Sudden Cardiac Death and ICD Therapy
David V. Daniels
Henry Hsia
BACKGROUND
Sudden cardiac death (SCD) is defined as death from cardiovascular causes shortly after the onset of symptoms in a person without a condition that would otherwise appear fatal.1 Estimates as to the impact of SCD on our health care system put the total annual mortality up to 450,000, which is 63% of all deaths from cardiovascular causes.2 Mechanisms of arrhythmic SCD include3,4:
Ventricular arrhythmia (60% to 80%): Most commonly VT → VF, also primary VF, or torsade de pointes
Bradyarrhythmia/asystole
Pulseless electrical activity (PEA)
In a series of young sudden death patients <40 years old without known heart disease, the most common etiology was still cardiac (73%). Coronary heart disease (CHD) was the most common cause in those >30 (58%), while myocarditis (22%), hypertrophic cardiomyopathy (HCM) (22%), and conduction system disease (13%) were more common in those <20 years of age.5 (See Table 7-1.)
TABLE 7-1 Etiologies of sudden death | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
OUTCOMES
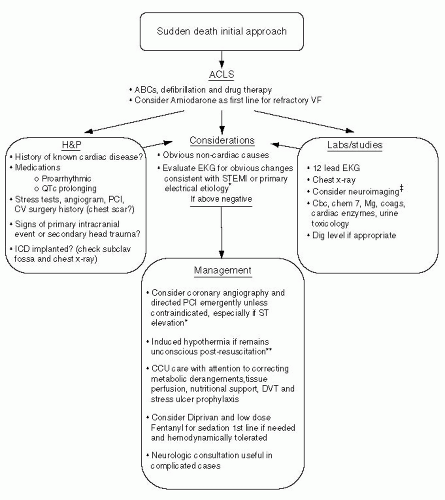
SCD is associated with a high incidence of mortality, and the ability to rescue the patient probably depends most on timely interventions that restore perfusion to and protect vital organs. Unfortunately, many patients will die in the prehospital setting or early in the resuscitative effort. For out-of-hospital sudden death, 20% make it to the hospital, half of them will die in the hospital, and only about half of the survivors will have any “meaningful” survival. Hence in total only about 5% of patients who sustain an out-of-hospital sudden death in the absence of ICD therapy will have a good outcome. In contrast, the survival with early defibrillation when the initial rhythm is VT or VF is substantially higher with up to 40% of those being discharged with a good neurologic outcome and is the single factor most strongly associated with a good outcome.4,6 Those that regain a sustained perfusing rhythm are candidates for further therapy as outlined in Figure 7-1.
INITIAL PREDICTORS OF POOR PROGNOSIS
Prolonged resuscitation time (>20 minutes)
Survival decreases by ˜10% for each minute of lapsed time before restoration of a viable rhythm
Asystole (0% to 2% survival) or pulseless electrical activity (PEA) (11% survival) as the initial rhythm
End tidal CO2 by capnography <10mm Hg after 20 minutes of resuscitation in patients with PEA predicts death with 100% sensitivity and specificity7
SPECIFIC ACUTE THERAPIES
Coronary Angiography and Directed Revascularization8
High degree of obstructive coronary artery disease (CAD) (71%) in an unselected population of SCD
Up to 50% have a totally occluded coronary artery
ST elevation+chest pain are highly predictive of recent coronary occlusion (87%), ST elevation alone (63%)
Up to 25% of those with recent total coronary occlusions have NO pathologic ST elevation
Successful angioplasty is an independent predictor of survival (Odds ratio 5.2)
Therefore, coronary angiography is reasonable in all survivors of SCD, especially in those with persistent ST elevation or antecedent chest pain, but should be considered on an individual basis for all patients given the significant pretest probability of obstructive CAD and potential for decreasing further arrhythmic events
Induced Hypothermia Protocol
Consider for patients who do not regain consciousness immediately after cardiac arrest
Well validated in combination with primary PCI after resuscitation9
Induced hypothermia 32-34 degrees Celsius by cooling blankets, ice packs, or central venous cooling catheter for 24 hours followed by passive rewarming10,11
Monitor temperature with bladder or central venous temperature probe
Sedation with midazolam or Diprivan, analgesia with fentanyl, paralysis with nondepolarizing neuromuscular blocking agent to prevent shivering
Bradycardia is common during hypothermia but seldom requires treatment11
Further Testing
In the absence of CHD, other less common structural, metabolic, and primary electrical etiologies should be considered. The following provide a framework for this investigation:
Review of History
History of known structural heart disease: prior myocardial infarct/coronary artery disease (MI/CAD), hypertrophic cardiomyopathy (HCM), rheumatic heart disease, valvular CM, dilated cardiomyopathy (DCM)
Family history: FH of SCD, LQT syndrome, FH of CAD, WPW, etc.
Medication list: drugs known to cause long QT
Evaluation of the 12-Lead ECG for Primary Electrical Etiologies of SCD
Look for evidence of structural heart disease:
Q waves for transmural scar from prior MI
Evidence of LVH, sarcoidosis (blocks)
Amyloidosis (low volts), epsilon wave for arrhythmogenic right ventricular dysplasia (ARVD)
Consider congenital or acquired long QT syndrome in a patient with significantly prolonged QTc, risk of torsade is low with a QTc <500 milliseconds12
Pre-excitation suggestive of a bypass tract which could → rapid A-V conduction and VF
Brugada syndrome:
Atypical ST elevation in V1-V3, right bundle branch block pattern13
Associated with polymorphic VT and VF
Congenital short QT syndrome:
Very rare, manifest by QTc <300 milliseconds14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree