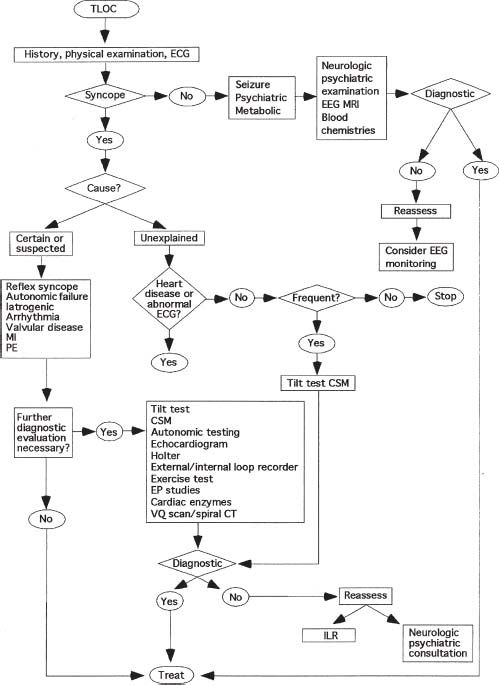
This chapter focuses on core material related to the evaluation of patients who present with syncope of unknown origin. It reviews the indications and contraindications for various salient procedures and diagnostic maneuvers to evaluate patients who present with syncope. Highlighted among these are head-up tilt table testing to provoke and confirm neurocardiogenic syncope and electro-physiologic testing to assess for atrioventricular (AV) node and sinoatrial (SA) node dysfunction and inducibility of supraventricular tachycardia (SVT) and ventricular tachycardia (VT), which could be responsible for recurrent syncope. It is critical, in this era of evidence-based medicine and quality outcomes, health maintenance organizations (HMOs), diagnosis-related groups (DRGs), and limitations of diagnostic testing availability, that a concise, logical, streamlined approach to the evaluation of patients with syncope be employed. Several useful algorithms can be found in the literature (Fig. 32.1).1 Recently, it was proposed that emergency departments adopt a streamlined approach to syncope patients that will allow more efficient utilization of resources, identifying high-risk patients and avoiding unnecessary admissions for low-risk patients.2
FIGURE 32.1 Example of diagnostic algorithm for patients with LOC. TLOC, transient loss of consciousness; ECG, electrocardiogram; EEG, electroencephalogram; MRI, magnetic resonance imaging; MI, myocardial infarction; PE, pulmonary embolism; CSM, carotid sinus massage; EP studies, electrophysiologic studies; VQ scan, ventilation perfusion scan; CT, computed tomography; ILR, insertable loop recorder. (Reprinted from Kaufmann H, Wieling W. Syncope: a clinically guided diagnostic algorithm. Clin Auton Res. 2004(Suppl 1);14:i87–i90, with permission.)
Syncope, defined as the transient loss of consciousness (LOC) with complete reversibility without subsequent focal neurologic deficit, is a frequent clinical conundrum for cardiologists, internists, and electrophysiologists.3,4 The approach to the syncopal patient is comprised of several algorithms, the aggressiveness of which depends on the seriousness of the syncopal spells, and the presence or absence of structural heart disease. Although the most common etiology of all syncope from all causes and in all groups is probably benign vasovagal syncope, a syncopal event in a patient with significant coronary disease, prior myocardial infarction (MI), severe left ventricular (LV) dysfunction, congestive heart failure, or in the context of known complex ventricular arrhythmias may be malignant and a harbinger of subsequent sudden cardiac death.
EPIDEMIOLOGY OF SYNCOPE
In the early 1980s, it was recognized that syncope is a common reason for emergency room visits and admissions.5 Many of these patients were suspected to have either reflex or neurocardiogenic/vasovagal syncope, but testing was limited. Simultaneously, techniques of electrophysiologic testing were being developed, ambulatory monitoring was in its infancy, and tilt table tests were still a research tool. Then, as today, the workup for patients with unexplained syncope was extremely expensive. Even with recent constraints, DRGs, and so on, the evaluation of patients with syncope still has been estimated to be $1 billion annually. Although syncope for the most part was probably suspected to be due to underlying neurocardiogenic syncope, in the 1980s, there was no good test or “gold standard” to determine which patients were susceptible or truly vasovagal. When the tilt table was introduced and recognized as a valuable electrophysiologic modality, it entered intense and extensive utilization. The late 1980s and early 1990s represent the probable zenith of its use. Between 1992 and 1994, tilt table procedures escalated from approximately 6,000 to 14,000 per year. Recent years have seen a downtrend in the number of tilt table tests being performed, particularly as our clinical acumen has become better at identifying patients who are experiencing vasovagal syncope. Patients with syncope and a normal heart virtually always have underlying vasovagal syncope, even despite a negative tilt table test. Given the constraints of limited reproducibility, specificity, and sensitivity, tilt table tests, although still frequently performed, are reserved for those patients who meet specific criteria of recurrent syncope, for which no ready explanation can be provided. Although tilt table numbers have declined for suspected vasovagal syncope, the last few years have seen a burgeoning of requests to investigate for underlying dysautonomias such as postural orthostatic tachycardia syndrome (POTS).
In general, determination of the underlying etiology for syncope is almost always largely presumptive. Rarely do spontaneous clinical events occur during cardiac or telemetric monitoring. The goal in the evaluation of syncope is therefore not only to determine a likely underlying diagnosis with a relative degree of certainty and alacrity but also to ensure that no life-threatening entities are responsible. Diagnostic studies such as head up tilt table tests and electrophysiologic studies (EPS) are merely tools to examine various components of the autonomic nervous system and the cardiac electrical system, and the results must be interpreted with cautious skepticism. Although it is reassuring to convince oneself of a relatively benign type of syncope, as in vasovagal, it is axiomatic that the patient should always be assumed to have more malignant underlying causes of syncope until proven otherwise. Merely assuming that a positive tilt table test explains syncope in a patient with an ejection fraction (EF) of 25% from known coronary artery disease is clearly clinically inappropriate and fraught with danger. To further confound the differential diagnosis, many patients have syncope that is multifactorial. For example, an elderly patient with tendency toward sinus node dysfunction and carotid sinus hypersensitivity may also be on medications that result in hypovolemia and an inclination toward orthostatic hypotension (OH). All can lead to syncope.
Syncope results from the many potential causes of cerebral hypoperfusion, and textbooks and review articles frequently display long, comprehensive lists of possible etiologies of syncope (Table 32.1).6 In general, these lists can be synthesized and concentrated into five potential causes: (a) reflex syncope, of which vasovagal is the index hallmark and most common cause; (b) OH; (c) arrhythmic syncope; (d) mechanical structural disease such as coronary artery obstructive and valvular cardiac disease; and (e) cerebro-vascular causes. Using this framework and a precise definition of syncope differentiates it from other causes of LOC, including transient ischemic attacks (TIAs) and strokes, hypoglycemia and other metabolic causes, seizure disorders, psychogenic syncope, or vertebral basilar insufficiency (drop attacks). Traditionally, etiologies of syncope have also been even more broadly divided into cardiac and noncardiac causes. This simple paradigm has been utilized to predict clinical outcomes and prognosis. Cardiac causes of syncope may lead to increased mortality compared to noncardiac causes, in which the prognosis is normal and survival is assured.7 However, there is certainly considerable overlap between the cardiac and noncardiac causes. For example, it is now understood that aortic stenosis can cause syncope not only from heart block, or fixed cardiac output, but through reflex mechanisms similar to the Bezold–Jarisch reflex.8
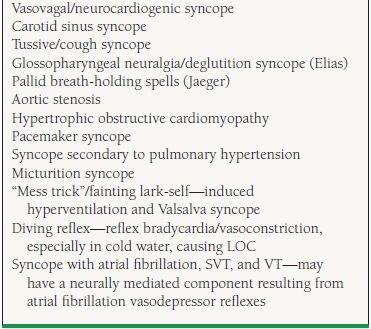
TABLE
32.1 Causes of Syncope
From Brignole M, Lavagna I, Paolo A, et al. Guidelines on management (diagnosis and treatment) of syncope—update 2004. Europace. 2004;6:467–537, by permission of Oxford University Press.
It is often difficult to differentiate an episode of true syncope from other causes of LOC. These include seizure disorders or epilepsy, metabolic abnormalities, cerebral vascular accidents (CVAs) or TIAs, and factitious syncope/pseudoseizures or conversion reactions. The prototypical tonic–clonic movements of epilepsy are well known. Aura, urinary incontinence, and tongue biting are also frequently reported during seizures. Prior head trauma and concussion also may suggest seizures as the cause of LOC. Syncope is frequently accompanied by a few involuntary movements of the head and extremities, which can mimic a seizure disorder. This has been termed “convulsive syncope” and “anoxic seizures” and results from loss of oxygen to the central nervous system (CNS) and brainstem motor centers, and does not reflect an epileptiform phenomenon. These jerking movements are also frequently observed during ventricular fibrillation induced during electrophysiologic testing or during tilt-induced profound vasovagal episodes. Witnesses to clinical episodes of syncope also frequently report similar movements and ascribe them to seizures. Even trained medical personnel may be quick to assume, incorrectly, that seizures are occurring in these situations.
HISTORY
When a patient presents with syncope of unknown origin, the single most important piece of information is the history. Specific detailed questioning regarding the presence or absence of structural heart disease, valvular heart disease, coronary artery disease, previous MIs, prior syncope,9 family history, and so on can quickly delineate the high-risk patient from those at low risk. Historical factors related to a syncopal event can also help point in a specific direction. Situational syncope during phlebotomy, during prolonged standing, in a dentist’s office, in a restaurant, in church, following alcohol ingestion, and so on is almost universally vasovagal or neurocardiogenic. The presence of prodromal symptoms, such as nausea or diaphoresis, usually also heralds the onset of the vasovagal reflex. Frequently, the patient with vasovagal syncope may have postsyncopal symptoms that can last from hours to a day or so, including weakness, nausea, fatigue, and a tendency to recurrent syncope.
In contrast, a lack of prodrome or presence of previous MI or heart failure certainly points to a more malignant etiology of syncope, usually mandating hospital admission. Complete and immediate recovery after a syncopal event suggests an arrhythmic etiology, such as VT, SVT, or AV block. Injuries are uncommon with vasovagal syncope, as the patient usually tends to crumble to the ground, rather than fall abruptly. In contrast, severe injuries and automobile accidents are suggestive of a more serious arrhythmic etiology such as extreme tachycardia or bradycardia.
Calkins et al.10 have retrospectively evaluated the value of the history and the differentiation of patients with recurring syncope. Eighty patients with recurrent syncope undergoing a complete evaluation were provided comprehensive questionnaires focusing on the features of their syncopal spells. Patients underwent extensive electrophysiologic testing, tilt table testing, and ambulatory recording when appropriate, with the diagnosis confirmed in these 80 patients. The origin of syncope was broadly broken down into two varieties: relatively benign syncope due to vasovagal or neurocardiogenic etiology versus a more serious type of syncope due to underlying AV block or VT. As expected, symptoms prior to the onset of syncope, such as blurred vision, palpitations, nausea, and generalized warmth or diaphoresis, were more consistent with neurocardiogenic syncope. Similar symptoms after the syncopal event were also more consistent with neurocardiogenic syncope. In contrast, little or no warning prior to the syncopal event was more consistent with AV block or VT. Patients with AV block or VT tended to be older and of male gender, owing to the predominance of atherosclerotic disease. In addition, patients with more dangerous syncope etiologies generally reported no prior episodes, specifically having less than two episodes of syncope in their lifetime. These features, together with a history, can help determine whether a patient requires admission for further investigation.
CLINICAL FEATURES OF SYNCOPE
Often, witnesses to the syncopal event can provide other clues as to the possible cause, particularly regarding the duration of syncope. Prolonged episodes of unresponsiveness, such as 7 to 10 minutes or more, are unlikely to be due to vasovagal or arrhythmic etiologies and instead suggest neurologic processes. Sudden LOC followed by fairly quick resumption of consciousness suggests tachyarrhythmias, such as VT, SVT, or atrial fibrillation with a post conversion pause. Patients who experience vasovagal syncope frequently have several minutes of prodromal symptoms, followed by LOC. The episode of unconsciousness with vasovagal syncope varies but may last 3 to 4 minutes, particularly if the patient cannot be rendered supine. A patient with vasovagal syncope may arouse slowly, with considerable confusion and postsyncopal vagal symptoms.
PHYSICAL EXAMINATION
The physical examination of patients with syncope is generally directed toward cardiac auscultation for the presence of valvular disease, carotid bruits, assessment of pulses, irregular pulse and heart rhythm. For patients with vasovagal syncope, the physical exam and the cardiovascular exam will generally be entirely normal. However, the presence of murmurs, S3 or S4 gallops, and displaced point of maximal intensity (PMI) may point to the presence of LV dysfunction. Similarly, bigeminal rhythms and trigeminy may also suggest the presence of LV dysfunction in a patient with syncope. Findings of congestive heart failure, jugular venous distention, hepatojugular reflux, hepatosplenomegaly, and bibasilar pulmonary rales also point to the presence of LV dysfunction in a patient with syncope. The finding of atrial fibrillation on physical examination or during electrocardiography (ECG) is very important and suggests tachybrady syndrome or sick sinus syndrome. Gross neurologic evaluation showing evidence of lateralization or focal neurologic deficits is also important, suggesting either cardioembolic phenomena from atrial fibrillation or carotid atherosclerotic disease, both of which can cause episodic LOC.
Carotid sinus massage can be performed safely at the bedside, but is contraindicated in the presence of carotid bruits, known carotid stenosis, TIAs, and CVAs. During ECG monitoring, sequential bilateral gentle carotid massage can be performed for 5 to 10 seconds, with the patient in a supine, slightly elevated head position. Positive responses consist of cardioinhibitory pauses >3 seconds. Patients with true carotid sinus syndrome frequently show an instantaneous and abrupt response with a prolonged cardioinhibitory response to massage with LOC.
Careful observations of postural responses of blood pressure and heart rate are often useful when evaluating patients with syncope. The presence of marked OH in patients with syncope is highly suggestive. OH is defined as a systolic blood pressure decline of >20 to 30 mm Hg or a diastolic blood pressure decline of >10 mm Hg. These can either be elicited immediately on assuming an upright posture from supine baseline or occur more gradually at 1 to 3 minutes. OH is very common, particularly in the elderly, and may be multifactorial, often resulting from medications (diuretics, vasodilators, etc.) and intrinsic dysfunction of autonomic reflexes that can occur with aging, strokes, diabetes, alcohol use, and atherosclerosis of cardiopulmonary, aortic arch, and carotid sinus baroreceptors. Marked abrupt or instantaneous OH is particularly prominent in multisystem atrophy (MSA, previously called Shy–Dragger syndrome) or in pure or primary autonomic failure (PAF, previously called Bradbury–Eggleston syndrome). Patients with MSA may exhibit features of Parkinson disease (PD), but PD itself is an important etiology for OH as well, either from intrinsic autonomic failure or from antiparkinson medications.11 Patients with PD often experience unexplained falls, which may result from OH, gait disturbances, or “on—off” phenomena.
DIAGNOSTIC TESTING FOR SYNCOPE
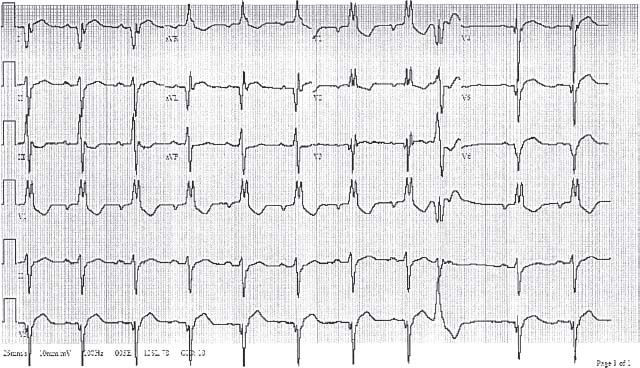
Laboratory investigation for syncope of undetermined etiology begins with an ECG to identify arrhythmias or previous MIs. The presence of Q waves indicative of previous MI, long QT interval, left bundle branch block, ventricular pre-excitation, or left anterior hemiblock are all significant and may suggest the need for further invasive investigation. Syncope in a patient with trifascicular block (Fig. 32.2) is a Class IIA indication for implantation of a permanent pacemaker.12,13 Signal-averaged ECG, although once touted as a major advancement in diagnostic capability for syncope, is now reserved largely for the detection of late potentials, predominantly in patients with transient ventricular ectopy, which may signify underlying arrhythmogenic right ventricular cardiomyopathy (ARVC). Unfortunately, most of these patients have an intrinsic QRS abnormality consistent with a right bundle branch block, which makes the signal-averaged ECG less specific.
FIGURE 32.2 Complete right bundle branch block, left anterior hemiblock, and first-degree AV block, the so-called trifascicular block. This finding in patients with syncope suggests intermittent high-degree AV block and may indicate a need for a permanent pacemaker.
Stress Testing and Echocardiography
When clinically indicated, particularly with physical findings or an ECG suggesting the presence of structural heart disease, initial testing often includes functional studies to assess for an ischemic etiology. Echocardiography is useful to assess for mechanical or structural lesions, such as hypertrophic cardiomyopathy, aortic stenosis, occult LV systolic dysfunction, or in the case of ARVC or RV dysfunction. Routine incorporation of these modalities is costly and unnecessary in the vast majority of syncope cases, particularly when the clinical history, ECG, and physical examination are normal and suggest a benign cause.
Ambulatory Electrocardiographic Monitoring
Ambulatory electrocardiographic monitoring as a baseline may be helpful, particularly for those patients with recurrent syncopal episodes, and may disclose paroxysmal atrial fibrillation, SVT, or nonsustained VT. Routine Holter monitoring in the absence of structural heart disease is frequently unrewarding. Systems utilizing event-recording technology, such as the King of Hearts (Instromedix) and others may be more helpful to disclose intermittent episodes of bradyor tachyarrhythmias. Newer wireless and bluetooth devices (e.g., Lifewatch—Instromedix, Cardionet) can provide full disclosure with continuous EKG monitoring to a central monitoring station for immediate reporting, and are collectively termed mobile cardiac outpatient telemetry (MCOT). (Fig. 32.3). These devices, however, are quite costly and are not indicated for high-risk cohorts.

FIGURE 32.3 Cardionet ambulatory arrhythmia monitor.
Ambulatory blood pressure monitor devices are also available and are frequently utilized for patients suspected of having intermittent orthostasis. However, these devices can be quite clumsy and burdensome, and often do not react quickly enough to record substantive data. Future ambulatory and implantable ECG event recorders currently in development may also allow simultaneous blood pressure recording.
Implantable Loop Recorders
The implantable loop recorder (ILR) (Fig. 32.4) (Medtronic— Reveal, St Jude Medical—Confirm) was designed specifically for patients with infrequent syncopal episodes in which Holter monitoring or 30-day event recordings fail to demonstrate the etiology of their syncope. The ideal patient is one who has recurrent syncope, palpitations, or suspected SVT once or twice a year, escaping conventional monitoring.
FIGURE 32.4 Reveal (Medtronic) ILR.
Current indications are for patients with syncope of undetermined etiology with a structurally normal heart. It should not be implanted in high-risk patients with syncope and severe LV dysfunction. It has also been used in patients with fleeting or suspected SVTs for whom electrophysiologic testing is contemplated. An emerging indication is for patients who have drug-refractory seizures in whom an arrhythmic etiology from either tachy- or bradycardia is suspected.
Several studies have utilized the ILR in their diagnostic algorithms to determine the cause of syncope. The Randomized Assessment of Syncope Trial (RAST) evaluated 60 patients randomized through either the conventional diagnostic paradigm of electrophysiologic testing, tilt table test, and extensive recording or accelerated loop recorder implants.14–16 Follow-up was for 1 year. Patients with loop recorder implants had an earlier time to diagnosis. The International Study of Syncope of Undetermined Etiology (ISSUE) investigators examined the use of the loop recorder implant in several important patient subgroups, including those with: (a) syncope and a normal heart that had a negative tilt table test; (b) syncope and a bundle branch block and a negative EPS; and (c) syncope with cardiomyopathy and a negative EPS. The first cohorts of the ISSUE study consisted of 82 patients with syncope and a negative tilt and 29 patients with syncope and a positive tilt.17 Both groups received ILRs. During follow-up, there was an approximate 34% syncope recurrence rate in both groups despite treatment. Interrogation of the ILRs showed that the underlying electrocardiographic abnormalities during syncope were consistent with a vasovagal etiology in the vast majority of patients. This suggested that in patients with a normal heart, syncope is still most likely due to underlying vasovagal phenomena, despite a negative tilt test. With this observation, as well as others on tilt test limitations, it has become apparent that the tilt table test may be superfluous in the evaluation of patients with syncope and a normal heart. The ISSUE study further went on to implant loop recorders in patients who had bundle branch block, syncope, and a negative electrophysiologic test, including a challenge with Ajmaline.18 During follow-up, syncope recurred in >40% of patients, and the most common finding was AV block or asystole, although sinus arrest was also observed. Therefore, this supported the current practice of implanting pacemakers in patients with syncope, normal LV function, and bundle branch block, which is currently a Class IIA indication. Finally, the ISSUE investigators implanted loop recorders in patients with ischemic and dilated cardiomyopathies and syncope following a negative EPS.19 These patients usually now receive a defibrillator. A total of 35 patients were implanted with loop recorders following a negative EPS. During a relatively short follow-up of 6 ± 5 months, there was a 17% recurrence of syncope, predominately due to bradyarrhythmias. No VT was observed, although the follow-up was short. Therefore, it still would be prudent to consider implanting a defibrillator in patients with severe LV dysfunction and syncope.
Recently, the ILR was utilized to disclose a new, previously poorly defined entity of prolonged paroxysmal high-degree or complete AV block in patients with recurrent syncope, otherwise normal hearts, normal EKGs without evidence of significant conduction abnormality, and no evidence that these episodes were due to a vagal etiology.20 These patients were observed to have varying degrees of transient high-degree AV block causing near syncope and were then treated with permanent pacemakers which eliminated their episodes. The actual prevalence of this disorder is unknown, but it certainly highlights the value of early utilization of ILRs in diagnostic paradigms.
No further investigations are probably required in a patient with historical absence of structural heart disease who has a normal ECG and a single episode of syncope that is typically vasovagal. However, if there are risk factors for coronary artery disease, such as a male aged >50 years, additional testing frequently includes assessment of LV function with an echocardiogram as well as an exercise test. In the absence of structural heart disease, for a single episode of syncope without malignant features, no other testing is typically required. However, if any of the above significant indicators of structural heart disease are present, then further investigation such as Holter monitoring and possibly EPS are warranted. The finding of nonsustained VT in the presence of LV dysfunction, and an EF <40%, especially in the setting of syncope, is indicative of the need for electrophysiologic testing and defibrillator implantation.
Electrophysiologic Testing
For patients who present with syncope of undetermined etiology, electrophysiologic testing has been described as the “gold standard” for demonstration of supraventricular and ventricular arrhythmias, AV nodal or His–Purkinje disease, and bradyarrhythmias, all of which can be responsible for syncope. Indications for electrophysiologic testing in patients with syncope are given in Table 32.2.21 This procedure, introduced clinically in the late 1970s, involves the insertion of several intravascular catheters to record intracardiac atrial electrograms, His potentials, and ventricular electrograms. Atrial and ventricular programmed electrical stimulation may induce sustained monomorphic VT or SVT. Measurement of AV node refractoriness and Wenckebach cycle length may demonstrate significant AV nodal disease that could be responsible for intermittent Mobitz type I, II, or high-degree AV block, particularly in elderly patients. Similarly, a prolonged His–ventricular (HV) interval suggests that syncope may be due to heart block. His–Purkinje conduction can be challenged by administration of IV procainamide with subsequent marked HV prolongation.22 In general, electrophysiologic testing is less helpful in the evaluation of the sinus node (Table 32.3). Occasionally, sinus node recovery times (SNRTs) can demonstrate prolonged pauses indicative of sinus node dysfunction. Attempted induction of sustained monomorphic ventricular tachycardia (SMVT) consists of programmed electrical stimulation of the right ventricle at two sites (RV apex and RV outflow tract), usually with sequential repetitive drive trains of 400 to 600 milliseconds followed by one, two, or three ventricular extrastimuli. Other protocols attempt to induce SMVT by using more rapid repetitive bursts (300 to 350 milliseconds) in the ventricle. The finding of SMVT is significant and suggests the need for an implantable cardioverter-defibrillator (ICD).
TABLE
32.2 Clinical Features Suggesting Need for Electrophysiologic Testing of Patients with Syncope
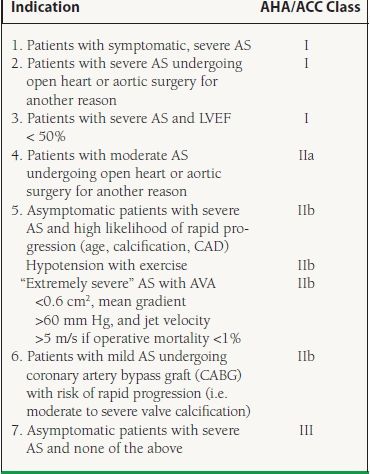
TABLE
32.3 Electrophysiology Study—Components
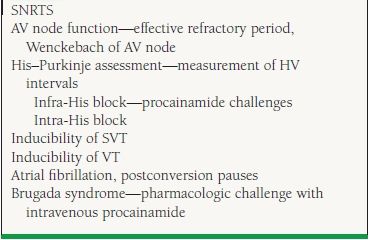
Almost every tachyarrhythmia is amenable to some form of radiofrequency catheter ablation. AV nodal reentry, AV reentry via accessory pathways, and atrial tachycardias are frequently mapped and ablated in a straightforward fashion. In previous decades, EPS was performed much more frequently for syncope evaluation than it is at present. Current clinical practice reserves EPS for a few select cases, such as patients with LV dysfunction, suspected SVTs, conduction abnormalities, and those who may be candidates for radiofrequency ablation. Rarely is EPS performed for syncope in patients with normal hearts and normal ECGs, given the likelihood of a vasovagal cause in this patient subset. Patients who present with syncope in the presence of LV dysfunction, a previous MI, or an EF < 35% to 40% qualify for empiric ICDs given the MADIT 2 and SCD-Heft data.23 There are still several clinical situations in which EPS is performed to evaluate syncope patients (see Table 32.2). American College of Cardiology/American Heart Association (ACC/AHA) guidelines are listed in Table 32.4.
TABLE
32.4 Guidelines for EPS for Patients with Syncope
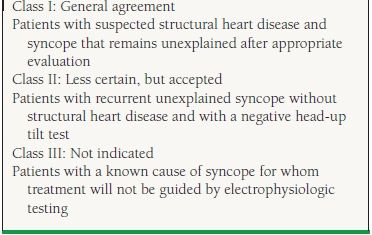
From Zipes DP, DiMarco JP, Gillette PC, et al. Guidelines for clinical intracardiac electrophysiological and catheter ablation procedures: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Clinical Intracardiac Electrophysiologic and Catheter Ablation Procedures), developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol. 1995;26: 555–573, with permission from Elsevier.
SPECIFIC ETIOLOGIES OF SYNCOPE
Neurally Mediated Syncope
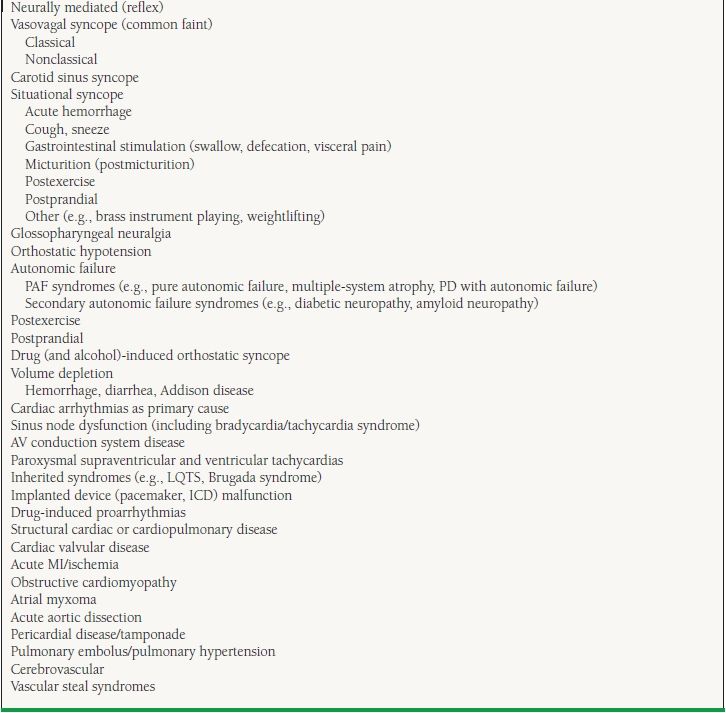
Vasovagal syncope (also called neurocardiogenic syncope, empty heart syndrome, and ventricular syncope) is the most common of the neurally mediated syncopes. All of these syndromes result from disturbances or perturbations of the autonomic nervous system. A partial list of some of the more commonly observed neurally mediated syncopes is given in Table 32.5. Syncope arising from aortic stenosis or hypertrophic obstructive cardiomyopathy is felt to have a significant neurally mediated component and may precipitate the stimulation of C fibers in the posterior left ventricle in a fashion similar to vasovagal syncope (Bezold–Jarisch reflex).8 In addition, it is suspected that in patients with syncope due to recurrent atrial fibrillation, SVT, or VT, there may also be a neurally mediated component in which atrial vasodepressor reflexes result in significant vasodepression, causing a drop in blood pressure and contributing to the LOC independent of a low cardiac output.
< div class='tao-gold-member'>