Static (Absolute) Lung Volumes
Measures of the so-called static (or absolute) lung volumes are often informative.1 The most important are the vital capacity (VC), residual volume (RV), and total lung capacity (TLC). The VC is measured by having the subject inhale maximally and then exhale slowly and completely. This VC is called the slow vital capacity (SVC). Similar to the SVC is the inspiratory vital capacity (IVC). The patient breathes normally and then exhales slowly and completely and inhales maximally. The SVC and the IVC provide similar results. The SVC is used in this book rather than the IVC.
With complete exhaling, air still remains in the lung. This remaining volume is the RV. The RV can be visualized by comparing the inspiratory and expiratory chest radiographs (Fig. 3-1). The fact that the lungs do not collapse completely on full expiration is important physiologically. With complete collapse, transient hypoxemia would occur because mixed venous blood reaching the lung would have no oxygen to pick up. Furthermore, inflation of a collapsed lung requires very high inflating pressures, which would quickly fatigue the respiratory muscles and could tear the lung, leading to a pneumothorax. This is the problem in infants born with respiratory distress syndrome, in which portions of the lung can collapse (individual acinar units, up to whole lobes) at the end of exhalation.
3A. Slow Vital Capacity
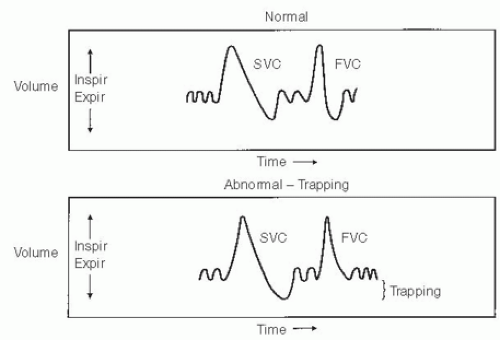
Normally, the SVC and forced expiratory vital capacity (FVC; discussed in Chapter 2) are identical, as shown in the top panel of Figure 3-2. With airway obstruction, as in chronic obstructive pulmonary disease (COPD) or asthma, the FVC can be considerably smaller than the SVC, as shown in the lower panel of Figure 3-2. The difference between SVC and FVC reflects trapping of air in the lungs. The higher flows during the FVC maneuver cause excessive narrowing and closure of diseased airways in COPD, and thus the lung cannot empty as completely as during the SVC maneuver. Although trapping is of interest to the physiologist, it is of limited value as a clinical measure. However, it does explain the possible discrepancies between the volumes of the SVC and the FVC.
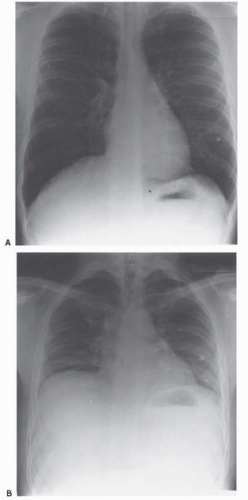 FIG. 3-1. Radiographs obtained from a healthy subject at full inspiration (i.e., at total lung capacity; A) and full expiration (B), in which the air remaining in the lung is the residual volume. |
3B. Residual Volume and Total Lung Capacity
Figure 3-3 depicts the static lung volumes that are of most interest. The RV is measured (see page 25) and added to the SVC to obtain the TLC. The expiratory reserve volume (ERV) is the volume of air that can be exhaled after a normal expiration during quiet breathing (tidal breathing). The volume used during tidal breathing is the tidal volume. The inspiratory reserve volume is the volume of air that can be inhaled at the end of a normal tidal inspiration. The sum of the ERV and RV is termed the functional residual capacity (FRC).
RV is the remaining volume of air in the lung at the end of a complete expiratory maneuver. It is determined by the limits of either the chest wall excursion or airway collapse or compression. In restrictive disorders, the limit of chest wall compression by the chest wall muscles determines RV. In obstructive disorders, the collapse of airways prevents air escape from the lungs, thereby determining the maximal amount exhaled. In obstructive disease, the RV is increased. There is one exception. The RV can be increased in a few young, healthy adults who are unable to completely compress their chest wall. In these cases, a curve like the one shown in Figure 2-6E is produced. The TLC is increased in most patients with chronic obstruction. However, TLC is often not increased in asthma. Finally, for a confident diagnosis of a restrictive process, the TLC must be decreased.
The FRC is primarily of interest to the physiologist. It is the lung volume at which the inward elastic recoil of the lung is balanced by the outward elastic forces of the relaxed chest wall (rib cage and abdomen). It is normally 40% to 50% of the TLC. When lung elasticity is reduced, as in emphysema,
the FRC increases. It also increases to a lesser extent with normal aging. With the increased lung recoil in pulmonary fibrosis, the FRC decreases.
the FRC increases. It also increases to a lesser extent with normal aging. With the increased lung recoil in pulmonary fibrosis, the FRC decreases.
PEARL: The FRC is normally less when a subject is supine than when sitting or standing. When a person is upright, the heavy abdominal contents pull the relaxed diaphragm down, expanding both the rib cage and the lungs. In the supine position, gravity no longer pulls the abdominal contents downward; instead, the contents tend to push the diaphragm up, and thus the FRC is decreased. The lower FRC and, hence, smaller lung volume in the supine position may interfere with gas exchange in patients with various types of lung disease and in the elderly. Blood drawn while these subjects are supine may show an abnormally low tension of oxygen in arterial blood. A similar effect often occurs in very obese subjects.
3C. How the Residual Volume Is Measured
Usually, the FRC is measured by one of the methods to be described. If the ERV is subtracted from the FRC, the RV is obtained and, as noted previously, if the RV is added to the SVC, the TLC is obtained (Fig. 3-3).
As shown in Figure 3-2, the SVC may be larger than the FVC in obstructive disease. If the FVC is added to the RV, the TLC will be smaller than if the SVC is used. Conversely, if the FVC is less than the SVC and the RV is calculated by subtracting the FVC from the measured TLC, you will calculate an RV that is high. By convention, and in this book, the SVC is used to compute static lung volume. Alternatively, in the United States, the FVC, not the SVC, is used to compute the FEV1/FVC ratio (ratio of the forced expiratory volume in 1 second to the FVC). European reference equations use FEV1/SVC, also called the Tiffeneau index.
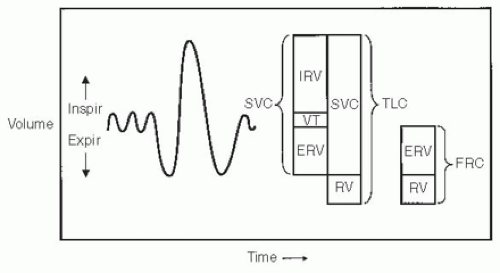 FIG. 3-3. Various static (or absolute) lung volumes. Total lung capacity (TLC) is the sum of the residual volume (RV) and slow vital capacity (SVC). The SVC is the sum of the inspiratory reserve volume (IRV), the tidal volume (VT), and the expiratory reserve volume (ERV). The functional residual capacity (FRC) is the sum of the RV and the ERV. Expir, expiration; Inspir, inspiration. |
The three most commonly used methods of measuring the FRC (from which the RV is obtained) are nitrogen washout, inert gas dilution, and plethysmography. If these are not available, a radiographic method can be used.
Nitrogen Washout Method
The principle of this procedure is illustrated in Figure 3-4. At the end of a normal expiration, the patient is connected to the system.
The lung contains an unknown volume (Vx) of air containing 80% nitrogen. With inspiration of nitrogen-free oxygen and exhalation into a separate bag, all the nitrogen can be washed out of the lung. The volume of the expired bag and its nitrogen concentration are measured, and the unknown volume is obtained with the simple mass balance equation. In practice, the procedure is terminated after 7 minutes and not all the nitrogen is removed from the lung, but this is easily corrected for. This procedure underestimates the FRC in patients with airway obstruction because in this condition there are lung regions that are very poorly ventilated, and hence, they lose very little of their nitrogen. A truer estimate in obstructive disease can be obtained if this test is prolonged to 15 to 20 minutes. However, patients then find the test unpleasant.
Inert Gas Dilution Technique
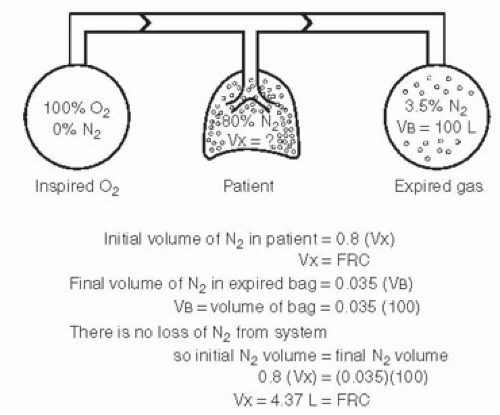 FIG. 3-4. Nitrogen washout method of measuring the functional residual capacity (FRC). The initial volume of nitrogen (N2) in the lungs at FRC equals 80% N2 × FRC volume. The N2 volume of the inhaled oxygen (O2) is zero. The volume of N2 washed out of the lung is computed as shown, and the FRC, or Vx, is obtained by solving the mass balance equation, 0.8 (Vx) = 0.035 (VB).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|