Chapter 3
Static lung volumes
Static lung volumes can be measured in the lung function laboratory by the following methods:
- Whole body plethysmography
- Multiple breath washout method
- Helium dilution method
- Single breath washout/dilution methods.
In individuals without airflow limitation, differences in measured lung volumes between methods are minimal. In obstructive disease, however, methodological differences may lead to substantial lung volume differences between methods. For example:
- Washout and dilution methods may underestimate results due to non-communicating regions in the lung being excluded from measurement.
- Plethysmography may overestimate results when the measured mouth pressure changes are not equivalent to alveolar pressure changes at zero flow. This typically occurs in the presence of substantial airway obstruction.
Test quality
Each method of measuring static lung volumes has its own particular requirements for equipment specifications, test performance and quality (1). The more general quality checks for static lung volumes include the following:
- No leak (mouth or equipment)—leak during any method of static lung volumes measurement will affect results and, as a consequence, results from trials affected by leak should not be used or reported.
- Spirometry performed as part of, or separately to, the lung volume measurement should meet the spirometry requirements for acceptable and repeatable results. Failure to perform spirometry adequately can result in underestimation or overestimation of total lung capacity (TLC) and/or residual volume (RV).
- To ensure that a maximal vital capacity (VC) has been measured, the VC(L) obtained during a static lung volume measurement should be compared to the (F)VC from spirometry. Ideally, VC should be greater than (F)VC—150 mL (where 150 mL is the repeatability criteria for VC and forced vital capacity, FVC).
- TLC obtained by static lung volume measurement should be greater than the alveolar volume (VA) obtained during gas transfer factor (TLCO) measurement.
- For plethysmography, three acceptable measures of functional residual capacity (FRC) within 5% of each other are required for a good quality result.
- For washout or dilution methods, often only one acceptable test is performed due to the length of time it takes for one trial to be carried out and the time required to return to normal resting conditions again. Caution should be used in interpretation of cases where only one acceptable effort is obtained. If more than one acceptable measurement is made, then the individual FRC measurements should be within 10% of each other.
- To ensure that a maximal vital capacity (VC) has been measured, the VC(L) obtained during a static lung volume measurement should be compared to the (F)VC from spirometry. Ideally, VC should be greater than (F)VC—150 mL (where 150 mL is the repeatability criteria for VC and forced vital capacity, FVC).
Review of the raw data may be required when concerns are raised regarding test quality, and cautionary statements should be used when relevant.
Interpretation
The parameters of static lung volumes generally used in interpretation are as follows:
- TLC—total lung capacity
- FRC—functional residual capacity
- RV—residual volume
- RV/TLC—the ratio of residual volume to total lung capacity
Limits of normal
For RV and RV/TLC, generally only abnormally high results are of interest. Hence, only an upper limit of normal (ULN) is used and it is defined as +1.64 z-scores.
For FRC and TLC, results can be abnormally high or low. The lower limit of normal (LLN) and ULN are set at −1.96 and +1.96 z-scores, respectively.
Note: The current interpretation guidelines set the LLN for TLC for restriction at −1.64 z-scores (fifth centile) (2). It is unclear why this is the case. A possible explanation is that the basic ventilatory defect interpretation strategies only use TLC to define restriction, hence only a LLN is set. Static lung volume measurements can provide information regarding consequences of airflow limitation (e.g. hyperinflation) as well as defining restriction; therefore, it can be argued that TLC should have both ULN and LLN.
Static lung volumes are generally reported in conjunction with spirometry results because the broad classifications of ventilatory defects include parameters from both spirometry (see Chapter 2) and static lung volume measurements.
Figure 3.1 depicts a flow diagram for interpretation of ventilatory function using spirometry and TLC from static lung volume measurements.
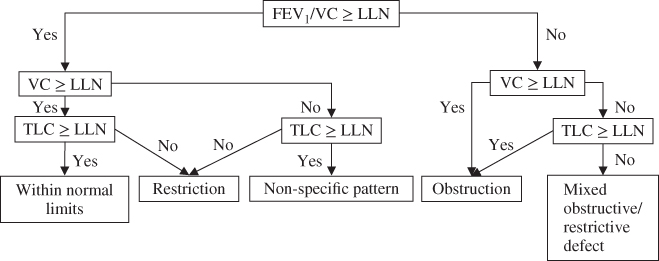
Figure 3.1 Ventilatory function interpretation strategy using spirometry and static lung volume measurements.
Adapted and reproduced with permission of the European Respiratory Society: Eur Respir J November 2005 26:948–968; doi:10.1183/09031936.05.00035205.
Once spirometry and TLC have been used to determine the ventilatory pattern (Figure 3.1), other parameters from static lung volumes can assist with further defining the pattern of abnormality (Table 3.1).
Table 3.1 After determining the ventilatory pattern using spirometry and TLC, other parameters of static lung volumes may be used to further define the pattern of abnormality.
| Using the interpretative strategy of Figure 3.1 | Parameters of static lung volumes | Pattern |
| Within normal limits | TLC > ULN, FRC > ULN or within normal limits RV/TLC < ULN | Possible large lung size |
| Obstruction | TLC, FRC < ULN, RV/TLC > ULN | Gas trapping due to airflow limitation |
| TLC < ULN FRC, RV/TLC > ULN | Hyperinflation (FRC) | |
| TLC, FRC, RV/TLC > ULN | Hyperinflation (TLC) | |
| Restriction | TLC < LLN FRC within normal limits RV/TLC > ULN | Possible neuromuscular weakness |
Consideration of the non-specific ventilatory pattern
Defined as TLC > LLN, FEV1/FVC > LLN, FVC and/or FEV1 < LLN (3), the non-specific pattern, although first identified in the early 1970s (4), has received little attention in interpretation circles. The pattern has been attributed to suboptimal test performance or obstruction (primarily small airways obstruction) (2). A study published in 2011, however, found that in approximately 1200 subjects presenting with the non-specific ventilatory pattern, the pattern persisted in approximately two-thirds of individuals on follow-up. Of the remaining third, the non-specific pattern differentiated to obstructive patterns, restrictive patterns, mixed patterns and results in the normal range over the follow-up period (3).
Comparisons to previous results
- There are no data in the literature defining a significant change in static lung volume parameters over time, nor do interpretation guidelines mention using parameters from static lung volume measures to assess changes over time (2).
- Changes in (F)VC and FEV1 are probably sufficient for identifying changes in ventilatory function over time.
Examples of interpretation of static lung volumes
Static lung volumes are usually interpreted in conjunction with spirometry results and interpretation is performed using the following steps as applicable:
- Check for requirements of cautionary statements related to the following:
- Reference values (are values appropriate for this subject?)
- Quality of test (read technical comments, check raw data if required)
- Reference values (are values appropriate for this subject?)
- Read clinical notes
- Follow flow chart of Figure 3.1
- Assess spirometry loop shape
- Assess response to inhaled bronchodilator
- Write technical interpretation
- Compare results to previous
- Put results into clinical context.

Full access? Get Clinical Tree


