Supraventricular Tachycardias
Supraventricular tachycardias (SVTs) continue to be the most common as well as most diverse type of cardiac arrhythmias. SVTs occur in all age-groups and are associated with a wide range of etiologies, heart rates, frequency, and severity of heart disease. The numerous potential mechanisms and variety of descriptive adjectives for these arrhythmias make establishing a succinct classification system difficult. Approaches to classification of SVT include (a) clinical behavior (i.e., paroxysmal, persistent, permanent, sustained, nonsustained and chronic), (b) mechanism (i.e., ectopic, reentrant, reciprocating, slow/fast, fast/slow, orthodromic, and antidromic), (c) electrocardiographic appearance (i.e., narrow or wide QRS), and finally (d) location (i.e., sinus, atrial, and atrioventricular [AV] nodal/junctional). These types of classifications may provide important information in the diagnosis and treatment of SVTs. Clinicians often have difficulty determining a consistent and inclusive comprehensive management algorithm that may be applied to all forms of SVTs. This chapter briefly reviews the most common SVTs and also provides a concise approach to diagnosis that incorporates all four methods of classification.
Symptoms of SVT may range from none to profoundly disabling. SVT generally presents with a variety of symptoms, the most common of which is palpitations. Palpitations may be accompanied by shortness of breath, chest pain, lightheadedness, near-syncope, and/or syncope. The cardiac evaluation of palpitations may include electrocardiography, ambulatory Holter monitoring, cardiac event recording, transtelephonic monitoring, and, less commonly, an implantable loop recorder. The goals of this diagnostic process are twofold. First, it is necessary to document the arrhythmia. Second, it is helpful to correlate symptoms with the documented arrhythmia. Although ambulatory Holter monitoring is easy to obtain and thus frequently ordered for patients with suspected SVT, its diagnostic yield is very low. Symptoms and simultaneous electrocardiographic abnormalities are observed in only 2% to 13% of 24-hour ambulatory Holter monitors. In contrast, patient-activated cardiac event recorders provide a greater yield and are more cost-effective than ambulatory Holter monitoring in the correlation of arrhythmia with transient symptoms.1
Implantable loop recorders are placed subcutaneously at a parasternal chest site, similar to a pacemaker. These monitors can record arrhythmias for more than a year. They record when activated by an external trigger or following automatic programmed parameters within the device. Because implantation of this device is considered invasive, it is reserved for patients with severe symptoms associated with presumed tachyarrhythmic episodes or those with very rare occurrences that are difficult to diagnose with less invasive testing modalities.
APPROACHING SUPRAVENTRICULAR TACHYCARDIA: AV NODE DEPENDENT VERSUS ATRIAL AND SINUS NODE DEPENDENT
In terms of evaluating arrhythmias based on site of origin, there are three types of SVT: (a) sinus node dependent (sinus tachycardia, inappropriate sinus tachycardia, and sinus node reentry), (b) atrial dependent (atrial tachycardia, atrial flutter, and atrial fibrillation), and (c) AV node/junction dependent (atrioventricular node reentry tachycardia [AVNRT] and atrioventricular reciprocating tachycardia [AVRT]). The first step in classifying SVTs is to differentiate sinus and atrial tachycardias from AV node/junctional tachycardias.2,3 This difference is easiest to see if the tachycardia is observed during changes in AV node conduction. AV node conduction can be altered by a change in vagal tone or with medications such as calcium channel blockers or adenosine. If spontaneous changes in vagal tone do not change AV node conduction, maneuvers may be performed to prolong AV node conduction and refractoriness. Physiologic maneuvers include deep breathing, carotid sinus massage, the strain phase of the Valsalva maneuver, and facial immersion. Carotid sinus massage increases vagal tone and is easily performed at the bedside. In older patients, it is important to exclude the presence of significant carotid artery atherosclerotic disease before performing carotid sinus massage. The “diving reflex” may be applied with pediatric patients. This can be done by placing a plastic bag filled with ice water on the patient ’s face for 15 to 20 seconds. Though this maneuver may be effective, it is less well tolerated and therefore not frequently used.
