Most data on heart failure biomarkers have been derived from patient cohorts with chronic disease. However, risk prediction in patients admitted with acute decompensated heart failure (ADHF) remains a challenge. ADHF is not a single disease: it presents in various manners, and different causes may underlie ADHF, which may be reflected by different biomarkers. Soluble suppression of tumorigenicity 2 (ST2) has been shown to be a strong independent predictor of short-, mid-, and long-term outcome in ADHF. Furthermore, combining biomarkers may help further improve the prognostic power of ST2. The ProBNP Investigation of Dyspnea in the Emergency Department study showed that elevated plasma levels of ST2 together with elevated levels of 4 other biomarkers have clear incremental values to predict outcome in ADHF. The Multinational Observational Cohort on Acute Heart Failure study is an international collaborative network that recruited 5,306 patients hospitalized for ADHF that demonstrated that ST2 and midregional pro-adrenomedulin had independently strong value to predict 30-day and 1-year outcome in patients with ADHF. The Multinational Observational Cohort on Acute Heart Failure study also showed that C-reactive protein plus ST2 better classified risk in patients with ADHFs than ST2 alone. Combining biomarkers for risk prediction or risk stratification might have clinical and more importantly pathophysiological meaning.
The use of biomarkers to assist in the care of acute decompensated heart failure (ADHF) patients has been an area of vastly expanding research. Natriuretic peptides (NPs) represent the current biomarker gold standard for diagnosis and prognosis in patients with ADHF. Subsequent study of the NPs demonstrates considerable opportunity to add to the prognostic information gained from their measurement. In this regard, newer biomarkers have been studied either alone or together with the NPs. Elevated plasma levels of the interleukin receptor family member suppression of tumorigenicity 2 (ST2) and others, such as midregional pro-adrenomedullin (MR-proADM), the pro-peptide of a prognostically meaningful endogenous vasoconstrictor, have been individually shown to be associated with poorer outcome in ADHF. Recently, various studies tested combined biomarkers to predict outcome in ADHF. Indeed, plasma levels of NPs are more related to myocardial stress, whereas MR-proADM might be more related to global stress and ST2 might better reflect ventricular fibrosis and remodeling. Combining those novel biomarkers was shown to have additive values.
Clinical Models to Risk Stratify Severe Critically Ill Patients
Different prognostic systems, such as the Acute Physiology and Chronic Health Evaluation II or III, the Simplified Acute Physiology Score (SAPS) II, and the Mortality Probability Models II, have been developed to predict the outcome of critically ill patients admitted to the intensive care unit (ICU). SAPS II provides a method to convert the score to a probability of hospital mortality and includes several key clinical parameters and biological markers, measured all at admission and known to alter outcome. Clinical parameters include age, gender, cause of ICU admission, co-morbidities, blood pressure, heart rate, and temperature. Several biological parameters recorded at admission are used to calculate the SAPS II, including arterial oxygenation, bicarbonates, liver and renal function markers, and potassium and sodium. SAPS II score can, however, only be measured at admission and is not used to follow patient condition. SAPS II has been shown to be a moderate marker of 28-day outcome.
To follow the severity of patients admitted in the ICU during their initial hospital stay, an organ dysfunction score has been developed, The Sepsis-Related Organ Failure Assessment (SOFA) score to describe organ dysfunction/failure. The SOFA score is mostly based on biological markers and has been seen by intensivists as a “multimarker strategy” to predict outcome. Indeed, in septic patients, various organ dysfunctions are present at admission, and the degree and the number of organ dysfunction are associated with outcome. SOFA score was described to assess the degree and the number of organ dysfunction at admission and during the following days. SOFA score is mostly based on biological markers and includes respiratory, kidney, liver, and coagulation markers. Importantly, none of the aforementioned scores include measurement of cardiac biomarkers.
Combined Troponin and NPs Use in ADHF
Plasma measurements of troponin and NPs are recommended in the initial phase of ADHF management. Plasma troponin levels may help ruling out an acute myocardial infarction as a main cause of ADHF. Elevated cardiac troponin levels at admission have also been correlated with poor prognosis. It has further been demonstrated that patients with ADHF with detectable troponin I and elevated BNP were at particularly high risk of death, whereas patients with ADHF without detectable troponin I and lower BNP levels had a substantially lower risk of adverse outcome. With the development and spread of highly sensitive troponin methods, the prognostic impact of troponin measurement has increased.
Combined Troponin and NPs Use in ADHF
Plasma measurements of troponin and NPs are recommended in the initial phase of ADHF management. Plasma troponin levels may help ruling out an acute myocardial infarction as a main cause of ADHF. Elevated cardiac troponin levels at admission have also been correlated with poor prognosis. It has further been demonstrated that patients with ADHF with detectable troponin I and elevated BNP were at particularly high risk of death, whereas patients with ADHF without detectable troponin I and lower BNP levels had a substantially lower risk of adverse outcome. With the development and spread of highly sensitive troponin methods, the prognostic impact of troponin measurement has increased.
Multimarker Strategy Including ST2 in Patients Admitted for Acute Dyspnea
Pascual-Figal et al prospectively studied 107 patients hospitalized with ADHF (mean age 72 ± 13 years, 44% men, left ventricular ejection fraction 47 ± 15%). Blood samples were collected on presentation to measure ST2 (reflective of myocardial fibrosis and remodeling), high-sensitivity troponin T (hsTnT—indicative of myocardial necrosis), and N-Terminal Pro-B-Type Natriuretic Peptide (NT-proBNP) (identifying myocardial stretch) levels. Each provided independent and additive prognostic information for death in the shorter and longer term. Furthermore, a simple combined multimarker score powerfully identified patients at low, intermediate, and high risk for all-cause mortality. The presence of none, 1, 2, or 3 elevated biomarkers was associated with a strikingly steeply rising incremental risk of death, ranging from 0% to 50%. The addition of this simple multimarker score significantly increased the predictive performance achieved by the entire model taking into account clinical predictors plus NT-proBNP levels. The survival curves suggest that biomarkers add prognostic information during the first year and clearly separate those patients at low risk (none or 1 biomarker elevated) from those at high risk (≥2 biomarkers elevated). This simple and objective ability to stratify patients into very low and very high risk could be used to triage patients with ADHF to different therapeutic interventions, ranging from low-risk HF observation units to earlier triage to mechanical support for those at very high risk.
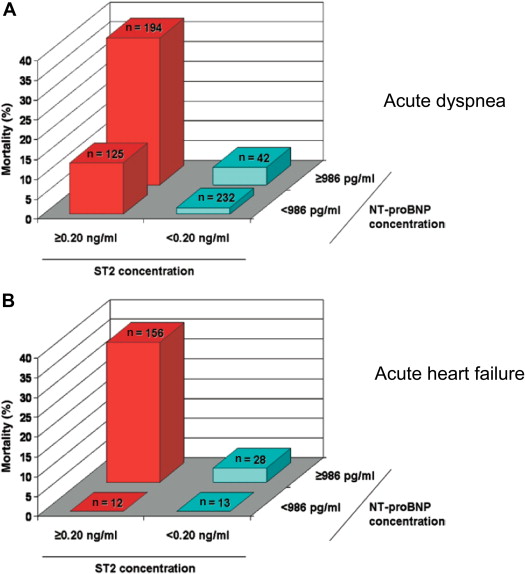
A multimarker strategy has also been evaluated by the Pro-B–type natriuretic peptide Investigation of Dyspnea in the Emergency Department (PRIDE) Investigators. Of 560 patients from PRIDE, 180 had ADHF. Concentrations of NT-proBNP, MR-proADM, and MR-proANP were measured, and patients were followed for 4 years for survival. In comprehensive statistical analyses, both midregional peptides were associated with death out to 4 years, individually or in a multimarker strategy. Figure 1 further shows that the association of ST2 and NT-proBNP might have additive values to predict 1-year outcome in patients with both acute heart failure and more globally acute dyspnea.