Stress Testing for Ischemia and Viability
Daniel H. Cooper
Thomas K. Kurian
Key Points
Echocardiographic stress testing is a sensitive and specific modality for detecting the presence of stress-induced ischemia in appropriately selected patients.
Ischemia manifests as regional wall motion abnormalities and changes in myocardial thickening during stress.
Exercise echocardiography yields additional prognostic information and is preferred to pharmacologic stress testing.
Causes of false negative results include: Failure to reach target heart rate, delayed peak stress image acquisition, single-vessel disease especially involving the circumflex artery, anti-anginal/beta-blocker use before testing.
Causes of false positive results include: HTN, LVH, coronary spasm, paradoxical septal motion secondary to conduction abnormality (LBBB, pacing).
To avoid these pitfalls, recognize the importance of achieving an adequate level of stress (>85% MPHR), timely image acquisition (<60 s for exercise echo protocols), and confirming wall motion abnormalities in multiple views.
Dobutamine stress echocardiography can be utilized to confirm myocardial viability by noting the presence of a biphasic response to increasing rates of dobutamine infusion.
General Principles
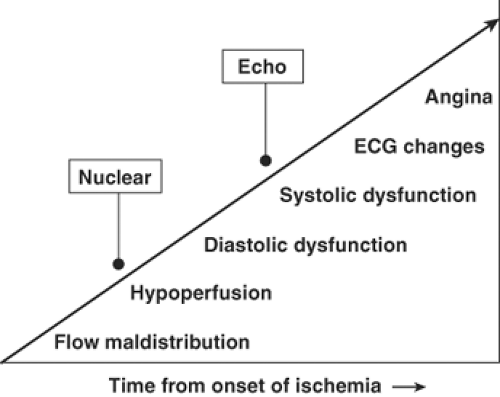
The use of stress echocardiography for detection of ischemia is based on the principles outlined by the ischemic cascade (see Fig. 6-1).
Impaired myocardial perfusion due to coronary artery disease (CAD) leads to a progression of manifestations during exercise or pharmacologic stress that ultimately results in regional or global wall motion or thickening abnormalities.
The goal is to determine whether ischemia is present or, if there are baseline wall motion abnormalities and reduced LVEF, if there is viable myocardium and LV contractile reserve.
Obtaining an adequate level of stress is vital to maintaining the modality’s sensitivity for detecting CAD.
Achieving 85% of the maximally predicted heart rate (MPHR = 220 – Age) improves sensitivity greatly.
However, if changes consistent with ischemia are detected at lower (submaximal) levels of stress, this improves specificity of the result.
Continuous patient monitoring by medical staff is required, including frequent symptom inquires, continuous ECG, and intermittent BP measurement.
Crash carts, stocked with resuscitation equipment and medications, should be available.
Risk of MI/Death ∼1/2500
Anatomy
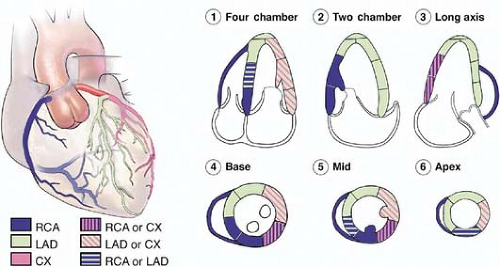
Stress echocardiography typically focuses on images obtained in the apical (four- and two-chamber) and parasternal (short- and long-axis) views, allowing for observation of all myocardial segments.
Knowledge of the typical distribution of coronary artery blood flow to the various myocardial segments is vital. It allows:
Confirmation in multiple views of suspected lesions, especially when image quality in one view is suboptimal.
Correlation of findings to specific location(s) of coronary artery stenosis (Fig. 6-2).
LAD: Anterior, anteroseptal, apex, +/- inferoapical (wrap-around LAD)
Circumflex: Anterolateral, inferolateral
RCA: Inferior, inferoseptal (basal, mid), +/- inferolateral (depending on dominance)
Distal versus proximal: A proximal LAD lesion; for example, will result in basal to distal wall motion abnormalities of the anteroseptum (septal perforators) and anterior wall (diagonal) whereas distal LAD disease will affect only the apex.
Exercise Stress Echocardiography
In general, all exercise stress protocols involve staged increases in workload to increase myocardial oxygen demand. This is accomplished by treadmill or stationary bicycle exercise.
The Bruce protocol (most common) involves symptom-limited exercise on the treadmill where grade and speed increases every 3 minutes.
METS (metabolic equivalents) are calculated automatically by the machine and is important to report as a prognostic indicator (<5 METS suggests poor prognosis if <65 years old).
Absolute Contraindications
Acute MI
High-risk unstable angina
Uncontrolled ventricular (VT) or supraventicular tachycardia (SVT)
Severe arterial hypertension; systolic blood pressure (SBP) >200 mmHg and/or diastolic blood pressure (DBP) >110 mmHg
Symptomatic severe aortic stenosis
Uncontrolled, symptomatic congestive heart failure (CHF)
Acute PE or pulmonary infarct
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree