Fig. 14.1
Early endocardial lesion set – proposed by Melo, based on bilateral isolation of pulmonary veins with LAA closure
Radiofrequency
Unipolar, unipolar with irrigated cooling, and bipolar systems with irrigated cooling are available in the market. The unipolar probes are used mainly endocardially, though there have been reports of unipolar epicardial applications also. Bipolar radiogrequency ablation is usually for epicardial ablation. Most bipolar systems have a flaw in that high impedance is often equated with a transmural lesion. Probably, the bipolar systems have some advantage in creating trans-mural lesions because of capture of the tissue between the electrodes. However, bunching of the tissue and incomplete coverage may be an issue. Furthermore, connecting lesions to remote areas of the left and right atrium are impossible to achieve. Although lesions sets created with radiofrequency energy vary, results are similar: AF is ablated in 70–80 % of patients [15–17]. Perioperative AF after radiofrequency ablation is common, occurring in approximately two-thirds of patients [18] (Figs. 14.2, 14.3, and 14.4).



Fig. 14.2
Cobra-adhere – Unipolar Radio-frequency ablation device. This device delivers unipolar radio-frequency to the atrial along with some weak suction to promote contact of the electrodes with the tissue

Fig. 14.3
Shows Medtronic Cardioblate, a bipolar Irrigated Radio-frequency Ablation Device, that has been used widely in Europe
Fig. 14.4
(a, b) Shows the new nContact probe, that utilizes irrigated unipolar radio-frequency and suction based tissue adhesion during lesion creation
Microwave
Cryo-ablation
Sueda and colleagues reported successful ablation using cryothermy ablation [12]. Gaita and coworkers have reported limited left atrial cryoablation combined with isolation of the pulmonary veins cures AF in approximately 70 % of patients [21] (Figs. 14.5, 14.6, and 14.7).
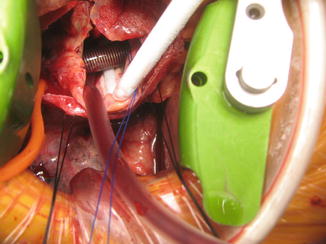
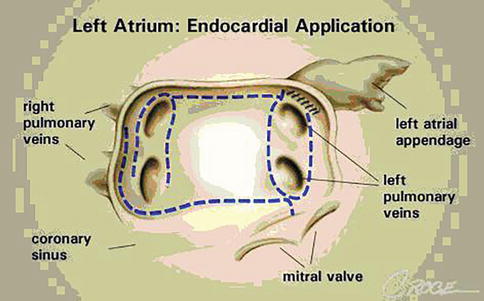

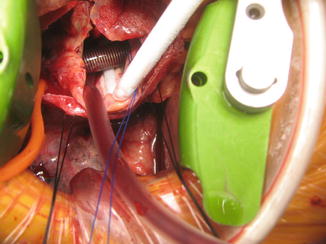
Fig. 14.5
This operative photograph of a mini-thoracotomy Maze procedure. It shows the flexible SurgiFrost, with the malleable cryo-probe inside the right atrium, adherent to the inner wall with cryotherapy while going around the venous cannula
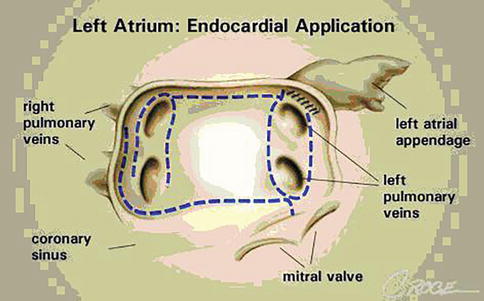
Fig. 14.6
Shows the proposed lesion sets on the right and left atria, that have the best likelihood of replicating the Cox-maze 3 lines of block with a variety of energy sources

Fig. 14.7
Shows the proposed lesion sets on the right and left atria, that have the best likelihood of replicating the Cox-maze 3 lines of block with a variety of energy sources
The Issue of Transmurality in Surgical Ablation for Atrial Fibrillation
The only goal of producing lesions with any ablation tool is the substitution of conducting tissue by non-conducting, scar tissue. The golden standard has been supposedly set by the “cut and sew” technique in the original Cox-Maze procedure. This is a “gold standard” that few discerning surgeons and even fewer in the cardiological community accept. In percutaneous ablation approaches, cardiologists have translated this goal in achieving conduction block as evidenced by electrophysiological measurements. The percutaneous approach allows checking for conduction block during the intervention. In line with the Maze procedure, surgeons redefined this goal into the production of histologically transmural lesions. In contrast to their Cardiology colleagues, they can check the histological quality of their lesions only by indirect means. Despite excellent clinical results obtained by surgeons in treating atrial fibrillation, recent studies have shown that the establishment of histologically transmural lesions is not as obvious as generally assumed. The question is whether this is important for our routine ablation procedures, and if so, how should we deal with it, based on the current evidence available [22–25].
Tissue characteristics considerably influence the continuity of lesions and lesion depth in the first place. The thickness of the atrial wall may vary tenfold within one ablation line. Similarly, the amount of fat tissue present in the different areas around the pulmonary veins shows a high intra and inter-individual variability. Furthermore, trabeculated areas creating bridges from isolated regions to normal conducting tissue may be responsible for persistent conduction. In the elderly and in patients with manifest hypertrophy of the atrial tissue, the presence of scattered fibrosis may offer another hurdle for ablation techniques to make smooth, consistent lesions. The temperature of the tissue and its surroundings is also likely to affect the lesion depth but poorly studied in the clinical setting. Beating heart versus the arrested heart, hypothermic perfusion versus normothermic perfusion, epicardial versus endocardial, all these approaches offer different environmental conditions for the ablation tools. An experimental study suggested that with radiofrequency ablation the endocardial approach is more effective than the epicardial approach. It is very likely that these unpredictable and mostly uncontrollable conditions determine the quality of a lesion set rather than the energy source used for the ablation or the design of the tool [26].
Most information on the quality of ablation lesions has been offered by studies on isolating pulmonary veins. The human anatomy allows ablation of the pulmonary veins, one by one, two by two, and sometimes, all four or five together in one encircling. The existence of an entrance and exit block between the pulmonary vein area and the atrial tissue, proving electrophysiological isolation, can thus be easily determined by monitoring the EKG during pacing from within and outside the isolated area. From such studies, the need for transmurality and the equivalence between transmurality and electrophysiological isolation, has been questioned. First, it was shown that transmurality may not be obtained until several weeks after ablation whereas electrical isolation is achieved immediately during the procedure suggesting that lesions may develop in time. Secondly, an autopsy study revealed that certain patients in sinus rhythm with proven conduction block during surgery, appear to have incomplete continuity of their lesion set and partially, incomplete transmural lesions at autopsy [26]. This observation was confirmed in a study in which 58 ablation lesions from seven patients who died between 2 and 22 days postoperatively, were studied [27]. These seven patients had a concomitant anti- arrhythmic procedure using saline irrigated cooled tip radiofrequency ablation (SICTRA) to treat permanent AF. Histological examination showed transmurality in 96–100 % of the SICTRA lesions at the pulmonary vein orifices and the posterior left atrial wall, but only in 14 % of the left atrial isthmus lesions, resulting in an overall transmurality rate of 76 % of the induced SICTRA lesions. Finally, it was demonstrated that in a large group of patients with clinically successful treatment and proven electrophysiological block initially during the intervention, conduction block was lost several months after the ablation procedure without recurrence of atrial fibrillation [28]. What all these means clinically is open to question. The left atrial isthmus lesion along with the coronary sinus lesion were insisted as being essential by Cox, based on anecdotal experience with a few patients and this may in itself be fallacious.
From these observations one can only conclude that our current understanding of the success of our ablation procedures is at least incomplete. In an effort to address this problem, a recent experimental study showed that the effect of isolating the pulmonary veins is not an all-or-none phenomenon. Complete isolation of the pulmonary veins revealed a 100 % success rate. However, if deliberately a gap was left in the encircling of the veins, still a very significant reduction of the susceptibility of the atrial tissue for atrial fibrillation was observed [20]. However, these were animal studies not conducted in a chronic AF model. These findings may offer an explanation for the discrepancy between the claims and reality of relatively high success rate of today’s pulmonary veins ablation procedures despite the conflicting data about continuity and transmurality of the lesions produced by these techniques. Apparently, these procedures not only affect the pulmonary veins but other structures involved in the initiation or maintenance of atrial fibrillation as well [29–33].
Transmurality has become an important issue, partly because several companies claim that their tools create transmural lesions suggesting that others don’t. Comparative, clinical studies are in progress but do not yet allow final conclusions on superior efficacy of certain tools. The current clinical impact of the transmurality issue is difficult to assess. A systematic review offered some important hints in this respect. The results of the classic “cut and sew” Cox-maze III procedures were compared to results of procedures using alternative sources of energy to obtain a bi-atrial lesion pattern. Patients in the first group had a 85.3 % post-operative SR conversion rate versus 79.7 % in the ablation group. If this difference of 5.6 % can be completely attributed to problems in achieving transmurality, the impact is distinct but small [11]. This may also be partly due to inadequate appreciation of the limitations of each of the alternative energy sources by the surgeons.
Based on the currently available evidence, one might conclude that histological transmurality is not a prerequisite for clinical success. Measuring the occurrence of a conduction block during ablation is an informative but not conclusive tool to determine successful treatment. Sophisticated mapping techniques might appear necessary to guide ablation strategies and control its efficacy in the future. More comparative clinical as well as experimental studies are needed to test the effectiveness of various ablation tools in this respect. The ultimate target for more successful ablation procedures has yet to be defined.
Results
In general the results of all ablation-based surgical procedures range around 70 % sinus rhythm at 6 months post-operatively. Neither energy source nor surgical technique (excluding the classic Maze III procedure) has been found to be superior. The reason for this is probably multi-factorial, including lack of transmural lesions in many cases, different lines of ablation, and different patient selection as compared to that in Cox’s reports [12, 15]. As mentioned before, this may be partly because of misleading advertising by the various vendors: surgeons using the techniques are not as familiar with the limitations of their energy sources as cutting-and-sewing! Another reason for the lack of a clear difference between the various procedures was suggested by Thomas and coworkers, who reported that pulmonary vein isolation is indeed an advantage; however, freedom from AF was demonstrated in a significant number of cases without completely successful pulmonary vein isolation [20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


