22 Supraventricular Tachycardia
I. CASE
A. Fetal echocardiography findings
1. Fetal echocardiography reveals situs solitus of the atria, levocardia, and left aortic arch.
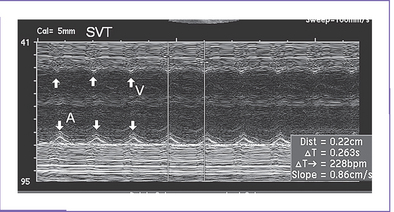
2. Heart rate is 228 bpm, with equal atrial and ventricular rates (Fig. 22-1), suggesting 1:1 ventriculoatrial (VA) or atrioventricular (AV) conduction with a short VA interval (86 ms).
3. Cardiac size is normal (cardiothoracic ratio = 0.33), and cardiac axis and position are normal.
4. The four-chamber view is normal, and ventricles are of equal size.
5. There is no evidence of structural congenital heart disease.
6. The aortic and ductal arches are leftward and of similar size.
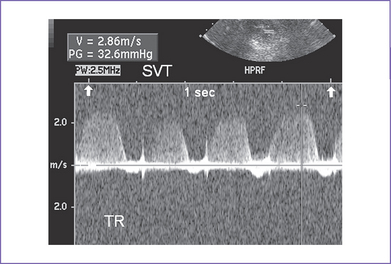
7. Outflow velocities are decreased (0.4 m/s) due to the decreased filling time in tachycardia.
8. The pulmonary venous flow pattern is abnormal (large a wave reversal).
9. Tricuspid and mitral valve holosystolic regurgitation is present (Fig. 22-2), with the additional finding of ascites fluid.
10. Tei indices (myocardial performance index) were not calculated due to the rapid heart rate.
11. The umbilical artery Doppler is normal in the free loop of the umbilical cord with persistent rapid, regular rate.
12. Other venous sites near the heart had large a wave reversal (hepatic vein, ductus venosus), with tachycardia, but the umbilical vein blood velocity has no pulsations.
13. Simultaneous superior vena cava (SVC) and ascending aortic Doppler confirm 1:1 VA association, with a shorter VA than AV interval.
C. Associated syndromes and extracardiac anomalies
None. The detailed level-2 obstetric ultrasound scan was completely normal.
D. Fetal management and counselling
1. Amniocentesis is not indicated. The risk from this procedure is higher than the chance of trisomy with SVT.
2. Initial management of the fetal SVT.
a. Hospital admission was advised for monitoring the fetal heart rate and the mother’s health during administration of antiarrhythmic medications.
b. The mother was fully evaluated by adult cardiology with a baseline electrocardiogram (ECG) and echocardiogram to exclude obvious cardiac pathology that would place her at risk in administering antiarrhythmic medications. Thyroid function testing was normal.
c. Management of the fetal SVT was discussed with the mother and her partner. It was explained that in more than 80% of patients, control of the dysrhythmia is possible, but occasionally this requires more than one medication and monitoring until the mother is on a sufficient dose of the medication that controls the fetal dysrhythmia.
d. With or without rhythm control, there is a small risk of a sudden fetal event or the development of fetal hydrops (particularly without control) as well as risks of other morbidities (e.g., stroke).
3. Daily fetal echo assessments included:
a. Progression of hydrops signs (pleural effusion, ascites, increasing pericardial fluid).
b. Increasing size indicating compromise of heart function.
c. Valve function for increasing degrees of tricuspid and mitral regurgitation. The dP/dt (change in pressure per change in time) can be assessed on AV valve regurgitation jets. Normal is greater than 1000 mm Hg per second, and a poor prognosis is associated with values less than 400 mm Hg per second.
d. Semilunar valve regurgitation, which is a sign of progression in myocardial dysfunction.
e. Myocardial function, which can be measured with the Tei index in sinus rhythm after conversion.
f. Venous Doppler assessment for signs of improvement.
a. Baseline maternal 12-lead ECG was performed, which showed a prolonged PR interval of 0.25 seconds with no other abnormality and normal QTc.
b. The mother was tested (hematology) for hyperthyroidism and infection. Consultation with adult cardiology was obtained, and her exam and echocardiogram were normal.
F. Neonatal management
1. On admission, the neonate was active, with no obvious malformation and normal vital signs.
2. The baby was normal and had a normal ECG with preexcitation.
3. Endocrinology consultation was obtained, and thyroid studies were performed; results were normal.
4. A 24-hour Holter monitor was normal.
5. A two-dimensional Doppler echocardiogram was normal.
H. Outcome of this case
a. The newborn had appropriate birth weight and Apgar scores of 9 at 1 minute and 9 at 5 minutes.
b. The baby was monitored in the intensive care unit (ICU) for 24 hours, and the rhythm was normal at 130 to 150 bpm.
d. Postnatal echocardiogram confirmed a structurally normal heart. The rhythm was normal sinus rhythm.
e. He was started on digoxin 5 mg/kg PO twice daily, and feeding was started.
f. He was discharged after 2 days.
g. Cord blood digoxin level was 80% for the newborn postnatal value.
h. The ECG was normal at all visits with no sign of a delta wave.
i. The baby was followed in cardiology every 2 months with ECG and Holter monitor, and digoxin dose adjustments were made based on weight increase.
j. At 1 year of age the digoxin was stopped.
k. No tachycardia occurred after birth.
II. YOUR HANDY REFERENCE
A. Prevalence
1. The actual prevalence of fetal tachyarrhythmia is not known.
a. The most common fetal tachycardia is SVT, which accounts for 90% of fetal tachycardia.
b. The second most common form of fetal tachycardia is atrial flutter and is seen in 10% to 30% of patients. Atrial pulsations in the IVC at greater than 400 bpm are a clue to the diagnosis.
c. Ventricular tachycardia in the fetus is relatively rare and accounts for less than 5% of fetal tachycardia. One clue to this diagnosis is a tachycardia rate of less than 225 bpm with signs of congestive heart failure (CHF).
2. Fetal arrhythmia can occur at any gestational age, but it is most commonly seen after 24 weeks of pregnancy. Tachycardia before 20 weeks of gestation raises the likelihood of infection or maternal drug ingestion or hyperthyroidism.
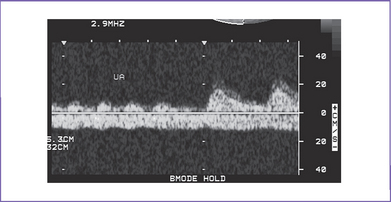
3. The risk of tachycardia is highest in fetuses with multiple blocked atrial premature beats leading to a low ventricular rate (atrial bigeminy). The vast majority of fetuses with atrial and ventricular premature beats without tachycardia have uneventful prenatal and postnatal outcome. Intermittent SVT should be monitored to assess what portion of the whole day the fetus is in SVT (Fig. 22-3).
4. Fetal tachycardia is associated with structural cardiac anomalies in 1% to 5% of cases.
a. The most commonly described associations with SVT are Ebstein’s anomaly and myocardial tumors, particularly rhabdomyoma.
b. Myocardial tumors and cardiomyopathy may be present in fetal ventricular tachycardia.
B. Outcome
1. In fetuses with SVT who were treated in utero, the postnatal outcome is complicated by recurrence of tachyarrhythmia in about 50% of the neonates.
2. In only 10% to 20% of infants does the tachycardia persist beyond the first year of life.
3. Fetal atrial ectopic (AET) and permanent (paroxysmal) junctional reciprocal tachycardia (PJRT) often persist after birth, and long-term antiarrhythmic therapy or electrophysiologic intervention may be necessary.
4. At 1 year of age, roughly one third of fetal SVT patients remain clinically symptomatic. One third do not have clinical tachycardia, but tachycardia can be induced using esophageal stimulation. In one third, tachycardia can no longer be induced, and presumably the bypass tract no longer conducts.
C. In utero diagnosis of fetal tachyarrhythmia
1. The majority of fetal tachyarrhythmias are detected during Doppler assessment of the fetal heart beat at routine obstetrics clinic visits in the second and third trimesters of pregnancy.
2. If monitoring of the fetal heart rate by ultrasound, continuous wave Doppler, or cardiotocography reveals, at any point, fetal arrhythmia (an irregular, rapid, or slow fetal heart rate), one should consider referring the mother for further evaluation by fetal ultrasound and fetal echocardiography. For persistently high or low rates at assessment, the referral should be immediate, given the potential risk of compromise and need for accurate diagnosis to plan management and intervention where possible.
3. Polyhydramnios and fetal hydrops can lead to detection of an underlying fetal tachyarrhythmia and should be considered in the setting where there is unexplained fetal hydrops. One might even consider continuous fetal heart rate monitoring or frequent Doppler assessment every day to exclude or confirm fetal tachyarrhythmia as a primary cause.
D. Mechanisms of fetal arrhythmias
1. The definition of an abnormally fast heart rate depends on the gestational age of the fetus.
a. The fetal heart rates that have been observed in normal pregnancy are 90 bpm at 6 weeks, increasing to 160 to 180 bpm by 9 weeks.
b. The heart rate falls to 140 bpm ± 20 bpm by 20 weeks, and again to 130 bpm ± 20 bpm near term.
c. A fetal heart rate in excess of 180 bpm is abnormal.
2. The high incidence of atrioventricular reentry tachycardia (AVRT) or, similarly, unidirectional reciprocating accessory pathway tachycardia (URAP) during fetal and neonatal life and its decrease due to the spontaneous disappearance of SVT can suggest immaturity of the myocardium. In particular, these tachycardias suggest a delayed development of the annulus fibrosus and/or prolonged persistence of accessory AV pathways.
3. Fetal atrial flutter is rare, and atrial fibrillation to date has not been reported in a fetus.
a. Atrial flutter is generated within the atria by an atrial reentrant circuit and is observed mainly during the third trimester. This supports the hypotheses of an atrial macroreentry as an underlying mechanism of fetal atrial flutter.
b. It might resolve spontaneously or progress to hydrops and death.
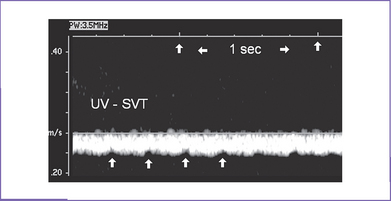
c. Incessant heart rates as high as 300 bpm can lead to hydrops in 2 to 3 days (Fig. 22-4) and manifest umbilical venous pulsations.
4. The pathophysiology in SVT of the human fetus includes an impeded ventricular filling due to a short, inadequate diastolic period. This can alter the ventricular filling either directly or by changes in diastolic ventricular function due to inadequate oxygen supply by the reduced myocardial flow. Both mechanisms can elevate the venous pressure, resulting in increased rates of transcapillary fluid filtration into the interstitial space and significant reduction of lymphatic flow. This inadequate reduction in lymphatic drainage results in interstitial edema and finally hydrops (Box 22-1).