Stress Echocardiography
Michael P. Brunner
I. INTRODUCTION.
Stress echocardiography (SE) is an effective method of evaluating for myocardial ischemia, based on the detection of stress-induced regional wall motion abnormalities (WMAs). Stressors include exercise, pharmacologic agents, and pacing. SE is used to screen for coronary artery disease (CAD), and it can help identify the coronary vessels involved. The accuracy of SE in the detection of significant coronary artery stenosis is 80% to 90%, which is superior to that of exercise electrocardiographic testing and comparable to that of nuclear stress imaging. In patients with left ventricular (LV) dysfunction and documented CAD, SE can differentiate viable myocardium from scarred myocardium, which may help predict whether LV function will improve after revascularization. As a diagnostic test for CAD, SE is safe and relatively inexpensive and can be rapidly performed by experienced hands. However, interpretation of SE images remains primarily subjective and requires a considerable learning curve. SE can also be used to assess the severity of valvular disease, hypertrophic cardiomyopathy, and exercise-induced pulmonary hypertension. In addition, it provides important prognostic information after myocardial infarction (MI) and prior to noncardiac surgery.
II. PATHOPHYSIOLOGY
A. Exercise stress testing.
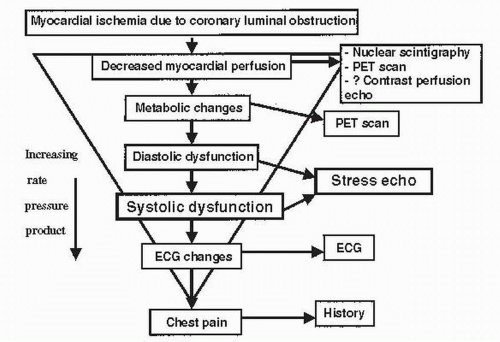
Myocardial ischemia results from a mismatch between oxygen supply and demand. The ischemic cascade is illustrated in Figure 49.1. Echocardiography detects ischemia by identifying new or worsening WMAs earlier in the cascade than detected by the electrocardiogram (ECG) or the onset of symptoms, but usually after the onset of worsening diastolic function. Exercise can be performed with a treadmill or an upright or supine bicycle.
B. Pharmacologic stress testing.
In patients who cannot exercise, pharmacologic stressors can be used. These drugs are sympathomimetic agents or vasodilators.
1. Sympathomimetic agents. Myocardial oxygen demand is determined by contractility (inotropy), heart rate (chronotropy), and wall stress (preload + afterload). Sympathomimetic agents produce stress by causing an increase in myocardial oxygen demand through increased inotropy, chronotropy, and blood pressure (BP) (afterload). Although a number of agents have been evaluated in combination with echocardiography, dobutamine is most widely used. Low-dose dobutamine has positive inotropic effects mediated through cardiac α1 and β1 receptors. At higher doses, it has positive chronotropic effects mediated through β2 receptors. The plasma half-life of dobutamine is 2 to 3 minutes. The normal response to dobutamine is an increase in heart rate and hyperdynamic wall motion, with only minimal effect on end-diastolic LV volume. It can be combined with atropine to achieve the usual target of at least 85% of age-predicted maximum heart rate (APMHR).
2. A vasodilator stress test is performed with dipyridamole or adenosine infusion. These agents result in perfusion abnormalities by causing blood to be preferentially shunted away from myocardial segments supplied by stenotic coronary arteries (i.e., coronary steal) and into more normal coronary vessels. This may lead to wall motion abnormality in the perfusion territory of the stenotic coronary artery that is seen on echocardiography. These agents are less commonly used for SE. Adenosine has fewer side effects than dipyridamole, owing to the former’s shorter half-life. However, because of the shorter duration of action of adenosine, the echocardiographic findings tend to be less pronounced and of shorter duration, resulting in a lower sensitivity.
3. The 2007 American Society of Echocardiography (ASE) guidelines recommend dobutamine as the first-line agent for pharmacologic SE. In addition, much of data for preoperative risk stratification and viability assessment using SE were derived from pharmacologic studies using dobutamine.
C. Atrial pacing.
Tachycardia induced by atrial pacing is an alternative to pharmacologic testing in patients that cannot exercise. In patients with a permanent pacemaker, stress is achieved by increasing the pacing rate until the target heart rate is reached. Transvenous and transesophageal pacing are considerations in patients without a permanent pacemaker.
III. INDICATIONS AND CHOICE OF STRESSOR
A. The indications and contraindications for SE testing are similar to those used for exercise electrocardiographic stress testing (see Chapter 47). The addition of an imaging modality improves the sensitivity and specificity of exercise electrocardiographic stress testing. Table 49.1 lists factors that may limit the sensitivity of electrocardiographic stress testing to detect CAD; patients with these factors benefit from a stress test utilizing an imaging modality (i.e., echocardiography, nuclear scintigraphy, or positron emission tomography [PET]).
B. Additional contraindications to SE occur with pharmacologic stress and depend on the underlying pharmacologic stressor. Patients with severe bronchospastic obstructive lung disease or high-grade atrioventricular (AV) block should avoid dipyridamole and adenosine. Patients with unstable ventricular arrhythmias should avoid dobutamine infusion. Relative contraindications to SE include unstable angina, severe baseline hypertension, uncontrolled arrhythmias, mobile LV thrombus, critical aortic stenosis (AS), hypertrophic obstructive cardiomyopathy, and decompensated heart failure.
C. Exercise stress is preferred over nonexercise stress because it more closely reproduces daily activity and is more sensitive in the detection of ischemia, provided the patient is able to achieve an adequate level of stress. No single exercise modality has been shown to have superior sensitivity, although the treadmill is more widely accepted among patients and physicians. Bicycle ergometry can be performed in the upright and supine positions. Images with treadmill stress testing must be obtained after exercise, whereas images may be obtained at peak exercise with bicycle ergometry while the patient continues to exercise. The sensitivity of treadmill testing to detect ischemia is reduced if images are not rapidly obtained (< 90 seconds) after exercise. However, the treadmill usually results in a greater level of stress than is associated with bicycle ergometry, which is more dependent on patient effort.
TABLE 49.1 Factors Limiting the Sensitivity of Stress Electrocardiography to Detect Coronary Artery Disease | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
D. Up to 30% of patients referred for exercise echocardiography may not be able to achieve an adequate level of exercise stress because of peripheral vascular disease, chronic obstructive pulmonary disease, or musculoskeletal problems. Pharmacologic stress testing is usually indicated in these patients.
IV. METHODOLOGY
A. Patient preparation
1. Patients should avoid heavy food intake for several hours before the test.
2. Rate-slowing agents (particularly β-blockers) blunt the normal heart rate response to exercise and may limit the ability of the patient to achieve at least 85% of the APMHR. This may reduce the sensitivity of the test results. If possible, these agents should be withheld before the stress test, unless the aim of the test is to evaluate their effectiveness in preventing exercise-induced ischemia.
3. The standard connections for a 12-lead ECG may be used with minor modifications to allow imaging in the parasternal and apical windows without affecting the accuracy of the exercise electrocardiographic testing results.
B. Equipment.
All SE studies are conducted with exercise electrocardiographic testing and standard hemodynamic monitoring equipment. A SE software package on the echocardiographic machine is necessary to acquire digital images and to allow side-by-side comparison of pre-stress images with peak stress or post-peak stress images. Resuscitation equipment and a defibrillator should be readily available.
C. Performing the test
1. Exercise SE. Regardless of the exercise modality, a quick, complete baseline echocardiographic scan is obtained for all patients. Resting images are obtained in the parasternal long- and short-axis and apical two- and four-chamber views and stored digitally. An apical long-axis view may be substituted for a parasternal long-axis view if the parasternal images are suboptimal. If endocardial definition is suboptimal, intravenous ultrasound contrast should be given to optimize the images.
a. Treadmill exercise is performed with standard protocols according to the functional status of the patient. Exercise is continued until at least 85% of the APMHR is reached, but it is preferably continued to the level of maximum exertion to maximize test sensitivity. APMHR equals 220 — age. Post-peak stress images are obtained as quickly as possible (in the left lateral decubitus position) after the patient transfers from the treadmill to the imaging table. Stress images in the same views as the baseline study are stored digitally and recorded on videotape. All post-peak stress images should be obtained within 90 seconds of completing exercise to maximize test sensitivity.
b. During upright bicycle echocardiography, baseline images are obtained in the standard left lateral position and are repeated with the patient in the upright position on the cycle ergometer. Adequate parasternal images may be recorded by having the patient lean forward. These images are recorded and digitized to allow comparable windows for the rest and peak stress images. Cycle ergometry is started at a workload of 25 W and increased by 25 to 50 W every 2 to 3 minutes until the patient reaches his or her level of perceived maximal effort. During upright bicycle echocardiography, images are obtained and digitized at rest, before peak, at peak, and after peak exercise.
c. With supine bicycle exercise, the entire study is performed while the patient is tilted 30° in the left lateral decubitus position, and images are obtained and digitized at rest, before peak, at peak, and after exercise. This exercise modality is not widely used.
d. Study end points for exercise SE include target heart rate (85% APMHR), severe electrocardiographic ischemia (ST-segment depression > 5 mm), intolerable symptoms (chest pain and dyspnea), severe hypertension
(systolic BP > 220 mm Hg or diastolic BP > 110 mm Hg), hypotension (systolic BP < 90 mm Hg or a fall in systolic BP > 20 mm Hg from baseline), ventricular tachycardia or sustained supraventricular tachycardia, and the development of new WMAs in at least two contiguous segments.
(systolic BP > 220 mm Hg or diastolic BP > 110 mm Hg), hypotension (systolic BP < 90 mm Hg or a fall in systolic BP > 20 mm Hg from baseline), ventricular tachycardia or sustained supraventricular tachycardia, and the development of new WMAs in at least two contiguous segments.
2. Pharmacologic SE
a. Dobutamine SE
(1) Dobutamine infusion is started at 10 µg/kg/min and increased every 3 minutes to 20, 30, and 40 µg/kg/min. If the patient has not reached 85% of APMHR by the end of the 40 µg/kg/min dose, a 3-minute dosage of 50 µg/kg/min may be used. Infusion is begun at lower doses (5 µg/kg/min) if baseline LV function is abnormal and myocardial viability is being sought. Images are digitized at rest and at low dosage (5 to 10 µg/kg/min), pre-peak dosage (30 µg/kg/min), and peak dosage.
(2) Atropine is used as needed to reach target heart rate > 85% of APMHR if dobutamine alone is not effective. Atropine (0.25 to 0.5 mg) is given intravenously every minute, starting at the 40 µg/kg/min dobutamine dose level and continuing until an end point is reached or a total dose of 2 mg is given. Atropine should be used with caution in patients that have glaucoma or benign prostatic hypertrophy. Isometric handgrip may be performed at the peak infusion rate to help achieve target heart rate.
(3) Study end points for dobutamine SE are the same as those used for exercise SE. If 85% APMHR has been achieved without any other end points, it is preferable to complete the protocol to the end of the 40 µg/kg/min infusion to increase the sensitivity of the test.
(4) Side effects. The most serious potential side effect of dobutamine is arrhythmia provocation. However, serious complications (e.g., arrhythmia, MI, and cardiac arrest) are rare, occurring in about 0.3% of studies in a large series of > 5,000 patients. Less serious side effects include tremor, nervousness, and marked hypertensive and hypotensive responses. The most common minor complication is hypotension, which usually responds to supportive therapy including intravenous fluids. A hypotensive response with dobutamine may be caused by ischemia and dynamic outflow tract obstruction or may result from the vasodilatory effect of dobutamine in combination with a small hyperdynamic LV and a low stroke volume.
(5) If angina or severe side effects develop, the effects of dobutamine may be reversed with intravenous β-blockade (0.5 to 1 mg/kg esmolol given over 1 minute or 2 to 5 mg/kg metoprolol given every 2 to 5 minutes). Like dobutamine, esmolol has a very short half-life and, therefore, may be preferable.
b. Dipyridamole or adenosine SE
(1) Patients with hypotension, AV block, or a history of severe bronchospasm should not undergo testing with these agents.
(2) Different protocols of dipyridamole infusion have been studied. The protocol recommended by the ASE is a low-dose two-stage infusion. The first stage begins at 0.56 mg/kg dipyridamole over 4 minutes; if no adverse effect or clinical end points are reached, an additional 0.28 mg/kg is infused over 2 minutes. A high-dose regimen of 0.84 mg/kg given over 10 minutes has been developed to improve the sensitivity of the test relative to low-dose protocols.
(3) Adenosine is given as a continuous infusion because of its very short halflife. A typical protocol starts at a low dose of 80 µg/kg/min and is increased every 3 minutes by 30 µg/kg/min to a peak dose of 170 to 200 µg/kg/min.
(4) Regadenoson is an adenosine receptor agonist with a 2 to 3-minute halflife, as compared with adenosine’s 30-second half-life. Regadenoson is administered as one 0.4-mg dose over 10 seconds.
(5) Study end points for dipyridamole or adenosine SE are similar to those used for exercise SE. A notable exception is that patients are not stressed until the APMHR is achieved. Additional end points include thirddegree AV block, severe hypotension, and intolerable side effects (e.g., bronchospasm). Symptoms usually start to resolve within 60 seconds after medication administration.
(6) If hypotension, bradycardia, or bronchospasm occurs, the effects of dipyridamole, adenosine, and regadenoson can be reversed with intravenous aminophylline 25 to 50 mg over 30 to 60 seconds.
D. Imaging techniques.
Modern technology allows digital image acquisition of multiple cardiac cycles and side-by-side comparison in a split screen display, enabling easy comparison of regional wall motion at rest and peak stress or after stress. Detailed frame-by-frame evaluation of wall thickening or excursion is possible, which helps in the evaluation of regional myocardial function. Obesity and lung disease remain the primary reasons for poor quality images. Harmonic imaging has improved endocardial definition, which can be further optimized with microbubble contrast agents.
1. Contrast echocardiography. Microbubble contrast agents provide improved echocardiographic resolution and allow real-time assessment of intracardiac blood flow. These agents are helpful when baseline SE images are suboptimal.
a. Intravenous agitated saline improves visualization of the right atrium and ventricle and enables visualization of intracardiac shunts. However, intravenous agitated saline is not able to cross the pulmonary circulation and opacify the left ventricle.
b. Second-generation microbubble contrast agents such as Optison and Definity incorporate perfluoropropane gas encased in an albumin-based or phospholipid shell, are more durable, and are able to cross the pulmonary circulation and opacify the left ventricle.
c. These agents are well tolerated and have a low complication rate. After initial concerns about safety, the FDA revised labeling requirements for second-generation contrast agents in 2008 and again in 2011. Patients with pulmonary hypertension or unstable cardiopulmonary conditions including acute coronary syndrome, worsening or unstable heart failure, serious ventricular arrhythmias, or respiratory failure no longer need to have their vital signs and oxygen saturation monitored for 30 minutes after injection.
Absolute contraindications to administration include previous hypersensitivity reaction and fixed right-to-left, bidirectional, or transient right-to-left cardiac shunts. Intra-arterial injection is contraindicated.
2. Real-time three-dimensional (3D) echocardiography. Significant advances have been made in 3D data acquisition without the need for off-line reconstruction. Three-dimensional imaging may shorten the acquisition period of post-exercise images or peak exercise images, allowing improved sensitivity and minimizing the technical strains imposed on the technologist obtaining the images. However, 3D SE is not routine in clinical use and remains under investigation.
V. IMAGE INTERPRETATION
A. Qualitative versus quantitative approach
1. Interpretation of SE findings is predominantly qualitative. Visual assessment of LV wall thickening and motion remains the standard method of interpretation of SE but is subject to interobserver and interinstitutional variability. Suggestions to optimize interpretation of SE images are outlined in Table 49.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree