6 Strain and Strain Rate Imaging
Basic Principles
Assessment of Left Ventricular Function
• The most widely used parameter for this measurement is ejection fraction (EF). Although this measure is simple and intuitive, as well as being supported by a wealth of prognostic information, it has important limitations:
• There is an emphasis on moving from the diagnosis of late heart failure (advanced structural change, poor outcome) to early stage heart failure (limited structural change—more chance of reversal). Early myocardial disease is usually characterized by:
Defining Strain
• Strain is a fundamental physical property of matter that reflects its deformation under an applied force.
• Strain may be measured as Lagrangian or natural strain:
• Lagrangian strain is defined on the basis of deformation from the original length (i.e., not subject to external forces): eL = {Lt − L(t=0)}/L(t=0)
• Natural strain is defined relative to a previous time instance but not original length: eN = ln {1 + et}
• In the tissue Doppler methodology, strain rate (SR) was derived from the gradient of velocity over a sampling distance, and strain obtained as the integral.
• Using speckle tracking, strain is derived from excursion of the speckles, and SR is derived from differentiation of the strain curve.
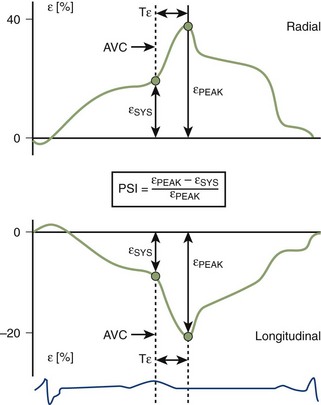
• Potential magnitude parameters include:
• Peak isovolumic relaxation (IVR) SR (i.e., peak SR between aortic valve closure [AVC] and mitral valve opening [MVO])
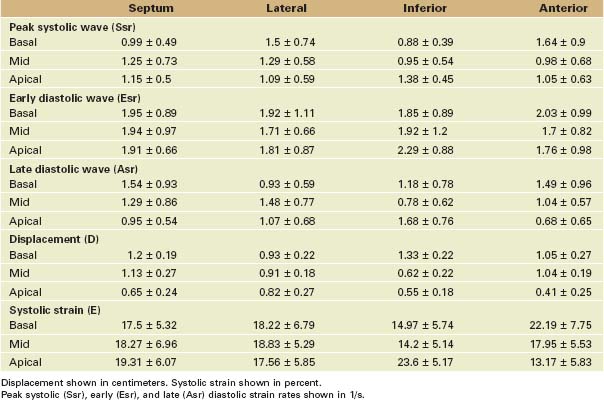
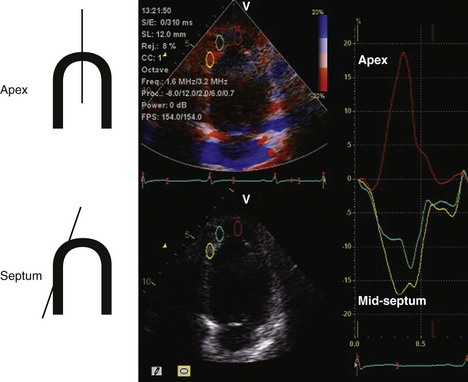
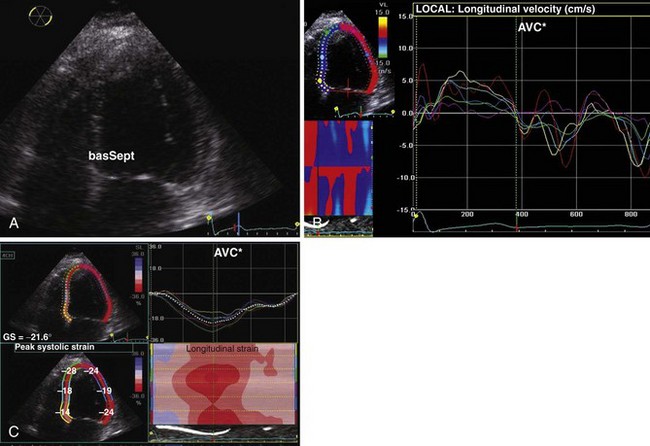
• Normal ranges of strain and SR have been described (Table 6-1). SR and strain may be expressed as curves relating to measures at one site (see Fig. 6-1) or in a parametric map (Fig. 6-2) where colors express magnitudes at various sites.
• There are minor differences between strain measurements provided by vendors. Nonetheless, strain and SR on all commercial systems have been extensively validated:
• Clinical validations have been performed on the basis of comparison with tagged magnetic resonance imaging (MRI) evidence of deformation. Unfortunately, this technique is imperfect.
Benefits of Strain
• Deformation offers four main benefits in comparison with other quantitative parameters: sensitivity, site specificity (i.e., independence from tethering), homogeneity, and physiologic significance (correlation with contractility):
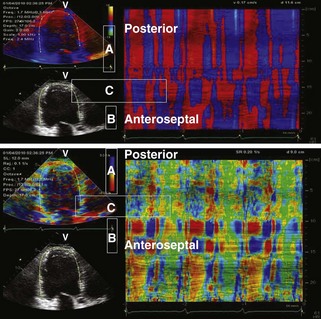
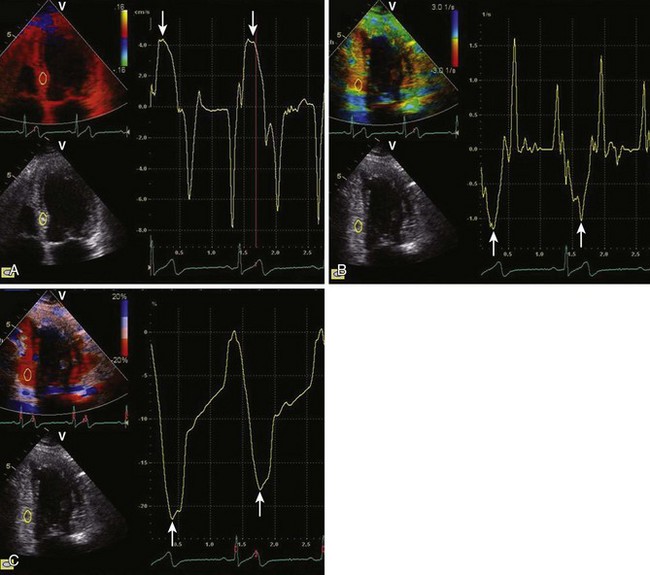
• The sensitivity of the deformation techniques to identify subtle gradations in function is an important attribute, especially for identifying early-stage disease. This is dependent on both having a narrow enough standard deviation to readily separate normal from abnormal tissue, as well as being specific for the location of the abnormal tissue (see Fig. 6-2).
• Site specificity implies that measurements obtained from within the sample volume truly reflect the performance of the tissue at this location rather than elsewhere in the wall. This is an inherent requirement for assessment of small areas of abnormal tissue, and techniques that are not site specific (e.g., tissue Doppler imaging or annular displacement) tend to average function along the length of the entire wall (see Fig. 6-2).
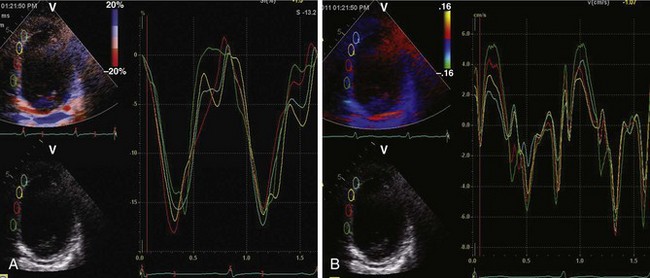
• The homogeneity of strain throughout the myocardium is relative rather than absolute, as there are minor variations of strain from apex to base. These variations are much less than the differences in tissue velocity within different parts of the heart (Fig. 6-3).
• The physiologic correlates of strain and SR have been sought in a number of experimental studies. Strain, which does not account for the time course of contraction, is analogous to regional EF. SR, a descriptor of the speed of contraction, is analogous to rate of change in pressure over time (dP/dt).
Disadvantages of Strain
• Measurement of myocardial deformation is a helpful but far from perfect technique for the assessment of regional or global LV function.
• None of the methods is independent of user expertise, to the extent that a variety of artifacts need to be recognized and avoided, in order to prevent misleading results.
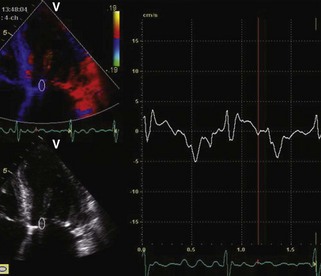
• The tissue velocity methodology is susceptible to artifact caused by angulation and works optimally when the direction of motion and the imaging access are as close as possible to parallel, and may be very misleading when angulation is major (Fig. 6-4).
Key Points
• LV EF is not an ideal measure of LV function because it depends on image quality, geometric assumptions, and loading conditions and is not sensitive for detection of early disease.
• Strain is defined as the change in myocardial length, relative either to original length or to length at a previous time, derived from excursion of speckles.
• SR is the rate of change in myocardial length (velocity), normalized to distance, and is the first derivative of the strain curve.
Methodologies
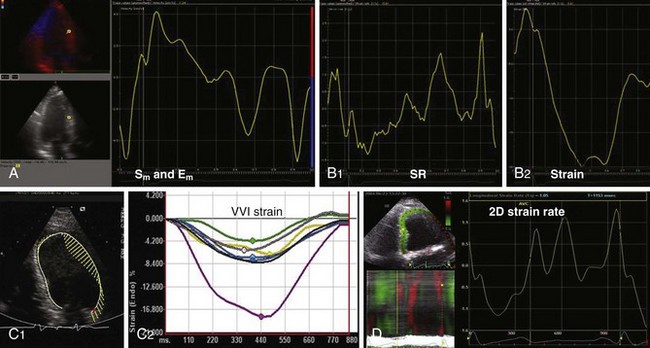
• They differ fundamentally according to whether tissue velocity or speckle is used as the primary modality (Fig. 6-5).
Tissue Doppler-based Strain
• The technique is based on comparison of the gradient of tissue velocity over the rate of change in length over a sample volume to obtain SR (ΔV/Δr). Strain is derived as the temporal integral of the spatial differential of velocity ∫(ΔV/Δr)δt.
• Interpretation steps
• Define start and end of systole using electrocardiography (end of T wave), aortic valve motion, color Doppler (isovolumic signal; Fig. 6-6) or LV outflow.
• Examine quality on the tissue Doppler; if there is artifact or aliasing, more complex analysis (i.e., strain) probably will not work.
• Move sample volume until a reproducible SR signal is obtained in the segment of interest and repeat in a reference segment. Measure peak systolic SR (Fig. 6-7).
• Limitations
• The motion that is measured should be parallel to the ultrasound beam, and generally this limits the application of the technique to apical images, although some work has been done in the anteroseptal and posterior walls from parasternal views.
• This technique is somewhat dependent on image quality, but the signal-to-noise ratio of Doppler is higher than for gray scale imaging, meaning that pictures unsuitable for tracing endocardial borders can sometimes provide accurate tissue velocity-based strain.
• The requirement for high frame rate, particularly for SR imaging, may be difficult to reconcile with a wide imaging sector.
Speckle-based Strain
• The application of 2D speckle technology on standard commercial machines is now more than 5 years old.
• How it works:
• The ultrasound image is composed of a matrix of speckles that correspond to minute tissue structures.
• Acquisition frame rate is extremely important, and optimal rate is 60 to 80 fps. If too low, speckles risk traveling out of the image; if too fast, the excursion between frames will be too small to measure.
• The adequacy of tracking can be expressed as the correlation between images. This can be mapped, to give the reader an impression for the reliability of the data, but apart from a process of offering minor guidance about tracking by one manufacturer, this quality control measure is unexploited.
• Strain measurement on archived images can be performed using some software that will process data from all vendors. However, caution needs to be applied to using this on DICOM images or the gray scale image in the background of color tissue velocity imaging (TVI), as the temporal resolution of both are too low for speckle tracking.
• The primary data are acquired as strain. SR can be calculated as the derivative of strain over time, but some constraints arise from acquisition frame rate (Fig. 6-8).
• Limitations
• Use after contrast left ventricular opacification is not feasible, presumably because of tracking contrast microbubbles in the myocardium.
Speckle- versus TVI-based Strain
• Generally, the feasibility and angle independence of speckle strain have made this the test of choice in the assessment of myocardial deformation.
• The relative simplicity of TVI means that this should be considered when there is no requirement for site specificity, especially if timing data are sought.
• TVI-based strain is preferable if assessment of deformation is sought at high heart rate (e.g., during stress) or there is a need to measure SR.