Fig. 10.1
Factors influencing the stabilization of the coronary artery on a beating heart
Here is a hypothesis or assumption on the relationship among stabilization, surgeon skill, and graft patency. Intuitively, residual motion of the anastomosis sites under efforts for stabilization affects the graft patency (Fig. 10.2). When the residual motion is acceptable for the surgeon, he or she feels comfortable enough to place precise stitches, making a good anastomosis with excellent graft patency. If the residual motion of anastomosis site were too big to make an acceptable anastomosis, expected graft patency would decease dramatically.
Fig. 10.2
Hypothesis: stabilization-patency relationship in off-pump coronary artery bypass grafting. For trainees with less experience, acceptable graft patency can be achieved only when the anastomosis site stabilization is near perfect (100 %). For expert surgeons, acceptable graft patency can be achieved as long as the anastomosis site stabilization is not poor. This relationship curve can be shifted to the left by surgical skill training
Surgeon’s skill is another factor for graft patency. The stabilization-patency relationship can be shifted to left by surgical training. The expert surgeon is able to manage to work on the moving coronary artery somehow, while the surgical resident is not. However, there is a human limit for working on a moving small target even for the expert surgeon. Thus, here is a hypothesis that these 2 factors, stabilization and surgeon skill, may affect the configuration of the anastomosis and graft patency. Therefore, surgical training (see Chap. 26: Teaching and training) and stabilization is the key for successful off-pump coronary artery surgery. Here comes the next question: regarding the stabilization, how good is good enough for surgeons to provide an acceptable graft patency?
10.1.2 How Good Is Good Enough for Stabilization?
An expert off-pump surgeon can make a good stitch on the moving coronary artery. However, there is a human limit of acceptable motion of the target. Figure 10.3 shows a scheme of suturing the moving coronary artery. The task of a surgeon is to hold the coronary artery adventitia and make a precise stitch without laceration of the wall. The coronary artery wall is soft and flexible and can be held to make immobile point even on the moving floor made with myocardium and fat tissue. Try to hold the coronary artery wall by forceps. If it can be held to be immobile without any tension, a surgeon can make a incision and stitches. If a surgeon feels any traction force on the holding point, delicate procedure around the holding point on the coronary wall without a risk of laceration is not recommended. In summary, a surgeon can confirm if he or she obtains an acceptable stabilization by holding the target coronary artery wall in static position.
Fig. 10.3
Suture in off-pump coronary artery bypass grafting. The bases of the coronary arteries are fixed to the contracting myocardium. The coronary artery wall can be held immobile, because the wall and surrounding fat are flexible
10.2 Evaluation of Stabilization
The motion of target anastomosis areas during off-pump coronary artery bypass is an important issue for cardiac surgeons. Several attempts for evaluating the cardiac surface motion in a quantitative fashion have been reported. In 1996, Borst and associates [2] reported that a mechanical stabilizer (Octopus) significantly reduced the area circumscribed by the 2-dimensional reference points on the right coronary artery and obtuse marginal branch in pigs by using an analog video camera. In 2002, Detter and associates [3] measured the deviation of small vessels in the anterior wall by using an orthogonal polarizations spectral imaging device, reporting that the deviation was significantly decreased with mechanical stabilizers. They also showed better stabilization is associated with shorter anastomosis time. In 2003, Koransky and associates [4] 3-dimensionally reconstructed the motion of the left anterior descending artery with digital sonomicrometry. They reported that mechanical stabilization significantly reduced the 3-dimensional excursion, maximum velocity, and average velocity. In 2004, Cattin and associates [5] captured the wall movements of the beating heart by using a high-speed camera coupled with a laser sensor, analyzing the trajectory of the point of interest. In their system, the 2-dimensional lateral motion (x-, y-axis) was captured with the high-speed camera, and the out-of-plane motion (z-axis) was acquired with the laser sensor. In 2005, Lemma and associates [6] captured the coronary artery simultaneously with two digital cameras, reconstructing the wall movements of the heart in 3-dimensional fashion. They quantitatively reported the distance of marker displacement on the beating heart in the Cartesian coordinate system (x-, y-, z-axis) before and after stabilization.
Most recently, Watanabe and associates developed a 3-dimensional digital motion capture and reconstruction system [7], which is an application of modern robotic technology (Fig. 10.4). The new digital system is able to reconstruct the 3-dimensional motion of any coronary arteries such as distance moved, velocity, acceleration, and deceleration in every region and every axis. By the use of an endoscope with high-speed camera (955 frames per second), accuracy of mean resolution (70 ± 6 μm) and time resolution of 3-dimensional data points (480 xyz position data per second) are improved. The endoscope and the small lightweight markers for tracking can be sterilized and used in any clinical procedure. In the following chapters, several studies using this system are introduced.
Fig. 10.4
(a) Three-dimensional digital motion capture and reconstruction system. Two high-speed cameras lining in a different angle capture the motion of markers on the beating heart. These 2-dimensional position data of the surface of the coronary artery are reconstructed into 3-dimensional data in the master computer. (b) An example of 3-dimensional coronary artery motion in one cardiac cycle
10.3 Tissue Stabilizers
10.3.1 Pre-Octopus Era: Tape, Snare, etc
In the previous era before Octopus or other suction-type tissue stabilizer, many efforts to stabilize the coronary anastomosis site were reported [8–12]. These efforts include tape, snare, and stitches around the target coronary artery, which are still useful in addition of the current suction-type tissue stabilizer. Because the effects of tissue stabilization depends on the local factor such as fat deposition around the anastomosis site and the tortuosity of the target coronary artery, few stitches around the coronary anastomosis site with traction, for example, may provide further stabilization. The off-pump surgeon needs to know the history and should apply these inexpensive, simple, and effective techniques when appropriate.
10.3.2 Suction-Type Tissue Stabilizer
In 1996, Borst and colleagues developed Octopus tissue stabilizer, which immobilizes the epicardium using a suction device [2]. Jansen and colleagues used this device for the patients who underwent off-pump coronary artery bypass [13]. With an aid of the Octopus tissue stabilizer, off-pump technique became popular in the late 1990s. Several suction-type tissue stabilizers are now available (Fig. 10.5), becoming the common, simple modality for off-pump coronary artery bypass surgery.
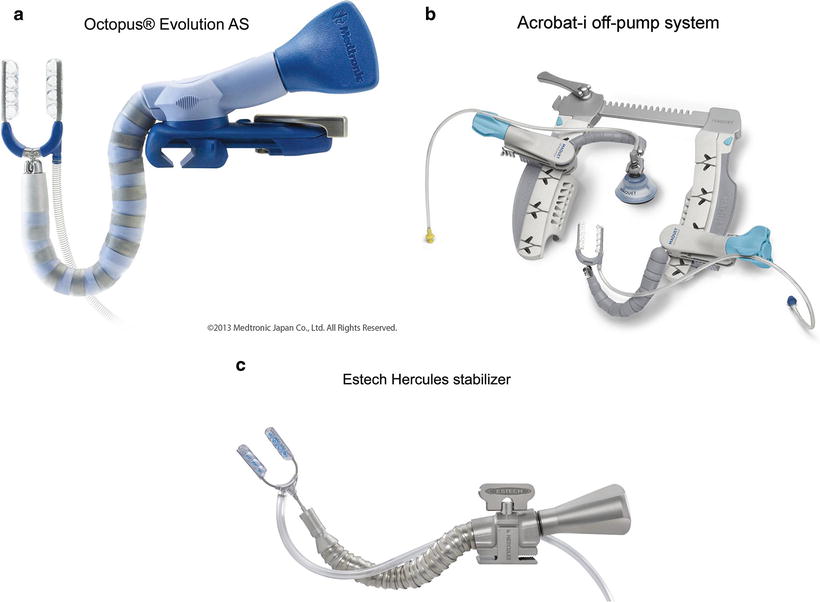
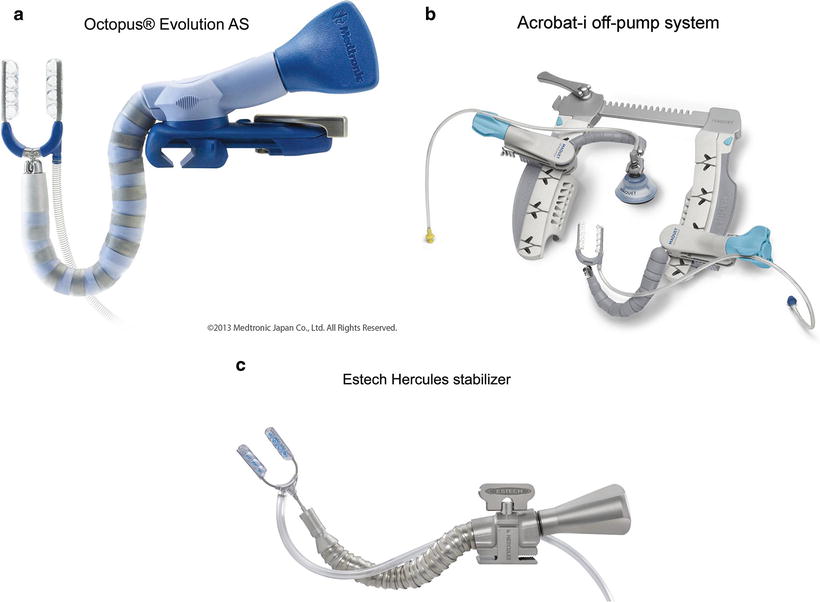
Fig. 10.5
Modern suction-type tissue stabilizers on the market. (a) Medtronic Octopus Evolution AS. (b) CTS Acrobat-i Off-Pump System. (c) Estech Hercules stabilizer
In an animal study, Watanabe and associates [7] found that mechanical stabilization (Octopus) can reduce the distance moved during one cardiac cycle remarkably, while the rapid, sudden movements such as maximal velocity, acceleration, and deceleration are not decreased much (Fig. 10.6). In detail, the distance moved in one cardiac cycle is decreased to 15.9 % of the baseline value (84.1 % reduction below the baseline when the baseline value is assumed as 100 %) in the left anterior descending artery by the Octopus stabilization, while maximum velocity, acceleration, and deceleration is only decreased to 62.5 % (37.5 % reduction), 65.3 % (34.7 % reduction), and 64.1 % (35.9 % reduction), respectively. In other words, “sudden quick motion” remains even under the most recent sophisticated mechanical tissue stabilizer. Several efforts to decrease these sudden quick motions are introduced in the following sections.
10.4 Pharmacological Stabilization: Beta-Blocker
β-adrenergic receptors are mainly located in the heart, blood vessels, and bronchi. β1-receptor blockers decrease heart rate (negative chronotropic effect) and myocardial contraction force (negative inotropic effect), whereas β2-receptor blockers dilate the smooth muscle of blood vessels in the heart, brain, and other organs and contract the smooth muscle of the trachea. In the clinical settings, β-receptor blockers have been used for the patients with heart disease as antihypertensive, anti-arrhythmic, and antianginal agents. For the patients with ischemic heart disease, β1-receptor blockers also reduced myocardial damage in acute myocardial ischemia since they reduce myocardial metabolic requirements during ischemia and increase oxygen delivery to the ischemic myocardium during and after ischemia [14–17]. A recent study demonstrated that coronary anastomosis time during off-pump coronary artery bypass was shorter under an infusion of esmolol, a short-acting β1-blocker, suggesting favorable stabilization during β1-blocker infusion [17].
Propranolol (Fig. 10.7), a nonselective β1– and β2-receptor blocker, was first introduced as an anti-tachycardia and anti-tachyarrhythmia drug during coronary artery bypass surgery. However, propranolol has a long duration of action time (2–14 h) with several side effects such as conduction disturbance, hypotension, and cardiac failure [14, 15]. Propranolol also blocks β2-receptor with a risk of perioperative asthma attacks. Esmolol (Fig. 10.7), an ultra-short-acting selective β1-receptor blocker, has been developed recently to avoid these side effects [14, 15]. More recently, landiolol hydrochloride (Fig. 10.7) has been developed by modifying the chemical structure of esmolol, to increase β1-receptor selectivity and potency without affecting the duration of action. This agent has some unique characteristics. Landiolol hydrochloride has a very rapid onset and offset of action [14–16, 18, 19]. Compared with esmolol, heart rate decreases more rapidly with landiolol [15–18]. Landiolol is rapidly metabolized by serum pseudocholinesterase and liver carboxylesterase to an inactive metabolite in humans within a half-life of 4 min, which is shorter than that of esmolol [14, 16, 18–20]. Renal and hepatic clearance does not contribute to the pharmacokinetics of this agent at clinical concentrations [18–20] which is useful for intraoperative infusion for the patients with renal and/or hepatic dysfunction [20]. Landiolol hydrochloride has higher β1-selectivity than any other known β-blocker [19]. It also suppresses ventricular and supraventricular arrhythmias in experimental settings [18, 19]. Furthermore, landiolol does not produce the dose-dependent decrease in mean arterial pressure like esmolol [15, 19], which seems to be suitable for off-pump coronary artery bypass surgery.