Public reporting has been proposed as a strategy to improve health care quality. Percutaneous coronary interventions (PCIs) performed in the United States from July 1, 2009, to June 30, 2011, included in the CathPCI Registry were identified (n = 1,340,213). Patient characteristics and predicted and observed in-hospital mortality were compared between patients treated with PCI in states with mandated public reporting (Massachusetts, New York, Pennsylvania) and states without mandated public reporting. Most PCIs occurred in states without mandatory public reporting (88%, n = 1,184,544). Relative to patients treated in nonpublic reporting states, those who underwent PCI in public reporting states had similar predicted in-hospital mortality (1.39% vs 1.37%, p = 0.17) but lower observed in-hospital mortality (1.19% vs 1.41%, adjusted odds ratio [OR adj ] 0.80; 95% confidence interval [CI] 0.74, 0.88; p <0.001). In patients for whom outcomes were available at 180 days, the differences in mortality persisted (4.6% vs 5.4%, OR adj 0.85, 95% CI 0.79 to 0.92, p <0.001), whereas there was no difference in myocardial infarction (OR adj 0.97, 95% CI 0.89 to 1.07) or revascularization (OR adj 1.05, 95% CI 0.92 to 1.20). Hospital readmissions were increased at 180 days in patients who underwent PCI in public reporting states (OR adj 1.08, 95% CI 1.03 to 1.12, p = 0.001). In conclusion, patients who underwent PCI in states with mandated public reporting of outcomes had similar predicted risks but significantly lower observed risks of death during hospitalization and in the 6 months after PCI. These findings support considering public reporting as a potential strategy for improving outcomes of patients who underwent PCI although further studies are warranted to delineate the reasons for these differences.
Three states currently mandate reporting of percutaneous coronary intervention (PCI) outcomes: New York since 1991, Pennsylvania since 2001, and Massachusetts since 2005. New Jersey has mandated the collection of data necessary to implement public reporting since 2007, but the state has not yet released the data to the public. We used the CathPCI Registry to evaluate the relation between mandatory public reporting and patient selection for PCI by identifying differences in patient characteristics, cardiac status, and indications for PCI in states with and without mandatory public reporting. In addition, we evaluated the relation between reporting and quality of care, as measured by care processes. Finally, we compared predicted and actual in-hospital mortality and other outcomes in patients who underwent PCI in states with and without mandatory public reporting.
Methods
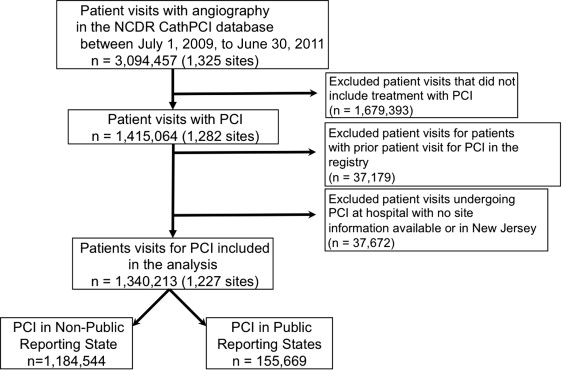
The CathPCI Registry is a national clinical registry program sponsored by the American College of Cardiology (ACC) and the Society for Cardiovascular Angiography and Interventions (SCAI) that has been previously described. All patient visits for PCI from July 1, 2009, to June 30, 2011, in version 4 of the CathPCI Registry (n = 1,340,213) were included. Procedures were categorized based on whether it was performed in a state that mandated public reporting of clinical outcomes to the state (New York, Pennsylvania, and Massachusetts) or without mandated public reporting of clinical outcomes (remainder of the CathPCI Registry; Figure 1 ).
New Jersey has been collecting data but has not implemented mandatory reporting and, thus, was analyzed separately. States (e.g., Maine, Ohio, Kentucky, Texas, Utah, Nevada, California, Colorado, Hawaii) that report risk-adjusted PCI mortality using Agency for Healthcare Research and Quality (AHRQ) all-payer hospital claims data were not considered to have public reporting. Although these claims data have been made publicly available, the risk adjustment methods developed by AHRQ do not contain clinical data and are specifically stated to be inappropriate to be used in isolation for comparison of hospitals.
Demographics, hospital characteristics, indications for PCI, and outcomes of patients who underwent PCI in states with mandated public reporting of clinical outcomes were compared. Tests of significance were performed using the chi-square test for categorical variables and the Wilcoxon rank-sum test for continuous variables. Standardized differences between the baseline characteristics of the 2 groups were calculated because of the large sample size.
Each patient’s predicted in-hospital mortality was determined using the National Cardiovascular Data Registry (NCDR) risk score model to determine if patients who underwent PCI in states with mandated public reporting of clinical outcomes were at similar baseline risk compared with patients treated in states without mandated reporting. The NCDR risk score has been previously described. For these analyses, the variables used in the original NCDR risk score were used to calibrate the model to provide the best statistical fit.
To determine whether differences in patient selection were present between reporting and nonreporting states, the risk difference between the predicted and observed mortality was determined. A generalized estimating equation logistic regression model accounting for within-site clustering was developed to evaluate the odds of in-hospital mortality after PCI in states with mandated public reporting of clinical outcomes compared with states without mandated reporting. An adjusted model was developed to control for differences in patient case mix (using variables contained in the full NCDR risk score model). Our final model controlled for all variables contained in the full NCDR risk score model plus additional potential confounders, such as patient and hospital characteristics. Stratified analyses were then used to determine whether differences between states with and without mandated public reporting of clinical outcomes varied within certain patient subgroups (elective PCI, acute coronary syndrome [ACS], cardiogenic shock).
Long-term outcomes are not available in the NCDR; however, certain long-term outcomes (death, myocardial infarction, repeat revascularization, readmission) were available in subset of patients at least 65 years of age who underwent an inpatient PCI from January 1, 2010, to December 31, 2011, that could be matched with the research-identifiable Medicare 100% inpatient fee-for-service claims file for a hospitalization that occurred at the same hospital (n = 247,017). The methods in which the NCDR and Medicare claims data were linked have been described previously. Data regarding readmissions were obtained from inpatient standard analytic files, and data regarding death were obtained from the Medicare enrollment database. The International Classification of Diseases, Ninth Revision, Clinical Modification, diagnosis codes were used to identify myocardial infarction (410.X1). International Classification of Diseases, Ninth Revision, Clinical Modification , procedure codes were used to identify coronary revascularizations (PCI 36.00, 36.06, 36.07, and 36.09 and coronary artery bypass grafting 36.10 to 36.19). Only revascularizations occurring after discharge from the index hospital stay were included in the revascularization analysis.
For long-term outcomes, unadjusted cumulative incidence curves (accounting for competing risk of death when necessary) and unadjusted/risk-adjusted odds ratio (OR adj ) at 180 days were calculated using the same methodology described earlier. The NCDR risk model was used to adjust the death analyses for potential confounders. For outcomes other than death, the Center for Medicare and Medicaid Services (CMS) readmission model variables were used for adjustment.
Analyses of the CathPCI Registry and Medicare claims data were approved by the Yale University Human Investigation Committee and performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina).
Results
We identified 1,340,213 patient visits from 1,227 unique sites who underwent the first PCI captured in version 4 of the CathPCI Registry. Most PCIs were performed in states that do not mandate public reporting of clinical outcomes (88%, n = 1,184,544), whereas 12% (n = 155,669) were performed in states that mandate public reporting. Of the PCIs performed in states with public reporting, 19% (n = 28,835) were performed in Massachusetts, 31% (n = 48,517) in New York, and 50% (n = 78,317) in Pennsylvania. In states with mandated public reporting of clinical outcomes, a higher proportion of patients had been transferred from another acute care facility to the hospital that performed the PCI (21.9% vs 18.7%, p <0.001).
Patients treated in states with mandated public reporting of clinical outcomes were older, more likely to be men, and a higher proportion had private insurance. They were less likely to have coexisting conditions such as heart failure, end-stage renal disease on hemodialysis, or diabetes ( Table 1 ). A higher proportion of patients in states without mandated public reporting underwent PCI for ACS with the largest difference being in those patients who underwent PCI for unstable angina. In contrast, a higher proportion of patients who underwent PCI in states with mandated public reporting of clinical outcomes underwent the procedure for stable angina. Fewer patients in states with mandated public reporting of clinical outcomes underwent a salvage procedure (defined as a procedure performed for patients in cardiogenic shock and who have either received chest compressions for a total of at least 60 seconds or have been on unanticipated extracorporeal circulatory support) (0.2% vs 0.3%, p <0.001). A slightly lower proportion of patients in states with mandated public reporting underwent PCI after cardiac arrest (1.8% vs 1.9%, p = 0.03) and cardiogenic shock (2.2% vs 2.5%, p <0.001).
Variable | Mandated Public Reporting | ||
|---|---|---|---|
| No (n=1,184,544) | Yes (n=155,669) | Standardized Difference | |
| Age, Mean (SD) | 64.6 (12.09) | 65.0 (12.11) | 0.03 |
| Women | 388,313 (32.8%) | 48,758 (31.3%) | 0.03 |
| White | 1,045,491 (88.3%) | 138,442 (88.9%) | 0.10 |
| Black | 97,741 (8.3%) | 10,798 (6.9%) | |
| Asian | 24,059 (2.0%) | 4,458 (2.9%) | |
| American Indian/Alaskan Native | 6,236 (0.5%) | 310 (0.2%) | |
| Native Hawaiian/Pacific Islander | 2,499 (0.2%) | 117 (0.1%) | |
| Insurance Provider | 0.27 | ||
| Private Health Insurance | 746,543 (63.0%) | 102,555 (65.9%) | |
| Medicare | 610,608 (51.6%) | 72,406 (46.5%) | |
| Medicaid | 108,083 (9.1%) | 14,943 (9.6%) | |
| Other | 54,512 (4.4%) | 4,355 (2.9%) | |
| None | 81,111 (6.9%) | 4,839 (3.1%) | |
| Indication for PCI | 0.10 | ||
| Elective PCI | 348,134 (29.4%) | 53,603 (34.4%) | |
| PCI for ACS | 806,034 (68.1%) | 98,593 (63.3%) | |
| PCI with Shock | 30,004 (2.5%) | 3,431 (2.2%) | |
| Prior MI | 353,857 (29.9%) | 45,576 (29.3%) | 0.01 |
| Prior Heart Failure | 139,560 (11.8%) | 16,589 (10.7%) | 0.04 |
| Prior PCI | 479,867 (40.5%) | 60,766 (39.0%) | 0.03 |
| Prior Coronary Bypass | 222,324 (18.8%) | 26,311 (16.9%) | 0.05 |
| Currently on Dialysis | 28,096 (2.4%) | 3,263 (2.1%) | 0.02 |
| Diabetes Mellitus | 428,005 (36.1%) | 54,945 (35.3%) | 0.02 |
| Presentation | 0.15 | ||
| No symptoms | 108,042 (9.1%) | 17,960 (11.5%) | |
| Symptoms unlikely to be ischemic | 35,549 (3.0%) | 3,924 (2.5%) | |
| Stable angina pectoris | 204,543 (17.3%) | 31,719 (20.4%) | |
| Unstable angina pectoris | 442,777 (37.4%) | 51,335 (33.0%) | |
| Non-STEMI | 210,443 (17.8%) | 26,908 (17.3%) | |
| ST-Elevation MI | 182,818 (15.4%) | 23,781 (15.3%) | |
| PCI Status | 0.06 | ||
| Elective | 536,556 (45.3%) | 66,312 (42.6%) | |
| Urgent | 443,538 (37.4%) | 62,484 (40.1%) | |
| Emergency | 199,813 (16.9%) | 26,426 (17.0%) | |
| Salvage | 3,948 (0.3%) | 366 (0.2%) | |
| Cardiac Arrest within 24 Hours | 22,290 (1.9%) | 2,803 (1.8%) | 0.01 |
| IABP | 29,502 (2.5%) | 4,382 (2.8%) | 0.02 |
| Left Ventricular Ejection Fraction < 30% | 45,884 (3.9%) | 5,863 (3.8%) | 0.01 |
There were modest differences in the delivery of care when comparing states with mandated reporting of clinical outcomes to states without these programs ( Table 2 ). The median door to balloon times for patients who underwent primary PCI in states with mandated public reporting of clinical outcomes were similar. There was better utilization of evidence-based medications in states with mandated public reporting, with a higher proportion of patients discharged on aspirin (96.8% vs 95.0%, p <0.001), ß blockers (85.0% vs 80.9%, p <0.001), statins (89.1% vs 86.6%, p <0.001), and thienopyridines (97.0% vs 96.3%, p <0.001). The proportion of PCIs considered appropriate using the ACC Appropriate Use Criteria was lower in patients who underwent PCI in public reporting states ( Supplementary Table 1 ).
| Mandated Public Reporting | |||
|---|---|---|---|
| No | Yes | P-Value ∗ | |
| Red Blood Cell Transfusion | 31,856 (2.7%) | 3,747 (2.4%) | <0.001 |
| PCI performed with Large Contrast Volume | 307,902 (30.5%) | 42,567 (29.6%) | <0.001 |
| Door to balloon time (in patients with immediate PCI for STEMI), minutes, median (25th,75th percentiles) | 62 (47, 78) | 62 (46, 78) | 0.87 |
| Discharge Medications in Patients Discharged Alive | |||
| ACE-Inhibitor/ARB | 743,411 (63.7%) | 94,651 (61.5%) | <0.001 |
| Aspirin | 1,109,767 (95.0%) | 148,950 (96.8%) | <0.001 |
| Beta Blockers | 944,403 (80.9%) | 130,807 (85.0%) | <0.001 |
| Statin | 1,011,008 (86.6%) | 137,003 (89.1%) | <0.001 |
| Non-Statin | 189,742 (16.3%) | 22,199 (14.4%) | <0.001 |
| Any Thienopyridines | 1,113,558 (96.3%) | 148,121 (97.0%) | <0.001 |
| Clopidogrel | 971,065 (83.2%) | 132,979 (86.5%) | <0.001 |
| Ticlopidine | 3,877 (0.3%) | 625 (0.4%) | <0.001 |
| Prasugrel | 141,028 (12.1%) | 14,908 (9.7%) | <0.001 |
∗ All tests compare public reporting states to non-public reporting states within each rows’ designated group (e.g. All patients in public reporting states versus all patients in non-public reporting states).
Patients who underwent PCI in states with mandated public reporting of clinical outcomes had similar NCDR model-predicted in-hospital mortality (1.39% vs 1.37%, p = 0.17) but lower observed mortality (1.19% vs 1.41%, p <0.001) relative to patients treated in states without mandated public reporting ( Table 3 ). Patients who underwent PCI in states with mandated public reporting of clinical outcomes had significantly lower in-hospital mortality after adjusting for baseline risk and other potential confounders (OR adj 0.80, 95% confidence interval [CI] 0.74 to 0.88, p <0.001; Figure 2 ).
| Mandated Public Reporting | |||
|---|---|---|---|
| No (n=1,184,544) | Yes (n=155,669) | P-Value | |
| All Patients Undergoing PCI | |||
| Predicted Mortality based on NCDR Risk Score %, (SE) | 1.39 (0.01) | 1.37 (0.01) | 0.17 |
| Actual Mortality %, (SE) | 1.41 (0.01) | 1.19 (0.03) | <0.001 |
| Difference between Predicted/Actual Mortality (%) | +0.02 | -0.18 | |
| Patients Undergoing Elective PCI | |||
| Predicted Mortality based on NCDR Risk Score %, (SE) | 0.36 (0.003) | 0.37 (0.01) | 0.26 |
| Actual Mortality %, (SE) | 0.33 (0.01) | 0.25 (0.02) | 0.003 |
| Difference between Predicted/Actual Mortality (%) | -0.03 | -0.12 | |
| Patients undergoingUndergoing PCI for ACS | |||
| Predicted Mortality based on NCDR Risk Score %, (SE) | 0.98 (0.003) | 1.05 (0.01) | <0.001 |
| Actual Mortality %, (SE) | 0.90 (0.01) | 0.82 (0.03) | 0.02 |
| Difference between Predicted/Actual Mortality (%) | -0.08 | -0.24 | |
| Patients Undergoing PCI with Cardiogenic Shock | |||
| Predicted Mortality based on NCDR Risk Score %, (SE) | 24.38 (0.14) | 26.00 (0.43) | <0.001 |
| Actual Mortality %, (SE) | 27.92 (0.26) | 26.61 (0.76) | 0.11 |
| Difference between Predicted/Actual Mortality (%) | +3.54 | +0.61 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


