To further explore the potential role of sST2 in the progression of cardiac disease, this section reviews both the associations with cross-sectional findings and longitudinal changes in cardiac structure and function measured by echocardiography and cardiac magnetic resonance imaging with sST2 levels in a variety of patient populations with or at-risk for cardiovascular disease. In a Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department substudy in patients with acute dyspnea, sST2 levels were found associated with left ventricular ejection fraction (LVEF), and both estimated right ventricular (RV) systolic pressure and RV hypokinesis. In a large cohort of ambulatory patients referred for echocardiograms, sST2 was predominantly associated with RV and not LV structural findings. In contrast, in the Framingham Heart Study, a community cohort of >3,300 participants, sST2 was not associated with either echocardiographic finding, although in the Cardiovascular Health Study, sST2 appeared strongly associated with the presence of diastolic dysfunction. Little evidence exists on the relation of sST2 levels with longitudinal change in cardiac structure and function. A substudy of Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) evaluated the association among LV remodeling (defined as an increase in LV end-systolic and -diastolic volumes), sST2, and the benefit of eplerenone and found that sST2 levels were good surrogates of left ventricular remodeling. In the same line, the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) study found that more time spent with an sST2 level less than the cutoff of 35 ng/L identified patients with a greater probability of a decrease in LV diastolic index over 1 year.
sST2 as described throughout this monograph is a powerful independent predictor of mortality in patients with acute dyspnea, acute decompensated heart failure (HF), chronic HF, acute coronary syndromes, and general community-based populations. The interleukin-33/ST2 receptor interaction has been shown to result in mitigation of the development of left ventricular hypertrophy (LVH) in animal models. In experimental cell culture and animal models, sST2 is released by myocyte cell stress, whereas others have shown with in vivo human data, and cellular data, that sST2 production is predominantly from endothelial cells and is not specific to the heart. A study validating the highly sensitive Presage commercial sST2 assay showed that sST2 levels could be elevated in both HF and noncardiac conditions, such as pulmonary disease and sepsis. Therefore, given a potential direct role for sST2 production from the myocardium under stress, a palliative role of the interleukin-33/ST2 interaction on the development of LVH, and the significant noncardiac production of sST2, understanding the association of sST2 levels with cardiac structure and function can provide insight into how to best use this test for prognosis and potentially guiding therapy in cardiovascular disease. This chapter is divided into 4 sections. The first 3 will evaluate the cross-sectional association of echocardiographic measures and sST2 levels in patients with acute dyspnea, in outpatients referred for echocardiography, and in community-dwelling cohorts from the general population. When available, associations with structural heart disease and subsequent prognosis will also be contrasted with B-type natriuretic peptide (BNP) or the amino terminal fragment of proBNP (NT-proBNP). Lastly, the association of sST2 levels and subsequent change in left ventricular structure and function with longitudinal imaging studies will be evaluated, and the implications for guiding therapy will be considered.
Echocardiographic Association With sST2 in Symptomatic Populations
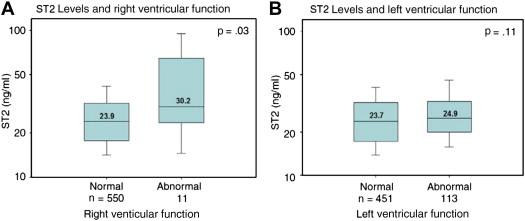
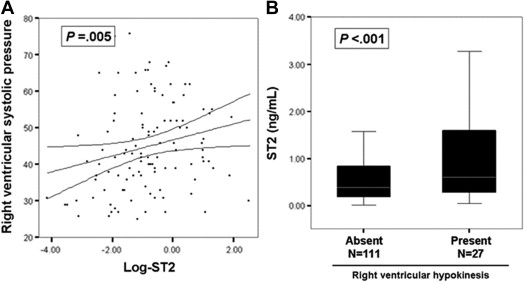
The Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department study first evaluated sST2 levels in patients with possible acute decompensated HF. In addition to showing sST2 was a powerful predictor of all-cause mortality independent of the cause of dyspnea, clinical risk factors, and NT-proBNP levels, a subset of 139 subjects were evaluated by echocardiography during their hospitalization. There was a significant association of sST2 levels with left ventricular ejection fraction (LVEF) and strong associations with both estimated right ventricular (RV) systolic pressure and RV hypokinesis ( Figure 1 ). In a multivariate analysis, sST2 remained independently associated with LVEF, LV dimensions, and transmitral E to tissue Doppler Ea ratio (a surrogate of left atrial pressure). Interestingly, RV systolic pressure also remained an independent predictor of sST2 level providing insight into the long-term prognostic association of sST2 in this acute dyspnea cohort irrespective of whether the symptoms were attributed to a cardiac or a pulmonary cause ( Table 1 ). In a subsequent study of patients with acute dyspnea in the emergency department, echocardiography was done per research protocol and ultimately available in 316 subjects (81% of the sST2 cohort) with technically feasible studies for a quantitative LVEF in 290. Echocardiographic indexes were evaluated in all patients and those with a preserved LVEF (≥50%, n = 200), and both sST2 and NT-proBNP levels were measured. Associations with LV structure and function were stronger for NT-proBNP than sST2. For subjects with a preserved LVEF, only the transmitral E to tissue Doppler Ea ratio remained significant for sST2 ( Table 2 ). Measures of RV function were not reported. Despite the stronger associations of NT-proBNP with echocardiographic structural and functional measures, in a multivariate analysis of 1-year all-cause mortality, sST2, but not NT-proBNP, remained a significant predictor of death. The findings from both these studies were of only moderate correlations with echocardiographic indexes, but an overall superior prognostic performance of sST2 compared with NT-proBNP speaks to the likely importance of sST2 levels being modulated through both cardiac and noncardiac sources.
| Covariate | T | P |
|---|---|---|
| Log-transformed NT-proBNP | 3.31 | 0.009 |
| RV systolic pressure | 2.29 | 0.002 |
| Transmitral E to tissue Doppler Ea ratio | –2.13 | 0.03 |
| Tissue Doppler A wave peak velocity | 2.11 | 0.05 |
| LV ejection fraction | –2.15 | 0.05 |
| LV end-diastolic dimension | 2.98 | 0.005 |
| LV end-systolic dimension | 2.57 | 0.01 |
| Heart rate | 2.59 | 0.01 |
| Jugular venous distension | 2.00 | 0.05 |
| All patients | LVEF ≥ 50% | |||||||
|---|---|---|---|---|---|---|---|---|
| sST2 | NT-proBNP | sST2 | NT-proBNP | |||||
| Spearman correlation | P | Spearman correlation | P | Spearman correlation | P | Spearman correlation | P | |
| LVEF | −0.21 | <0.001 | −0.55 | <0.001 | ||||
| LVEDV | 0.08 | 0.19 | 0.43 | <0.001 | ||||
| LVESV | 0.14 | 0.02 | 0.53 | <0.001 | ||||
| LV mass index | 0.26 | <0.001 | 0.68 | <0.001 | 0.12 | 0.09 | 0.47 | <0.001 |
| Pk E velocity † | 0.13 | 0.23 | 0.25 | <0.001 | 0.10 | 0.17 | 0.16 | 0.03 |
| Pk A velocity | −0.16 | 0.007 | −0.26 | <0.001 | 0.04 | 0.56 | 0.10 | 0.2 |
| Dec time | −0.24 | <0.001 | −0.24 | <0.001 | 0.02 | 0.84 | 0.20 | 0.007 |
| Em | −0.26 | <0.001 | −0.52 | <0.001 | −0.13 | 0.1 | −0.42 | <0.001 |
| Am | −0.23 | 0.001 | −0.46 | <0.001 | −0.04 | 0.6 | −0.22 | 0.007 |
| E/Em | 0.33 | <0.001 | 0.59 | <0.001 | 0.21 | 0.01 | 0.44 | <0.001 |
∗ Patients with echocardiography completed (n = 290). Nonparametric (Spearman) correlations are presented.
† Pk E velocity, peak early diastolic mitral inflow velocity; Pk A velocity, peak late diastolic mitral inflow velocity; Dec time, deceleration time of the early diastolic mitral inflow velocity; Am, tissue Doppler-derived myocardial late diastolic peak velocity.
sST2 Level and Association With Echocardiographic Findings in Ambulatory Patients Referred for Echocardiography
At the San Diego Veterans Affairs Medical Center, Daniels et al evaluated 588 ambulatory patients referred for echocardiograms by measuring both sST2 and BNP levels. In addition, these patients were followed for 1-year for all-cause mortality. The indications for study were diverse and included suspected HF (20%), history of risk factors or pre-operative examination (16%), murmur (15%), dysrhythmia or abnormal ECG (12%), and suspected valvular abnormality (10%). Overall, this was a distinctly different population than the ones previously described earlier. sST2 was predominantly associated with RV and not LV structural findings ( Figure 2 and Table 3 ). Although both sST2 and BNP were univariate predictors of 1-year mortality, only sST2 remained predictive in the multivariate analysis (hazard ratio [HR] 17.11 per log sST2, p <0.001). A history of HF remained as the only other multivariate predictor of death, but the HR was more modest (HR 2.69, p = 0.01). These findings again suggest that noncardiac pathology is in part driving sST2 levels and subsequently influences prognosis.