Case Studies
Introduction
2. Pulseless ventricular tachycardia (VT)/ventricular fibrillation (VF) treated with an automated external defibrillator (AED)
Sample Scenario Sheet
| Emergency Action Steps | Necessary Tasks |
| Scene Survey | Ensures scene safety. Takes or communicates standard precautions. Coach: The scene is safe. |
| Initial Assessment | |
| General Impression | Verbalizes general impression of patient (appearance, breathing, circulation) Coach: The patient is not moving. There is no obvious movement of his chest. His skin looks pale. |
| Primary Survey | |
| Responsiveness/Airway | Assesses airway … Coach: |
| Breathing | Assesses breathing … Coach: |
| Circulation | Assesses pulses, skin (e.g., color, temperature and moisture), estimates heart rate Coach: |
| Defibrillation/Disability | Based on information obtained, determines need for a defibrillator Coach: |
| Secondary Survey | |
| Vital Signs/History | Obtains baseline vital signs, history Coach: |
| Airway, Breathing, Circulation | Assesses need for advanced airway, gives O2, establishes vascular access … Coach: |
| Differential Diagnosis, Evaluates Interventions | Determines treatment plan, begins appropriate care, evaluates patient response, facilitates family presence when applicable Coach: |
| Post-resuscitation Support/Reassessment | |
| Begins Postresuscitation Support/ Performs Reassessment | Repeats initial assessment Coach: |
| Repeats vital signs Coach: | |
| Evaluates response to care Coach: | |
Case 1: Respiratory Arrest
| Objective | Given a patient situation, describe and demonstrate the initial emergency care for a patient who has experienced a respiratory arrest. |
| Skills to Master | Primary and secondary surveys Recognition of a patient with respiratory compromise/arrest Head tilt–chin lift, jaw thrust without head tilt Insertion of an oral or nasal airway Pocket face mask or bag-mask ventilation Upper airway suctioning Attachment and use of electrocardiogram (ECG) monitoring leads Use of a pulse oximeter and capnometer IV access |
| Rhythms to Master | Sinus bradycardia Sinus rhythm Sinus arrhythmia |
| Medications to Master | O2 |
| Related Text Chapters | Chapter 1: The ABCDs of Emergency Cardiovascular Care Chapter 2: Airway Management: Oxygenation and Ventilation |
| Essential Actions | |
| Unacceptable Actions | • Failure to recognize signs of deterioration to respiratory failure or arrest and the need for more aggressive intervention • Failure to monitor the cardiac rhythm in any patient who displays abnormal ventilatory rate or effort, abnormal heart rate, perfusion, blood pressure, or acute altered mental status |
Case 1: Scenario Sheet
| Emergency Action Steps | Necessary Tasks |
| Scene Survey | I am putting on personal protective equipment. Is the scene safe to enter? Coach: The scene is safe. |
| Initial Assessment | |
| General Impression | As I approach the patient and form a general impression (assessing the patient’s appearance, work of breathing, and circulation), what do I see? Coach: You see a woman supine on a stretcher. Her eyes are closed and her hair and clothing are wet. You see no signs of breathing. Her skin looks pale. |
| Primary Survey | |
| Responsiveness/Airway | I will quickly approach the patient and assess her level of responsiveness. Does she respond when I call her name? Coach: There is no response. |
| Does she respond when I pinch her hand? Coach: The patient is unresponsive. | |
| I will open the patient’s airway using a jaw thrust without head tilt maneuver. Do I see anything in the patient’s mouth such as blood, broken teeth or loose dentures, gastric contents, or a foreign object? Coach: You see a small amount of pink fluid in the patient’s mouth. | |
| I will ask an assistant to clear the patient’s upper airway with suctioning. Coach: The airway is now clear. What should be done now? | |
| Breathing | Is the patient breathing? Coach: The patient is not breathing. |
| I will ask the airway team member to size and insert an oral airway and begin positive pressure ventilation with a bag-mask device connected to 100% O2 while I continue the primary survey. I want the airway team member to maintain proper head position and a good seal with the mask against the patient’s face. I want a second team member to assume responsibility for compressing the bag with just enough force to produce gentle chest rise. Coach: An oral airway has been inserted and the patient is being ventilated with a bag-mask. You see gentle chest rise with bagging. At what rate should this patient be ventilated? | |
| The patient should be ventilated at a rate of 10 to 12/min (i.e., one ventilation every 5 to 6 seconds). Each ventilation should be given over 1 second. I will ask an assistant to assess baseline breath sounds while the patient is being ventilated and then prepare the intubation equipment. | |
| Circulation | I will ask the defibrillation team member to attach a pulse oximeter and the ECG monitoring leads while I feel for a carotid pulse for up to 10 seconds. Do I feel a pulse? Coach: A pulse is present. Current resuscitation guidelines generally begin with a C-A-B sequence. You have chosen the traditional A-B-C approach. Why? |
| Hypoxia is the most unfavorable consequence of submersion. CPR for drowning victims requires modification of the C-A-B sequence and involves the use of the traditional A-B-C approach because of the hypoxic nature of the arrest.1 While I am feeling the patient’s pulse, I will assess her skin condition. What is her skin temperature, color, and condition? Coach: The patient’s skin is cool, pale, and wet. What should be done now? | |
| Defibrillation/Disability | I will assess the need for a defibrillator. Because the patient has a slow pulse, defibrillation is not necessary right now. I will ask a team member to obtain the patient’s baseline vital signs while I begin the secondary survey. |
| Secondary Survey | |
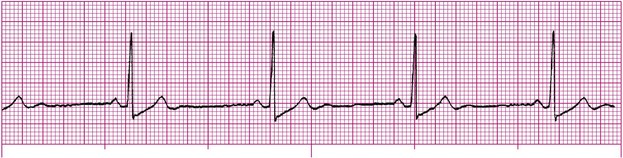
| Vital Signs/History | What are the patient’s vital signs? Coach: The patient remains unresponsive and apneic. Breath sounds are clear and equal bilaterally with bag-mask ventilation. The patient’s heart rate is 44 beats/min. Her blood pressure is 86/54 mm Hg. The patient has been placed on the cardiac monitor (Figure 7-1). What is the rhythm on the monitor? |
| The rhythm is a sinus bradycardia. Is there someone available who may know what happened to this patient? Coach: (See SAMPLE history obtained from the patient’s husband). | |
| Sample History | |
|---|---|
| Signs/symptoms | Submersion incident |
| Allergies | None |
| Medications | Unknown |
| Past medical history | Depression |
| Last oral intake | Unknown |
| Events prior | The patient was retrieved from the swimming pool by her husband. He estimates she was in the water for less than 10 minutes. |
| Airway, Breathing, Circulation | I want my most experienced assistant to intubate the patient. I want the IV team member to start an IV with normal saline. I would also like a team member to obtain a 12-lead ECG while I perform a focused physical examination. Coach: (See physical examination findings). A tracheal tube has been inserted and the cuff inflated. An IV has been established with normal saline. Describe how you will confirm placement of the tracheal tube. |
| Physical Examination Findings | |
|---|---|
| Head, ears, eyes, nose, and throat | Pink fluid initially present in mouth (cleared with suctioning) |
| Neck | Trachea midline, no jugular venous distention |
| Chest | Breath sounds clear and equal with bag-mask ventilation |
| Abdomen | No abnormalities noted |
| Pelvis | No abnormalities noted |
| Extremities | No abnormalities noted |
| Posterior body | Unremarkable |
| I will confirm placement of the tracheal tube starting with a 5-point auscultation of the chest. I will listen first over the epigastrium. What do I hear? Next, I will listen to the right and left sides of the chest in four areas. What do I hear? Coach: There are no sounds heard over the epigastrium. Breath sounds are diminished on the left side of the chest with bag-mask ventilation. They are clearly heard on the right. What would you like to do now? | |
| On the basis of these findings, I suspect a right primary bronchus intubation. I will ask the airway team member to deflate the cuff, pull back slightly on the tracheal tube, reinflate the cuff, and reassess the patient’s breath sounds. Coach: Breath sounds with bag-mask ventilation now reveal clear and equal breath sounds. What would you like to do now? | |
| Differential Diagnosis, Evaluates Interventions | If capnography confirms the presence of CO2, I will ask the airway team member to note the centimeter markings on the tracheal tube and then secure the tube in place. Coach: Waveform capnography confirms the presence of CO2. The tracheal tube has been secured. What should be done now? |
| Postresuscitation Support/Reassessment | |
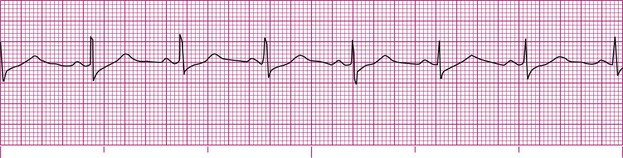
| Begins Postresuscitation Support/Performs Reassessment | I would like to repeat the primary survey and obtain another set of vital signs. Is the patient attempting to breathe spontaneously? What is the rate and quality of the patient’s pulse? What is the patient’s blood pressure? Coach: The patient is attempting to breathe spontaneously at a rate of 6 to 8/min. Her vital signs are now: Blood pressure 112/74, pulse strong and regular at 75 beats/min; ventilatory rate 10/min via bag-mask; SpO2 97% with bagging. What is the rhythm on the cardiac monitor (Figure 7-2)? What would you like to do next? |
| The monitor shows a sinus rhythm. Although the patient is beginning to breathe on her own, I want the airway team member to continue assisting her ventilations until the rate and quality of the patient’s spontaneous breathing effort improves. I will evaluate the patient’s 12-lead ECG results and transfer the patient for continued monitoring and care. | |
Case 2: Pulseless VT/VF With An Aed
Case 2: Scenario Sheet
| Emergency Action Steps | Necessary Tasks |
| Scene Survey | I am putting on personal protective equipment. Is the scene safe to enter? Coach: The scene is safe. |
| Initial Assessment | |
| General Impression | As I approach the patient and form a general impression (assessing the patient’s appearance, work of breathing, and circulation), what do I see? Coach: A woman is supine on a stretcher. Her eyes are closed. You do not see any signs of breathing. Her skin is pale and her lips are blue. What would you like to do now? |
| Primary Survey | |
| Responsiveness/Breathing | I will approach the patient and assess her level of responsiveness. Is she aware of my approach? Coach: The patient is unresponsive. How would you like to proceed? |
| I will quickly check for breathing. Coach: The patient is not breathing. How would you like to proceed? | |
| Circulation | I will feel for a carotid pulse for up to 10 seconds and assess the patient’s skin temperature, color, and moisture at the same time. Is a pulse present? Coach: There is no pulse. Her skin is cool, pale, and dry. What should be done now? |
| I will ask the CPR team member to begin chest compressions. Coach: At what rate should compressions be performed? How far should the patient’s chest be compressed? | |
| Compressions should be performed at a rate of at least 100/min. An adult’s chest should be compressed at least 2 inches (5 cm). Coach: Compressions are being performed as requested. How would you like to proceed? | |
| Airway | Although there are no visible signs of trauma, I will open the patient’s airway using a jaw thrust without head tilt because I understand that the patient was found on the floor and I cannot rule out a trauma as a result of a possible fall injury. Do I see anything in the patient’s mouth such as blood, broken teeth or loose dentures, gastric contents, or a foreign object? Coach: The patient’s airway is clear. What should be done now? |
| Breathing | I will ask the airway team member to quickly size and insert an oral airway. I will ask the airway team member and an assistant to perform two-person ventilation with a bag-mask device connected to 100% O2. I want the patient ventilated with just enough force to produce gentle chest rise. I will ask another assistant to assess the patient’s baseline breath sounds while the patient is being ventilated. Coach: An oral airway has been inserted. The patient is being ventilated with a bag-mask. You see gentle chest rise with bagging. What would you like to do next? |
| Defibrillation/Disability | I want the chest compressor and airway team member to automatically rotate positions after every five cycles (about 2 minutes) of CPR so they do not become fatigued. Without interrupting CPR, I will ask the defibrillation team member to power on the AED and then to apply the AED pads to the patient’s bare chest. Coach: The power to the AED is on. The AED pads are in place on the patient’s chest. How do you want to proceed? |
| I will ask my team to briefly interrupt chest compressions and ask the defibrillation team member to press the “Analyze” button on the AED. Coach: The AED advises a shock. | |
| As soon as the defibrillation team member indicates that he is ready to shock, I want all team members to clear the patient. I want the chest compressor to switch positions with the airway team member. As the airway team member clears the patient and assumes the compressor role, I will ask her to ensure that O2 is not flowing over the patient’s chest as we prepare to defibrillate the patient. Coach: Everyone cleared the patient and she has been defibrillated. | |
| I want my team to resume CPR immediately, beginning with chest compressions. After five cycles of CPR (about 2 minutes), the defibrillation team member will reanalyze the patient’s rhythm. Coach: The AED states, “No shock advised.” | |
| I will check for a pulse and repeat the primary survey. Is the patient responsive? Is she breathing? Does she have a pulse? Coach: A strong carotid pulse is present. The patient is waking up and breathing on her own about 12 times/min. What should be done now? | |
| Secondary Survey | |
| Vital Signs/History | I will ask an assistant to obtain a complete set of vital signs. Is there someone available who can provide additional information about this patient? Coach: The patient’s heart rate is strong and regular at a rate of 80 beats/min. Ventilations are occurring at a rate of 12/min. The patient’s blood pressure is 98/60. (See SAMPLE history obtained from neighbor and physical examination findings). What would you like to do next? |
| Sample History | |
|---|---|
| Signs/symptoms | Found unresponsive by neighbor |
| Allergies | Unknown |
| Medications | Azithromycin (Zithromax), alendronate (Fosamax) |
| Past medical history | “Intestinal problems” |
| Last oral intake | Unknown |
| Events prior | Found unresponsive on the kitchen floor by a neighbor who had last spoken to patient about 25 minutes prior |
| Physical Examination Findings | |
|---|---|
| Head, ears, eyes, nose, and throat | Cyanosis of lips |
| Neck | Trachea midline, no jugular venous distention |
| Chest | Breath sounds clear and equal with positive pressure ventilation |
| Abdomen | No abnormalities noted |
| Pelvis | No abnormalities noted |
| Extremities | No abnormalities noted |
| Posterior body | No abnormalities noted |
| Post–cardiac Arrest Support/Reassessment | |
| Begins Post–cardiac Arrest Support/Performs Reassessment | I want the airway team member to apply a pulse oximeter and capnometer to assess the patient’s oxygenation and ventilatory efforts. I will ask the airway team member to apply an oxygen delivery device (if the patient’s breathing is adequate) or continue to assist the patient’s breathing with a bag-mask device connected to O2 (if the patient’s breathing is inadequate) as indicated. I will order a cardiology consult and continue to monitor the patient’s vital signs and ECG every 5 minutes as I prepare to transfer the patient for continued care. |
Case 3: Pulseless VT/VF
Case 3: Scenario Sheet
| Emergency Action Steps | Necessary Tasks |
| Scene Survey | I am putting on personal protective equipment. Is the scene safe to enter? Coach: The scene is safe. |
| Initial Assessment | |
| General Impression | As I approach the patient and form a general impression, what do I see? Coach: The patient is supine on a stretcher. His eyes are closed. The patient does not appear to be breathing and his skin looks pale. |
| Primary Survey | |
| Responsiveness/ Breathing | I will quickly approach the patient and assess his level of responsiveness. Coach: The patient is unresponsive. |
| I will quickly check for breathing. Coach: The patient is not breathing. How would you like to proceed? | |
| Circulation | I feel for a carotid pulse for up to 10 seconds. Do I feel a carotid pulse? What is the condition of the patient’s skin? Coach: There is no pulse. The patient’s skin is cool, pale, and dry. What should be done now? |
| I will ask the CPR team member to begin chest compressions and ask for the defibrillator immediately. Without interrupting CPR, I want the defibrillation team member to attach combination pads to the patient’s bare chest. Coach: Compressions are being performed as requested. How would you like to proceed? | |
| Airway | I will open the patient’s airway using a head tilt–chin lift maneuver because I understand that the patient was assisted to the floor when he collapsed, and no head or neck trauma is suspected. Is there anything visible in the patient’s mouth such as blood, broken teeth or loose dentures, gastric contents, or a foreign object? Coach: The patient’s airway is clear. What should be done now? |
| Breathing | I will ask the airway team member to size and insert an oral airway. I want the airway team member and an assistant to begin positive pressure ventilation with a bag-mask connected to 100% O2. I want the airway team member to maintain proper head position and a good seal with the mask against the patient’s face. I want a second team member to assume responsibility for compressing the bag with just enough force to produce gentle chest rise. I will ask another assistant to assess baseline breath sounds while the patient is being ventilated. Coach: An oral airway has been inserted. Two-person bag-mask ventilation is being performed. You see gentle chest rise with bagging. Breath sounds are clear and equal with positive pressure ventilation. Combination pads are in place on the patient’s chest as requested. What should be done now? |
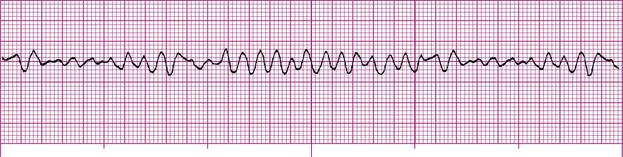
| Defibrillation/Disability | I will ask for the defibrillator immediately. I want the CPR team member and the airway team member to automatically rotate positions after every five cycles (about 2 minutes) of CPR. I want the patient’s ECG rhythm checked every 2 minutes as the team members change positions. Coach: A biphasic defibrillator is within arm’s reach. You see this rhythm on the cardiac monitor (Figure 7-3). What is the rhythm on the monitor? How do you want to proceed? |
| The rhythm is ventricular fibrillation. I will ask the airway team member to ensure that O2 is not flowing over the patient’s chest as the defibrillation team member prepares to shock the patient. I want the IV team member to prepare the initial medications that will be used and start an IV after the first shock is delivered. Coach: What initial medications do you want the IV team member to prepare? | |
| I want the IV team member to prepare epinephrine, vasopressin, and amiodarone. Coach: What energy setting will you use for your initial shock? | |
| I am using a biphasic defibrillator. The manufacturer of the machine I am using recommends 200 J for the initial shock. As the machine charges, I want all team members (with the exception of the chest compressor) to immediately clear the patient. I want the chest compressor to continue CPR while the machine is charging. When the defibrillator is charged, I want the chest compressor to immediately clear the patient. After making sure that the chest compressor is clear, I will ask the defibrillation team member to defibrillate the patient with 200 J. Coach: Shock delivered. What would you like to do next? | |
| Secondary Survey | |
| Vital Signs/History | I want my team to resume CPR immediately, beginning with chest compressions. After five cycles of CPR (about 2 minutes), I will recheck the patient’s rhythm. |
| Airway, Breathing, Circulation | Without interrupting CPR, I want the IV team member to start an IV of normal saline and then give the patient 1 mg of epinephrine using a 1 : 10,000 solution IV push. I want the medication flushed with 20 mL of normal saline and then raise the arm into which the medication was administered for about 20 seconds. Coach: An IV has been started with normal saline in the patient’s left antecubital vein. Epinephrine has been given IV as ordered. |
| Differential Diagnosis, Evaluates Interventions | I am considering possible causes of the arrest. Is there someone available who may know what happened before the patient collapsed? Coach: (See SAMPLE history obtained from the patient’s wife and coworkers and physical examination findings). |
| Sample History | |
|---|---|
| Signs/symptoms | Collapsed about 15 minutes ago |
| Allergies | Codeine, penicillin |
| Medications | Divalproex sodium (Depakote) |
| Past medical history | Epilepsy, substance abuse |
| Last oral intake | Unknown |
| Events prior | Sudden collapse |
| Physical Examination Findings | |
|---|---|
| Head, ears, eyes, nose, and throat | No abnormalities noted |
| Neck | Trachea midline, no jugular venous distention |
| Chest | Breath sounds clear and equal with positive pressure ventilation |
| Abdomen | No abnormalities noted |
| Pelvis | No abnormalities noted |
| Extremities | No abnormalities noted |
| Posterior body | No abnormalities noted |
| The cardiac monitor still shows ventricular fibrillation. While CPR continues, I want the IV team member to administer IV amiodarone. Coach: The IV team member requests clarification regarding your amiodarone order. What dosage that should be administered at this time? | |
| In cardiac arrest, the loading dose of amiodarone is 300 mg IV. I want 300 mg of amiodarone given IV at this time. Coach: Amiodarone has been given as instructed. The patient’s cardiac rhythm remains unchanged and CPR is ongoing. What would you like to do now? | |
| I will prepare to defibrillate with 300 J, as recommended by the manufacturer of the defibrillator I am using. As with the first shock delivered, I will ensure that all team members, with the exception of the chest compressor, are clear of the patient. The defibrillator is now charged and I will ask the chest compressor to clear the patient and then ask the defibrillation team member to defibrillate the patient with 300 J. Coach: The shock has been delivered. A team member calls your attention to a rhythm change on the cardiac monitor. What is the rhythm on the monitor (Figure 7-4)? | |
| The monitor shows a sinus rhythm with uniform premature ventricular complexes. Coach: What would you like to do next? | |
| Because there is an organized rhythm on the monitor, I will ask the CPR team member to stop CPR and check for a pulse.2 Coach: A strong carotid pulse is present. What should be done now? | |
| Post–cardiac Arrest Support/Reassessment | |
| Begins Post–cardiac Arrest Support/Performs Reassessment | I will ask an assistant to obtain a complete set of vital signs while I will repeat the primary survey. Is the patient responsive? Is he breathing? Coach: The patient is unresponsive but breathing shallowly at a rate of approximately 4 breaths/min. A strong pulse is present at a rate of about 80 beats/min. His blood pressure is 88/62 mm Hg. His color is improving. What should be done now? |
| I will recheck the patient’s vital signs and ECG every 5 minutes. I want a team member to apply a pulse oximeter and capnometer, obtain a 12-lead ECG, and order a cardiology consult. Until the patient’s spontaneous breathing is adequate, I want the airway team member to continue assisting the patient’s breathing with the bag-mask until arrangements can be made for mechanical ventilation. I want the IV team member to prepare an IV infusion of amiodarone while I arrange for the patient’s transfer for further care. | |
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree