Stress Echocardiography
Stress echocardiography (SE) is one of the main diagnostic modalities used in the evaluation of patients with known or suspected coronary artery disease (CAD). Stress echo permits an integral evaluation of global and regional ventricular function, valvular integrity, and, most important, myocardial response to stress. The Class I indications for SE in chronic ischemic heart disease are diagnosis of ischemia in symptomatic individuals and the assessment of myocardial viability (hibernating myocardium) for planned revascularization (dobutamine echo). In addition, the referral base to the test is being augmented by situations when the effects of increasing cardiac reserve are sought in patients with valvular heart disease, diastolic dysfunction, pulmonary hypertension, and hypertrophic cardiomyopathy.
The accuracy of SE is superior to stress electrocardiography (ECG) and comparable to that of nuclear stress testing. In general, SE is less sensitive for single vessel CAD but more specific than perfusion imaging.
Numerous studies have validated the prognostic significance of SE, with a negative test carrying a very low risk (<1%) of major cardiac events over the subsequent 4 to 5 years. SE can also distinguish viable from scarred myocardium. The ability to predict which patients with left ventricular (LV) dysfunction will benefit from modern revascularization techniques is an important piece of information that may facilitate the discussion of benefit and risk for intervention that may carry significant risk. Although the accuracy and prognostic implications of dobutamine stress echocardiography (DSE) in the detection of viability are comparable to the more contemporary modalities of positron emission tomography (PET) imaging and magnetic resonance imaging (MRI), the role of dobutamine-induced augmentation in predicting functional recovery has been challenged by the recent results of the STICH trial. Within the realm of valvular heart disease, SE has an increasing role in predicting the functional significance of a variety of valvular lesions. Compared to other noninvasive modalities, SE is safe, widely available, relatively inexpensive, and avoids radiation exposure. However, its interpretation remains subjective and requires a considerable learning curve with substantial interobserver variability. Much effort has been devoted toward quantitation—for example using strain—but this remains challenging.
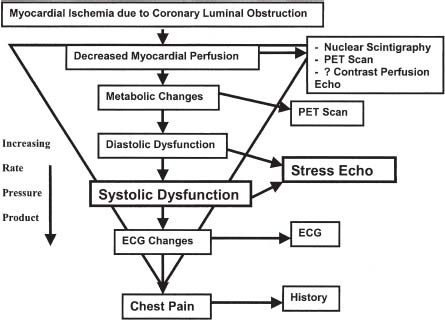
SE detects ischemia earlier in the ischemic cascade than ECG and before symptoms appear by identifying new regional wall motion abnormalities (RWMA) (Fig. 11.1). SE adds to exercise ECG particularly when the baseline ECG limits ST-segment assessment such as in left bundle branch block (LBBB), intraventricular conduction delay, paced rhythms, left ventricular hypertrophy (LVH), and digitalis effect.
FIGURE 11.1 Ischemic cascade. (From Daly RP. Stress Echocardiography. In: Griffin BP, Topol EJ, eds. Manual of Cardiovascular Medicine, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2009:633, with permission from Wolters Kluwer Health.)
FORMS OF STRESS
Exercise Echocardiography
The most physiologic form of stress testing remains exercise. In addition to the echocardiographic data, exercise provides important physiologic information for prognosis and risk stratification. Exercise echo can be done using a treadmill or bicycle. The advantage of bicycle exercise is that imaging can be performed during stress. For treadmill exercise, patients must be taken off the treadmill and the echo images acquired within 1 minute of peak exercise. However, bicycle exercise is more effort dependent and therefore less reliable in reaching a target heart rate. Exercise is also preferred for noncoronary indications such as valvular heart disease or hypertrophic cardiomyopathy.
Pharmacologic Stress Echocardiography
Approximately 30% of patients are unable to exercise for reasons such as peripheral vascular disease, obstructive lung disease, or musculoskeletal problems. For these patients, pharmacologic SE can be performed. There are three options for pharmacologic SE: (a) sympathomimetic agents such as dobutamine, (b) vasodilator agents such as adenosine, and (c) atrial pacing.
Of the sympathomimetic agents, dobutamine has the largest clinical experience. It produces stress through an increase in myocardial oxygen demand via its positive inotropic and chronotropic effects. At low doses, it has positive inotropic effects mediated through cardiac α and β1 receptors. At high doses it possesses chronotropic effects through the β2 receptor. Dobutamine can be combined with atropine to achieve a target heart rate of 85% of age-predicted maximum heart rate. Contraindications to atropine use include angle-closure glaucoma and severe benign prostatic hypertrophy. In patients who are morbidly obese without other viable noninvasive options for risk stratification, dobutamine has been combined with transesophageal echo to avoid the potential morbidity of cardiac catheterization. When assessing viability, dobutamine is preferred for assessment of contractile reserve at low doses.
Vasodilators, such as adenosine or dipyridamole, induce ischemia via a coronary steal effect that preferentially shunts blood away from myocardial segments supplied by stenotic coronary arteries. Adenosine has a short half-life, and both have fewer side effects than dobutamine. However, the intensity of ischemia is also less, so the echo findings are also less pronounced, resulting in a lower sensitivity of approximately 50% to 60% and a decreased ability to detect small amounts of ischemia in patients with single-vessel disease. Atropine is required in all subjects in order to gather equivalent data. Vasodilator stress is commonly used in Europe and when myocardial perfusion data are sought with myocardial contrast echocardiography.
Atrial pacing, either by transvenous or transesophageal routes, has been used to achieve stress. The small increases in rate/pressure product and general poor tolerability of pacing have prevented this method from having general acceptance.
IMAGING TECHNIQUE
The typical treadmill protocol involves acquiring a series of resting images: parasternal long-axis, parasternal short-axis (including apical), and apical four-, three-, and two-chamber views. These images are stored digitally and then compared side by side with similar views acquired immediately poststress. During bike stress echo testing, images are recorded at rest and after each increment of load.
The dobutamine echo protocol starts with resting images in the same parasternal and apical views already mentioned. The infusion is started at 10 µg/kg/min, and this dose is increased every 3 minutes to 20, 30, and 40 µg/kg/min. Atropine is administered if the patient does not achieve >85% of predicted maximal heart rate (PMHR) and handgrip can also be added.
Harmonic imaging is now used routinely for better endocardial definition. LV opacification has an important role for patients with suboptimal images to improve visualization of endocardial thickening, as this is the most specific marker for ischemia.
INTERPRETATION OF STRESS ECHO
At rest, akinesis (excursion <2 to 3 mm) and dyskinetic segments are often believed to be consistent with a transmural infarct—certainly, this is more likely if the wall is also thinned (<6 mm). Hypokinetic segments demonstrate a partial infarct or viable myocardium.
Responses to stress echo and their interpretations are summarized in Table 11.1. Results are reported graphically in bull’s-eye form (Fig. 11.2), with segments assumed to correspond to a particular coronary distribution (Fig. 11.3). The traditional 16-segment ASE model has been supplanted by a 17-segment AHA model that includes the apical cap, although it needs to be acknowledged that the apex is often not visualized at 2-D echocardiography. Each wall segment is graded subjectively as normal, mildly hypokinetic, severely hypokinetic, akinetic, or dyskinetic in both the rest and stress images. A normal response to stress echo involves a global increase in contractility and hyperdynamic wall motion, and a gradual increase in heart rate. This is manifested by increased wall thickness, increased endocardial excursion, and a reduction in cavity size with stress.
TABLE
11.1 Stress Echocardiography Responses and Interpretation
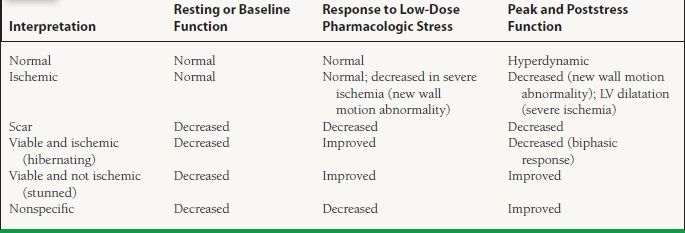
From Daly RP. Stress Echocardiography. In: Griffin BP, Topol EJ, eds. Manual of Cardiovascular Medicine, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2009:637, with permission from Wolters Kluwer Health.