11 Stress Testing for Structural Heart Disease
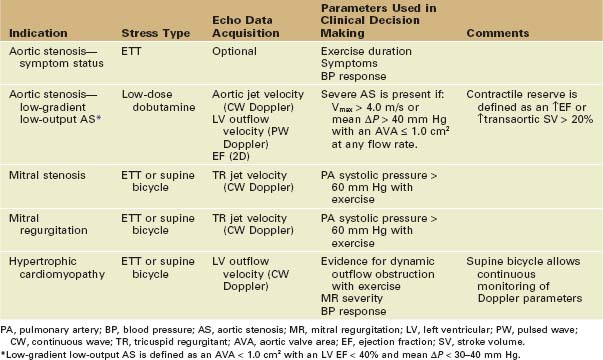
Basic Principles
• The physiologic effects of structural heart lesions may not be evident at rest (Table 11-1).
• Flow across a stenotic valve that is adequate at rest may fail to increase appropriately with exercise or pharmacologic stress.
• Intracardiac pressures that are normal at rest may increase significantly as cardiac output increases, with either stenotic or regurgitant valve lesions.
• Changes in ventricular geometry with stress may result in altered valve dynamics with an increase in regurgitant severity.
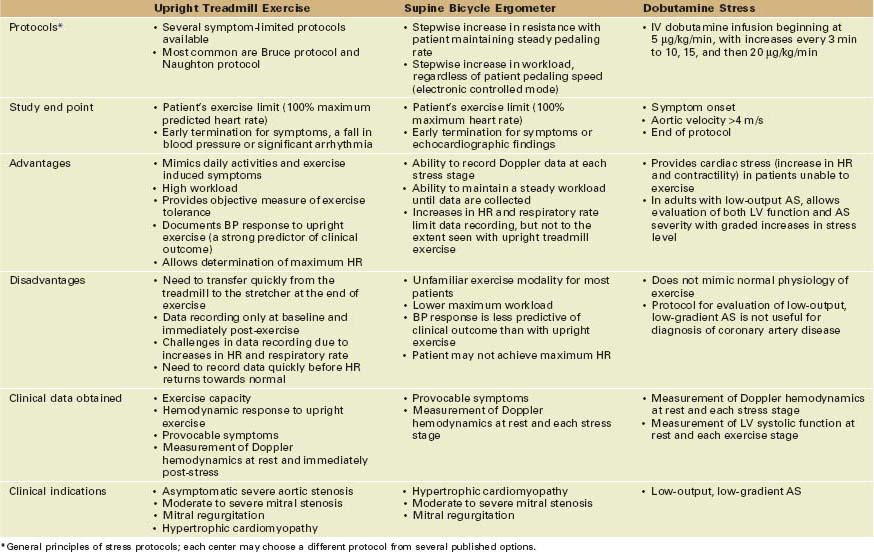
• Exercise is the most physiologic type of stress test as it mimics normal physical activity (Table 11-2).
• The typical hemodynamic target for an exercise stress test is 85% of the age-adjusted maximum predicted heart rate (HR) (about 220 minus patient age).
• Systolic blood pressure (BP) normally increases by at least 20 mm Hg with exercise; a blunted BP rise suggests significant cardiovascular limitation.
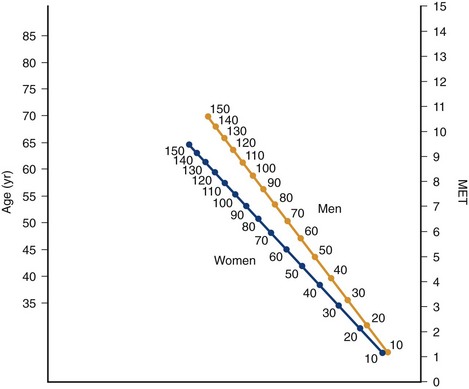
• With standard treadmill exercise protocols, exercise duration provides an estimate of functional aerobic impairment (FAI) using a nomogram based on age, gender, and degree of physical conditioning (Fig. 11-1).
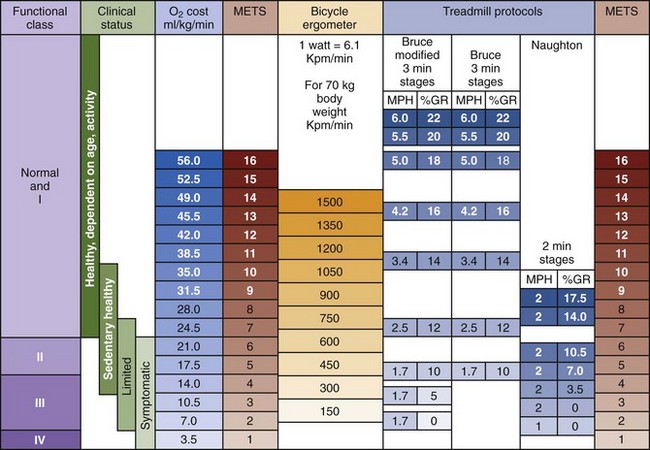
• Metabolic equivalents (METs) are a measure of oxygen (O2) consumption, where 1 MET equals 3.5 mL O2 per kg/min, equivalent to the resting metabolic state, 3 to 6 METs is equivalent to moderate exercise, and greater than 6 METs corresponds to strenuous exercise.
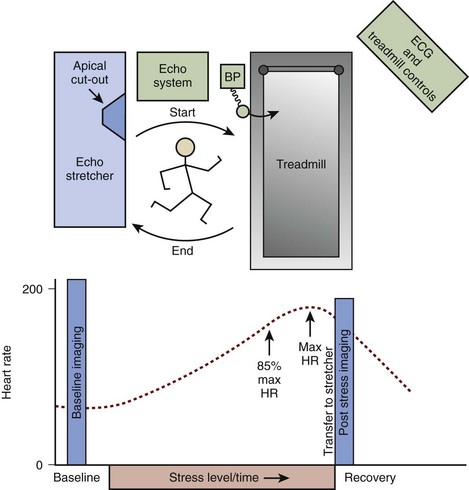
• With treadmill exercise, echocardiographic data are recorded at baseline and immediately following exercise, after the patient transfers back to the stretcher (Fig. 11-2).
• With a supine bicycle ergometer, an incremental increase in workload is achieved either by maintaining a constant pedaling speed (mechanically braked bicycles) or by maintaining a desired workload regardless of pedaling rate (electronically braked ergometers).
• Supine bicycle exercise allows continuous recording of echocardiographic data, although the maximum workload may be lower than with upright treadmill exercise.
• Pharmacologic stress testing is useful in patients who cannot exercise and for specific clinical indications.
• A pharmacologic agent, most often intravenous dobutamine, can be used as a cardiac stressor, based on the induced increase in HR and left ventricular (LV) contractility.
• Continuous electrocardiographic (ECG) monitoring is needed during all stress testing.
• Continuous ECG monitoring is a standard safety measure for detection of cardiac arrhythmias during stress testing.
• The ECG usually is not accurate for detection of coronary disease in patients undergoing stress testing for structural heart disease because:
• Exercise stress testing is safe in adults with structural heart disease with appropriate patient selection and careful clinical monitoring (Box 11-1).
• Overall risk is similar to stress testing for coronary disease with very low risk for death or myocardial infarction.
• Risk is related to the severity of the underlying structural heart disease, with a higher risk for syncope when severe aortic stenosis (AS) is present; stress testing is contraindicated when symptoms are present in AS patients.
• Other major complications include arrhythmias and hypotension; the stress test should be stopped immediately if BP fails to increase appropriately or at the onset of an arrhythmia.
• Careful monitoring is needed for stress testing in adults with structural heart disease (Box 11-2).
Box 11-1
Risks of Stress Testing in Adults with Structural Heart Disease
Risk for major complications is reported for populations primarily including patients with coronary artery disease (CAD). Large databases on adults with structural heart disease are not available. Risk may be higher in patients with more severe structural heart disease, particularly for exercise or dobutamine stress testing in patients with severe AS or HCM.
Box 11-2 Recommended Set-up and Monitoring for Stress Testing in Adults with Structural Heart Disease
Asymptomatic Severe Aortic Stenosis
Indications
• Symptom onset is a definite indication for aortic valve replacement in adults with severe AS.
• A clinical history often is adequate to elicit the onset of decreased exercise tolerance or subtle symptoms of exertional dyspnea, chest discomfort, or dizziness.
• Doppler data are not routinely recorded with exercise testing for evaluation of AS symptom status but may be helpful in selected cases.
Step-by-step Approach
Test Preparation
• Review the clinical history and ask the patient directly about possible symptoms; if symptoms are present, stress testing should not be performed.
• Record the baseline ECG, determine cardiac rhythm, and compare with previous ECGs to ensure there are no acute changes.
• Instruct the patient about the stress test protocol, including:
• Transfer rapidly to the echo stretcher immediately after treadmill exercise if Doppler data will be recorded.
• Obtain informed consent for the exercise stress test.
• The primary risk of stress testing in adults with severe AS is provocation of symptoms, including angina or syncope.
• Reported adverse events with stress testing in adults with asymptomatic AS include:
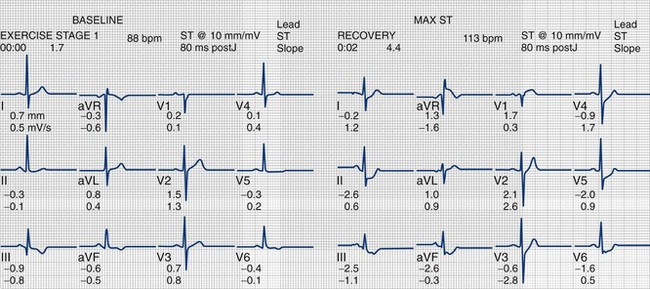
• Horizontal ST depression >2 mm in up to 80% of patients, which is not predictive of coronary artery disease.
• Provoked symptoms of angina, dizziness, or dyspnea in up to one third of patients. The test should be stopped promptly at symptom onset.
Review the Baseline Echocardiogram
• A complete resting quantitative echo-Doppler study is needed before stress testing in adults with AS.
Exercise Stress Test
• A standard symptom-limited treadmill or supine bicycle stress test protocol is preferred for evaluation of exercise duration and the BP response to upright exercise.
• With the upright treadmill Bruce protocol, treadmill speed and incline are increased every 3 minutes until the study end point is achieved (Fig. 11-3).
• In some cases, supine bicycle exercise may be reasonable if the goal is to measure Doppler hemodynamics at rest and with exercise.
• Exercise is stopped for:
• Any significant arrhythmia, including sustained ventricular tachycardia (absolute indication) and multifocal premature ventricular beats, new-onset atrial fibrillation, supraventricular tachycardia, heart block, or bradyarrhythmias (relative indications).
Interpretation of Stress Test
• Adults with severe AS who have abnormal symptoms with exercise testing are then classified as having severe symptomatic AS and should be referred for consideration of valve replacement.
• Exercise duration, compared with normal standards for age and gender, is a strong predictor of clinical outcome; limited exercise tolerance suggests hemodynamically significant AS.
• In the absence of symptoms, achieving an HR at least 85% of the predicted maximum indicates that an adequate workload was achieved; a lower maximum HR suggests inadequate effort or the effects of beta-blocker therapy.
• A blunted BP response to exercise (failure to increase by at least 10 mm Hg) is consistent with flow limiting severe AS, and valve replacement should be considered.
Doppler Echocardiographic Data
• Doppler data are not routinely recorded with exercise testing for evaluation of AS symptom status but may be helpful in selected cases.
• Aortic valve velocity and gradient increase with exercise due to the increase in transaortic flow rate.
• When stenosis is not severe, the valve leaflets are still somewhat flexible so that orifice area increases slightly (by about 0.2 cm2) with the increase in flow rate.
• When the valve leaflets are rigid so that leaflet opening does not increase with exercise, there is a greater increase in transaortic velocity and gradient compared with a flexible valve.
• Recording accurate Doppler data with stress testing for AS is challenging.
• Velocity data post-exercise must be recorded as quickly as possible, before HR and flow rate decline significantly.
• Echocardiographic windows post-exercise may differ from the rest windows due to changes in cardiac size and position with exercise.
• Immediately post-exercise, LV outflow velocity and aortic jet velocity are again recorded.
• Aortic jet velocity often is recorded from the apical window in order to record the data as quickly after exercise as possible; if the highest jet is from a different window, this needs to be taken into account.
Potential Pitfalls
• Stress testing in adults with severe AS is contraindicated when symptoms are present; there is a high risk for sudden death with stress testing in this situation.
• Exercise duration may be limited by comorbid conditions, such as pulmonary or systemic diseases, rather than by severe AS.
• BP may be difficult to measure with exercise in AS patients; if the BP cannot be measured, the test should be promptly stopped because hypotension may be present.
Alternate Approaches
• Stress testing is not needed in all patients with severe AS; if an accurate clinical history is obtained, watchful waiting and patient education about early symptoms is appropriate.
• Serum brain natriuretic peptide levels are higher in adults with symptomatic AS than in those who are asymptomatic and may be helpful in evaluation of equivocal symptoms.
• Direct imaging of valve anatomy with transesophageal echocardiography, cardiac computed tomographic (CT) imaging, or with cardiac magnetic resonance (CMR) imaging also may be helpful in clinical decision making.
Low-output, Low-gradient Aortic Stenosis
Indications
• Low-output, low-gradient AS is defined as a mean transaortic pressure gradient of less than 30 mm Hg and an aortic velocity of less than 3.5 m/s with an AVA of less than 1.0 cm2.
• LV systolic function typically is moderately to severely reduced, with an ejection fraction (EF) of less than 50%.
• Some patients with low-gradient, low-output AS have severe valve obstruction with LV dysfunction due to the high afterload imposed by the stenotic valve.
• Dobutamine stress echocardiography (DSE) is helpful for distinguishing severe AS with afterload mismatch from primary LV dysfunction with moderate AS in the setting of a reduced LV EF.
Step-by-step Approach
Test Preparation
• Review the clinical history with attention to any potential contraindications to dobutamine infusion (e.g., significant arrhythmias, allergy history, uncontrolled hypertension).
Baseline Echocardiogram
• The most recent complete transthoracic study is reviewed to determine the optimal windows for data recording and to ensure that the baseline stress test data are recorded correctly.
Stress Protocol
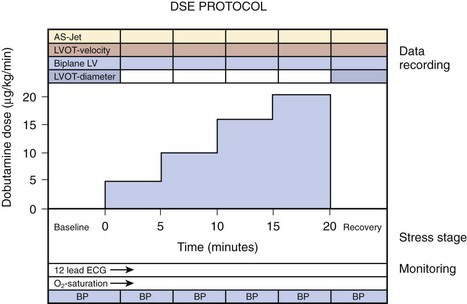
• After baseline Doppler echo data and monitoring data are recorded, dobutamine infusion is started, typically at 5 µg/kg/min (Fig. 11-5).
• Careful patient monitoring is needed to ensure patient safety, which is critically important given the presence of LV dysfunction and aortic valve obstruction in these patients.
• The ECG is continuously monitored during the test, with periodic (usually every 3 minutes) 12-lead ECG recording.
• BP is measured periodically, at least every 3 minutes, with an increased frequency of monitoring as dictated by the clinical situation.
• The dobutamine infusion is increased every 3 to 5 minutes by 5 µg/kg/min to a maximum dose of 20 µg/kg/min (e.g., stress stages at 5, 10, 15, and 20 µg/kg/min).
• Dobutamine starting and maximum doses are lower compared with stress testing for coronary disease.
• The stress test end point is not determined by HR because there usually is only a modest increase from baseline.