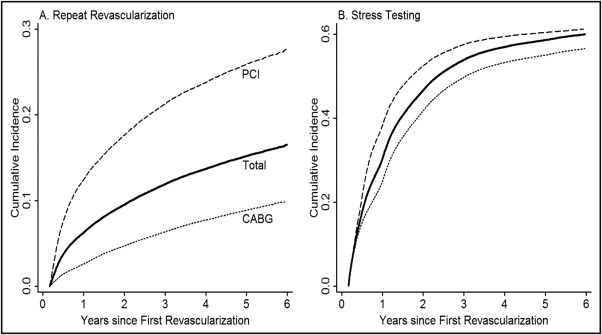
The optimal use of stress testing after coronary revascularization remains unclear, and overuse of stress testing might increase the rates of repeat revascularization. We analyzed the association at both the patient and regional level between the use of stress testing and repeat revascularization for a cohort of Medicare beneficiaries receiving revascularization within 30 days of an admission for symptomatic coronary artery disease. The sample consisted of 219,748 Medicare beneficiaries aged >65 years who received percutaneous coronary intervention or cardiac bypass artery grafting after hospital admission for symptomatic coronary artery disease in 2003 to 2004. Medicare claims data through 2008 identified the use of stress testing and repeat revascularization. The associations between the cumulative incidence of stress testing and repeat revascularization were analyzed using linear regression analysis. Within 6 years of the initial revascularization, the cumulative incidence of events was 0.61 for stress testing and 0.23 for repeat revascularization. Most (53.1%) repeat revascularizations were preceded by a stress test. Only 10.3% of repeat revascularization procedures were preceded by myocardial infarction. The 4-year cumulative incidence of repeat revascularization and stress testing varied between the Hospital Referral Regions represented by the sample, and the positive correlation between the rates by the health referral region accounted for only a small portion of the total health referral region variation in revascularization rates. In conclusion, stress testing is commonly performed among Medicare patients after the initial revascularization, and most repeat procedures are performed for stable coronary artery disease. The variation in stress testing patterns only explained a modest fraction of the regional variation in the repeat revascularization rates.
Although routine stress testing for patients with asymptomatic coronary artery disease (CAD) has been advocated for patients after percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), current appropriateness criteria suggest that stress testing within 5 years of CABG or 2 years of PCI is not appropriate for asymptomatic patients. In addition, the current guidelines suggest that coronary revascularization should not be undertaken in asymptomatic patients unless evidence of high-risk ischemia is present by noninvasive imaging. Despite these guidelines, geographic variation in the use of stress testing by physicians might be associated with greater rates of repeat revascularization given the potentially discretionary nature of both decisions. To evaluate the contribution of regional variation in stress imaging use to the incidence of repeat revascularization, we conducted a retrospective cohort review of Medicare enrollees who underwent multivessel revascularization after admission for acute coronary syndrome.
Methods
The 2003 and 2004 Medicare Provider Analysis and Review (MedPAR) records were used to identify all fee-for-service Medicare beneficiaries aged ≥66 years admitted for symptomatic CAD from January 1, 2003 to October 14, 2004, defined by the presence of International Classification of Diseases, 9th edition, Clinical Modification diagnosis codes 410.xx, 411.1, and 413.9. Each patient’s first CAD-related hospitalization during 2003 and 2004 was considered their index admission. For the identified patients, we obtained all MedPAR, Carrier, and Outpatient Medicare claims and Medicare Denominator files for 2002 through 2008; thus, ≤6 years of follow-up were available. Using the claims from the 12 months preceding the index admission and the index admission itself, the patients were excluded if they had a history of CAD-related admission, cardiac surgery, or PCI.
The MedPAR and Carrier records were used to determine whether each identified patient had undergone coronary revascularization during the 30 days after their index admission date using the “International Classification of Diseases, 9th edition, Clinical Modification” procedure codes, Healthcare Common Procedure Coding System codes, and Diagnosis-Related Groups (PCI, 36.01 to 36.07, 92980 to 92981, 92984, 92995 to 92996, G0290 to G0291, 516 to 518, 526 to 527, 555 to 558; CABG, 36.10 to 36.19, 33510 to 33523, 33530 to 33536, 106 to 107, 109, and 547 to 550). The patients were included if their initial coronary revascularization procedure was multivessel PCI or CABG. We also identified and included patients who had undergone a staged PCI procedure by adding those patients who received a second PCI procedure within 30 days of their first but for which the second PCI claim did not include an acute coronary syndrome-specific diagnosis code.
The Carrier, Outpatient, and MedPAR records were next used to identify the use of stress testing after revascularization using the Healthcare Common Procedure Coding System and International Classification of Diseases, 9th edition, Clinical Modification codes (stress testing with electrocardiography: 93015 to 93018, 89.41 to 89.43; nuclear testing: 78460 to 78461, 78464 to 78466, 78468 to 78469, 78472 to 78473, 78481, 78483, 78491 to 78492, 78494, 89.44; and echocardiography: 93350). Electrocardiographic stress testing and nuclear stress testing claims occurring within 3 days of each other were considered a single, nuclear stress test; electrocardiographic stress testing and stress echocardiography testing occurring within 24 hours of each other were considered a single, echocardiographic stress test. Because stress testing immediately after revascularization can be done to assess the appropriateness for cardiac rehabilitation or to measure the response to revascularization, the stress tests were only included if they occurred >60 days from the date of the patient’s first revascularization. The patients were included in the analyses if they survived 60 days after their initial revascularization procedure without repeat revascularization (with the exception of staged PCI previously described) or readmission for myocardial infarction.
The interval to stress testing and the interval to repeat revascularization within 6 years of the initial revascularization were calculated using cumulative incidence techniques. Unadjusted cumulative incidence rates of repeat revascularization were examined both across the entire cohort and stratified by the initial revascularization modality (CABG or PCI), with comparisons of cumulative incidence made using a nonparametric test of equality. Finally, the patients were assigned to their Health Referral Region (HRR) from the Dartmouth Atlas according to the zip code on their index admission MedPAR record. Using observations aggregated at the HRR level, the correlation between the HRR level cumulative incidence of repeat revascularization and stress testing was assessed using simple linear regression models weighted according to the number of cohort members in the HRR. The correlation between HRR level incidence of stress testing and the proportion of patients receiving a stress test who underwent repeat revascularization within 60 days of their stress test (the “test yield”) was also compared using weighted linear regression analysis.
Inferential statistics were considered significant at a 2-sided α-level of 0.05. All calculations were conducted in Stata/MP, version 12.0 (StataCorp, College Station, Texas), except for competing risk calculations, which were performed using R, version 2.12.1 (R Foundation, Vienna, Austria) using the cmprsk package. The University of North Carolina Public Health-Nursing institutional review board reviewed and approved the study protocol and waived informed consent.
Results
A total of 86,132 patients met the inclusion criteria, of whom 54,124 were treated initially with CABG and 32,008 with PCI. The patients were followed up for a mean of 1,639 days after revascularization (standard deviation 508 days). The baseline characteristics are listed in Table 1 .
| Variable | All (n = 86,132) | PCI (n = 32,008) | CABG (n = 54,124) | p Value |
|---|---|---|---|---|
| Mean age (years) | 75.0 | 75.8 | 74.5 | <0.001 |
| Men | 60.3% | 53.6% | 64.2% | <0.001 |
| Diabetes mellitus | 25.7% | 24.9% | 26.3% | <0.001 |
| Hypertension, with complications | 50.3% | 52.1% | 49.3% | <0.001 |
| Heart failure | 6.4% | 8.4% | 5.3% | <0.001 |
| Previous stroke | 7.2% | 6.9% | 7.4% | 0.03 |
| Chronic kidney disease/renal failure | 1.6% | 1.8% | 1.5% | 0.002 |
| Chronic obstructive pulmonary disease | 10.2% | 12.2% | 9.0% | <0.001 |
| ST-segment elevation myocardial infarction at presentation | 19.0% | 21.9% | 17.2% | <0.001 |
The cumulative incidence of having ≥1 repeat coronary revascularization procedure >60 days after the initial acute coronary syndrome-related revascularization was 0.17. The cumulative incidence of repeat revascularization was greater (0.28) among the PCI patients at 6 years of follow-up compared to 0.10 among the CABG patients (p <0.001; Figure 1 ). The coded indications for repeat revascularization were similar, regardless of the patient’s initial revascularization modality ( Table 2 ).
| Diagnosis (“International Classification of Diseases, 9th edition, Clinical Modification” codes) | All (n = 13,292) | PCI (n = 8,360) | CABG (n = 4,932) | p Value |
|---|---|---|---|---|
| Angina (411.1, 413.x) | 37.7% | 38.1% | 37.0% | 0.19 |
| Other chest pain (786.50, 786.51, 786.59) | 10.5% | 10.6% | 10.4% | 0.69 |
| Acute myocardial infarction (410. x1) | 10.3% | 10.6% | 9.8% | 0.15 |
| Preceded by stress test within 60 days of revascularization | 43.2% | 41.1% | 46.7% | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


