INDICATIONS/CONTRAINDICATIONS
Patients should be thoroughly staged and have no N2 disease when considered for aggressive induction therapy followed by resection for a superior sulcus lung cancer. Generally patients will undergo induction chemoradiotherapy and have restaging CT scans. Resection is performed as long as there is no progressive disease. Relief of pain during induction therapy is a favorable sign for a good therapy response.
Indications
Potentially resectable posterior-based superior sulcus tumor (Figs. 30.1 and 30.2)
Adequate cardiopulmonary function and performance status
Contraindications
Extensive involvement of the brachial plexus
N2 disease
Extensive involvement of the vertebral body (with the caveat that a very few centers of excellence offer combined superior sulcus resections in conjunction with total vertebrectomy with reasonable results)
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Patients with known involvement of the subclavian vessels should have an anterior approach to their tumors to enhance the ability to perform a complete resection. Adequate recovery from induction therapy, both in terms of functional status and hematologic values should be ensured prior to surgery. Generally waiting at least 4 to 6 weeks is prudent before proceeding with surgery following induction therapy. An epidural catheter is usually placed in the induction area for postoperative pain relief.
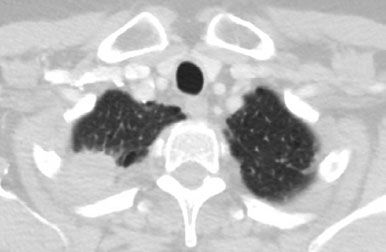
Figure 30.1 Axial CT scan of a patient with a small right superior sulcus lung cancer involving ribs 1, 2, and 3. Induction chemoradiotherapy was administered followed by a posterior approach for resection.
 SURGERY
SURGERY
Positioning
The patient is placed in the lateral decubitus position and carefully padded. Special attention to the arm on the involved side is made so that it is out of the way of the surgeon but not so far abducted or superiorly placed that a nerve stretch injury will occur. Sequential compression devices are placed on the calves to reduce the possibility of deep venous thrombosis. The skin preparation should include the posterior midline and the nape of the neck as the parascapular incision is carried very high onto the back.
Technique
The incision is generally almost entirely a posterior parascapular incision midway between the spine and scapula border (Fig. 30.3). The muscles that are usually transected include the latissimus dorsi, the trapezius, the major and minor rhomboids, the levator scapulae, and the serratus posterior superior (Fig. 30.4). The chest is typically entered in the fourth interspace and the limits of the invasion of the ribs ascertained. Generally the first two or three ribs are involved and require resection. The outer chest wall can be marked with a cautery mark or other marker to guide the surgeon as to where to end the anterior aspect of the chest wall resection. Several centimeters of free rib margin should be planned for. Alternatively a video camera can be inserted in the chest in the beginning and using a needle, the limits of the chest wall resection defined on the outer surface of the ribs. It is helpful to place a chest spreader under the scapula to provide good exposure to the chest wall during this phase of the operation (or use a table-mounted hook retractor).

Figure 30.2 Coronal CT of the same patient demonstrating a small superior sulcus lung cancer.

Figure 30.3 Long posterior parascapular incision, which divides the posterior aspect of the latissimus dorsi and most of the trapezius muscles. The scapula is also marked as well as the spinous processes of the midline.
The chest wall resection usually begins anteriorly from the lowest involved rib taking them sequentially until the first rib is transected (Fig. 30.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


