Chapter 35
Supraventricular Tachycardia
1. What does the term supraventricular tachycardia (SVT) mean?
2. What is the most common cause of paroxysmal SVT?
AVNRT accounts for 60% to 70% of paroxysmal SVTs, followed by AVRT.
3. What factors are part of the generic workup for supraventricular tachycardia?
 History, including type and duration of symptoms (palpitations, lightheadedness, chest pains, dyspnea, presyncope, precipitating factors)
History, including type and duration of symptoms (palpitations, lightheadedness, chest pains, dyspnea, presyncope, precipitating factors)
 Questions regarding the intake of alcohol, caffeine, and illicit drugs
Questions regarding the intake of alcohol, caffeine, and illicit drugs
 Cardiac history (myocardial infarction, valvular disease, cardiac surgery)
Cardiac history (myocardial infarction, valvular disease, cardiac surgery)
 Physical examination (although often unrevealing)
Physical examination (although often unrevealing)
 12-lead electrocardiogram (ECG) (looking for signs of chamber enlargement, preexcitation, etc.)
12-lead electrocardiogram (ECG) (looking for signs of chamber enlargement, preexcitation, etc.)
 Echocardiogram (often unrevealing because paroxysmal SVT can occur in the absence of structural heart disease, although atrial arrhythmias will often occur in the setting of dilated atria)
Echocardiogram (often unrevealing because paroxysmal SVT can occur in the absence of structural heart disease, although atrial arrhythmias will often occur in the setting of dilated atria)
 Laboratory tests (electrolyte abnormalities, hyperthyroidism)
Laboratory tests (electrolyte abnormalities, hyperthyroidism)
4. What are the causes of narrow complex regular tachycardias (regular referring to fixed R-R intervals—the time or distance between QRS complexes)?
ECGs of the more common SVTs that cause narrow complex regular tachycardias are shown in Figure 35-1.
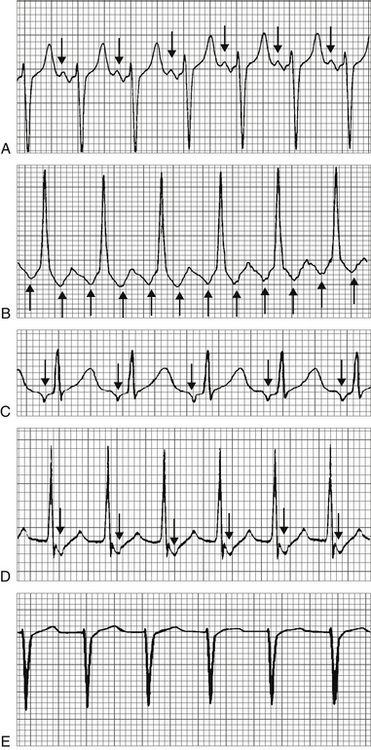
Figure 35-1 SVTs that cause a narrow complex regular tachycardia. A, Sinus tachycardia. Normal appearing P waves (arrows) are present before each QRS complex. B, Atrial tachycardia. Abnormal, inverted P waves (arrows) are present before each QRS complex. C, Atrial flutter. Flutter waves (arrows) are present. There is 2:1 conduction. D, Atrioventricular nodal reentrant tachycardia (AVNRT). No P waves are present before the QRS complexes. Retrograde, inverted P waves (arrows) are visible immediately after the QRS complexes. E, Atrioventricular reentrant tachycardia (AVRT). No P waves are present before the QRS complexes. Although retrograde P waves are sometimes seen in the ST-T segment with AVRT, none are visible in this particular rhythm strip.
 Sinus tachycardia (not really an arrhythmia, but still in the differential diagnosis)
Sinus tachycardia (not really an arrhythmia, but still in the differential diagnosis)
 Rare causes of narrow complex QRS, especially in adults, that are often difficult to diagnose and are more suited for discussion at the cardiology fellow or attending level, include sinoatrial (SA) nodal reentrant tachycardia and focal junctional tachycardia.
Rare causes of narrow complex QRS, especially in adults, that are often difficult to diagnose and are more suited for discussion at the cardiology fellow or attending level, include sinoatrial (SA) nodal reentrant tachycardia and focal junctional tachycardia.
5. What are the causes of narrow complex irregular tachycardias (tachycardias with irregular R-R intervals)?
ECGs of SVTs that cause narrow complex irregular tachycardias are shown in Figure 35-2.
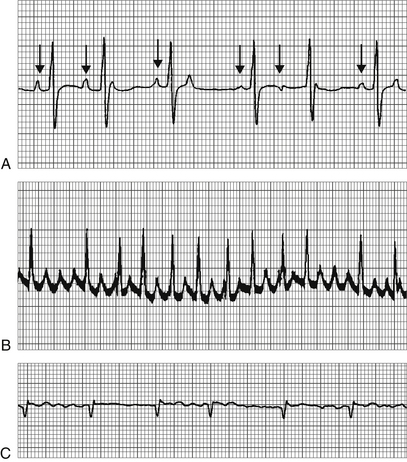
Figure 35-2 Supraventricular tachycardia (SVTs) that cause a narrow complex irregular tachycardia. A, Multifocal atrial tachycardia (MAT). P waves of differing morphologies (arrows) are present before the QRS complexes. B, Atrial flutter with variable block. Flutter waves are intermittently visible between the QRS complexes. C, Atrial fibrillation. No organized atrial activity is present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