If physiologic maneuvers are unsuccessful, drugs may be used to alter AV node conduction. Edrophonium chloride (Tensilon) was used classically because its potent vagotonic effect creates temporary AV node block; however, it is often poorly tolerated and therefore is no longer commonly used. Verapamil and diltiazem can also be used to create temporary AV node block. These calcium channel–blocking medications have a slow onset, allowing for a “gentler” diagnosis than sudden AV node block. However, calcium channel blockers have potential for side effects such as hypotension. Adenosine is the most commonly used drug for this purpose because of its extremely short half-life. Adenosine provides a very transient AV nodal block. This effect is maximized when it is administered in a rapid intravenous bolus via a central vein. Care must be taken when administered in patients with bronchospasm as it may exacerbate their reactive airway disease.
Observing tachycardia behavior during slowed AV nodal conduction or AV block may help differentiate between sinus/atrial and AV nodal/junctional tachycardias. Perpetuation of the tachycardia, despite AV block occurs primarily with atrial/sinus tachycardias (Fig. 29.1). Termination of the tachycardia as a result of AV block often implicates the AV node as an essential part of the tachycardia circuit (thus an AV node/junctional-dependent tachycardia). There are rare exceptions to this rule. First, some atrial tachycardias terminate with adenosine administration. However, these atrial tachycardias often slow gradually before terminating, as compared to AV node–dependent arrhythmias, which terminate suddenly. Additionally, if the tachycardia breaks spontaneously, examining the termination can provide insight as to whether the tachycardia is atrial/sinus or AV nodal/junctional. If the tachycardia terminates with a P wave that is not followed by a QRS (Fig. 29.2), it is most consistent with an AV nodal/junctional-dependent tachycardia. This is best explained by understanding that if the rhythm had been an atrial tachycardia, it would have had to terminate at the atrial focus and develop AV block simultaneously, which is very unlikely.
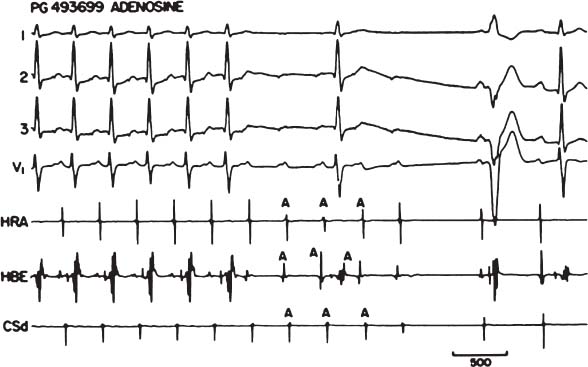
FIGURE 29.1 Atrial tachycardia terminating following the administration of adenosine demonstrating continuation of the atrial tachycardia despite block in the AV node. This would imply that the tachycardia is not AV nodal dependent.
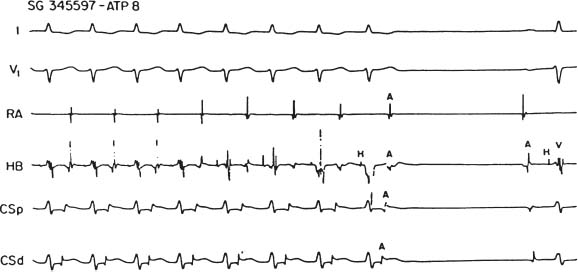
FIGURE 29.2 AV nodal/junctional-dependent tachycardia.
Other electrocardiographic findings are helpful in distinguishing sinus/atrial-dependent from AV nodal/junctional-dependent tachycardia. The P-wave axis indicates the origin of atrial depolarization, which may help differentiate sinus/atrial from AV junction tachycardia. A “high to low” activation sequence is manifested by a surface electrocardiogram positive P-wave deflection in the inferior leads. This is most consistent with a sinus or high atrial tachycardia. AV junctional tachycardias must activate the atria from the area at the AV ring (often near the AV node), leading to “low to high” activation and negative P-waves in the inferior leads.
If the tachycardia appears to have a 1:1 P:QRS relationship, examining the relationship of the R wave to the following P wave may provide additional information to differentiate between sinus/atrial versus AV nodal/junctional tachycardias. If the distance from the R to the following P wave is >50% of the R–R distance, the tachycardia is termed “short RP”. If the distance from the R to the following P is <50% of the R—R distance, the tachycardia is termed “long RP” A short RP interval is more often seen in AV nodal/junctional-dependent tachycardias (AVNRT and AVRT) and a long RP interval is more often seen in sinus/atrial tachycardias. However, this rule also has exceptions that should be noted. Long RP tachycardias, though typically indicative of sinus/atrial dependence, can be seen in atypical (fast–slow) AVNRT or in an unusual form of AVRT that occurs with an accessory pathway (AP) that displays decremental properties. This is seen in the permanent form of junctional reciprocating tachycardia (PJRT). Also, sinus or ectopic tachycardias with a long first-degree AV block may present with a short R–P interval.
In <50% of patients, an appreciable P wave may not be clearly distinct from the QRS. This is because the P wave is hidden within the QRS complex or because the rate and artifact of the tachycardia mask the P wave. In typical AV node reentrant tachycardia the P wave generally occurs simultaneously with the QRS. In this arrhythmia, the P wave is often inscribed in the terminal portion of the QRS and results in pseudo-R ’ deflection in V1 or S wave in II, III, and aVF. However, appreciation of this change may require comparison of this QRS during tachycardia with the QRS when in normal sinus rhythm (Fig. 29.3).
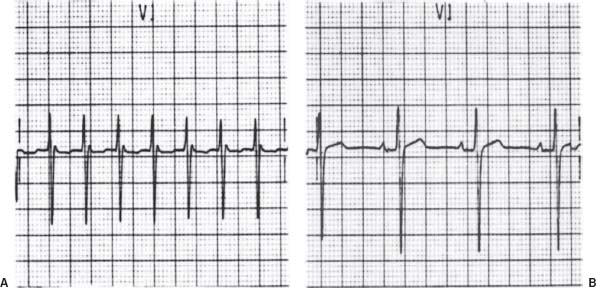
FIGURE 29.3 A: ECG in typical AV node re-entrant tachycardia. B: ECG in normal sinus rhythm.
AV NODE-DEPENDENT TACHYCARDIAS: AVNRT VERSUS AVRT
Once the above methods lead to establishing that the rhythm is AV nodal dependent, further evaluation is needed to determine what type of AV nodal tachycardia is present. AV node–dependent tachycardias include (a) AVNRT and (b) AVRT using an AP.
AV Nodal Reentry Tachycardia
Clinical Presentation and Diagnosis
In patients without ventricular pre-excitation in sinus rhythm, typical AVNRT is the most common mechanism of SVT, accounting for >60% of presenting SVTs.4–6 As shown in Table 29.1, AVNRT is seen in children as well as in the elderly; however, it is most common in the fourth decade. This arrhythmia affects women more often than men, as women represent two-thirds of the patients with AVNRT. This arrhythmia is not associated with structural heart disease. Although palpitations are the primary symptom of this arrhythmia, syncope and near-syncope have been observed, most notably in elderly patients. Because the right atrium is activated nearly simultaneously with the right ventricle, it is often contracting against a closed tricuspid valve, causing many patients to feel neck fullness. Canon A waves can be seen on physical exam. Because this is an AV node–dependent arrhythmia, termination can be achieved with AV nodal blockade. Onset and termination are characteristically abrupt. AVNRT is often triggered by a premature atrial beat which finds the fast pathway refractory and conducts down the slow pathway with associated PR prolongation consistent with dual AV node physiology AVNRT typically terminates with a retrograde P wave (negative P-wave axis in the inferior leads) without a subsequent QRS indicating AV block and dependence of the tachycardia on AV nodal conduction. Because the majority of the reentry circuit is within the AV node, the atrial and ventricular activation are nearly simultaneous; thus, this is a “short RP” tachycardia. The retrograde P wave is frequently hidden within the QRS complex.
TABLE
29.1 Narrow-QRS Tachycardia: Clinical and Electrophysiologic Characteristics
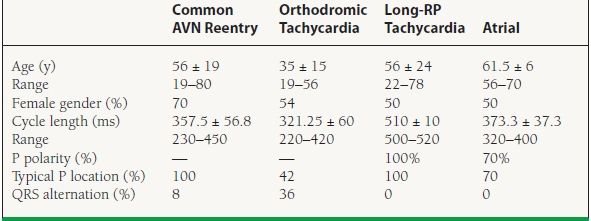
Diagnostic categories listed in the table represent the final diagnosis made at electrophysiology study. P polarity was not identifiable in AV node reentry and orthodromic tachycardia.
Mechanism
The electrophysiologic circuit of AVNRT uses regions of tissue within or adjacent to the AV node that possess different electrophysiologic properties. Patients with AVNRT have dual AV nodal physiology. Within or near the AV node there is a fast conducting pathway with a long refractory period and a slower conducting pathway with a shorter refractory period. In typical AVNRT (slow–fast form) there is antegrade conduction over the slower pathway and retrograde conduction over the fast pathway (Fig. 29.4). AVNRT typically initiates with a premature atrial beat that arrives at the AV node when the fast pathway is still refractory (longer refractory time), but the slow pathway is able to conduct antegrade. However, because of the slower conduction, by the time the impulse arrives to the compact AV node, the fast pathway has recovered and is able to conduct retrograde back up to the atrium. Thus, typical AVNRT is down the slow pathway and up the fast pathway. Because the atria are activated via the fast pathway, the retrograde P wave is very close to (or buried within) the QRS. As mentioned previously, ECG lead V1 may reveal a pseudo-R prime pattern due to deformation of the terminal portion of the QRS complex by the retrograde P wave. This ECG finding is very specific for AVNRT.
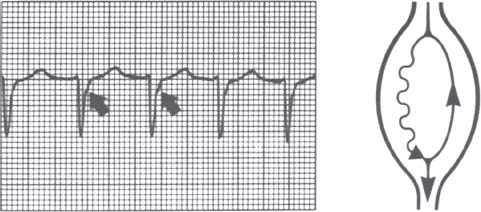
FIGURE 29.4 Typical AVNRT denoting superimposed P waves and retrograde atrial depolarization (arrows).
In the unusual variety or “atypical” AVNRT, antegrade conduction occurs over the fast pathway and retrograde conduction over the slow or intermediate pathway. Though this “atypical” form uses a similar mechanism (dual AV node physiology), although in reverse, it results in a long RP (retrograde slow conduction) and a short PR (fast antegrade conduction) interval. This atypical AVNRT is still AV node dependent and thus may terminate with adenosine or during any change in AV nodal conduction properties.
Treatment
Because both typical and atypical AVNRT are manifestations of dual AV node physiology, they are treated in the same fashion. Patients with unstable hemodynamics should undergo immediate cardioversion. In the acute setting, a hemodynamically stable patient is typically responsive to vagal maneuvers or adenosine. If those are not successful at terminating the tachycardia then an intravenous formulation of beta-blockers and calcium channel blockers may be utilized. If the patient has recurrent arrhythmic episodes, longer-acting medications that alter AV node conduction (including beta-blockers and calcium antagonists) may be used. Though medications can be successful, catheter ablation is considered the treatment of choice. Ablation is a Class I recommendation for patients with one or more episodes of AVNRT who desire resolution of the arrhythmia and patients with recurrent symptomatic or poorly tolerated AVNRT episodes. Catheter ablation of either form of AV node reentry consists of an anatomic ablation of the slow pathway located at the posterior input to the AV node. This area is most often bordered by the coronary sinus and the tendon of Todaro posteriorly and the tricuspid annulus anteriorly. Once identified, radiofrequency or cryotherapy ablation or modification of the slow pathway is performed to the point where tachycardia is no longer inducible.
AV Reciprocating Tachycardia and Ventricular Pre-excitation (Wolff–Parkinson–White Syndrome)
Clinical Presentation and Diagnosis
Accessory AV connections or pathways may also participate in AV nodal–dependent reentrant arrhythmias. The presence of such an AP may be apparent by surface ECG. Because of the rapid and nondecremental conduction properties of these pathways, they may “pre-excite” the ventricle. Ventricular pre-excitation results in a short PR interval and slurring of the upstroke of the QRS (“delta wave”). This ECG abnormality is termed Wolff–Parkinson–White (WPW) pattern. The term WPW syndrome is reserved for patients who also have clinical SVT. It is estimated that 1 to 1.5 in 1,000 ECGs show a WPW pattern. Population-based studies have indicated that 50% to 60% of patients with WPW pattern demonstrate symptoms that may include palpitations or more severe symptoms such as syncope.7 Approximately 85% of such symptomatic patients have AV reentrant tachycardia using the AV node as the antegrade limb and the AP as the retrograde limb of the circuit.8,9 Approximately 30% to 40% of patients with WPW are capable of sustaining atrial fibrillation.
This type of tachycardia is not only dependent on the AV node but requires the presence of an AP. This pathway provides an additional connection between the atria and ventricles, other than the AV node. The term “pre-excitation” stems from the fact that the ventricle receives electrical activation from both the AV node-His-Purkinje system (AVN-HPS) and the AP Because antegrade conduction via the AP is not decremental as with the AV node, the ventricle is activated via the pathway before the AVN-HPS activation. This pre-excitation is represented by the delta wave on the ECG. When there is evidence of ventricular pre-excitation by ECG at baseline, the AP is described as “manifest.” This pre-excitation tends to be more evident at more rapid atrial rates, when AV nodal conduction is slowed, making preexcitation even more apparent. Occasionally, conduction through the AV node is preferred to that over the AP. This may be secondary to slow or poor antegrade conduction in the AP or to the location of the pathway. In these patients there may be minimal or no delta wave on the ECG, as the ventricle is predominantly or completely activated via the AV node. The AP is still present and may be able to conduct retrograde (and thus be able to cause tachycardia), but it is not evident in sinus rhythm. These APs are termed “concealed.”
It is important to remember that the presence of an AP does not always indicate that this pathway is a critical part of the presenting SVT. For this reason it is important first to determine the role of the AV node (dependent or independent) in the presenting SVT. APs provide only an additional connection between the atria and ventricles. Patients with an AP and even a history of WPW syndrome may also have other SVTs (i.e., AVNRT) that have no relationship to the AP.
Accessory Pathways
APs may be located along either the mitral or tricuspid annuli. These pathways consist of a bundle of myocardial muscle that bypasses the AV groove with direct insertion on the ventricular myocardium of the right or left ventricle. On rare occasions, the lower insertion is in proximity or attached to the branches of the right bundle. As shown in Table 29.2, of all APs, almost half are located on the left side of the heart along the mitral annulus, nearly one-third are in the posteroseptal region, and the remainder are at the right anteroseptal region or the right lateral wall of the tricuspid annulus.
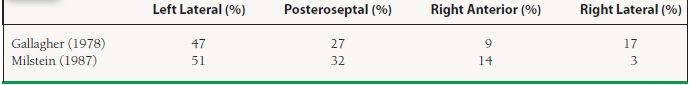
TABLE
29.2 Distribution of Most APs