Fig. 8.1
(a) Graphic transcription of daily compliance and pattern of use of a ventilator provided by ventilator software in a patient who is well adapted to his ventilator, with excellent compliance. Use of the ventilator during the night is continuous, without interruption, suggesting acceptable quality of sleep. (b) Graphic transcription of daily compliance and pattern of use of ventilator provided by ventilator software in a patient who tolerates his treatment poorly, revealing multiple interruptions during the night, and days without ventilator use (Adapted from Ref. [2])

Fig. 8.2
Upper graph: pattern of use; Lower graph: total daily use. Graphic illustration of pattern of use and total daily use in a COPD patient with poor adaptation to NIV. Note frequent interruption during treatment, days with no treatment, and daily use <4 h. Six days before admission to the respiratory ward for acute exacerbations of COPD, the patient complained of shortness of breath that was alleviated by NIV, as evidenced by a rapid increase in daily use
A detailed report on compliance is important for deciding whether or not to pursue ventilatory support, discussing alternate patterns of daily use of NIV in case of poor tolerance during the night (i.e., daytime sessions), and understanding insufficient impact of NIV on arterial blood gases (ABG) or clinical symptoms.
8.3 VT and Minute Ventilation
Although leaks have traditionally been a problem in volume-cycled NIV, pressure cycling and advances in blower technology now allow a certain amount of unintentional leakage without affecting pressurization capabilities and efficient delivery of VT, at least in some ventilators [4]. This is of major importance because unintentional leaks are a clinical reality in unsupervised patients treated by domiciliary NIV.
In single-limb circuits with a vented mask, the built-in flow sensor monitors total gas flow, that is, the sum of respiratory flow and unintentional and intentional leaks (Fig. 8.3). Because there is no direct measurement of expiratory flow in a single-limb circuit, VT can only be estimated by taking into account changes in flow and unintentional leaks (from the mask or from the mouth), assuming that the intentional leak is known. For most ventilators, built-in software underestimates VT and this underestimation is little affected by leaks. Conversely, higher pressure support increases underestimation of VT [5, 6]. Sogo et al. [7] developed a bench model presented as more representative of clinical leaks by inducing random dynamic leaks during inspiratory or expiratory phases. Unlike previous studies, the authors found that the four ventilators tested significantly overestimated VT (with differences ranging from 18 % ± 7 % to 36 % ± 18 %) suggesting that a portion of the identified leak was erroneously considered by the software as volume delivered to the patient. The inaccuracy in VT estimation has direct clinical implications: commercial software can unpredictably either underestimate or overestimate VT. For these reasons, clinicians should minimize unintentional leaks by adjusting mask fit or changing mask type or ventilator settings. Once leaks have been corrected, clinicians must remain aware of differences in estimation of VT between ventilators and not rely only on information provided by ventilator software to monitor efficacy of NIV.
Fig. 8.3
Flow and leaks during NIV with a bi-level pressure support ventilator (single-tube system and nasal mask vented)
8.4 Leaks
Unintentional leaks are major contributors to NIV intolerance, patient-ventilator asynchrony, suboptimal correction of ABGs, and nocturnal hypoventilation. Estimation of leaks by the ventilator – if reliable – is a useful contribution to NIV monitoring.
Rabec et al. [8] showed that leaks assessed by built-in software of the VPAPTM III-ResLinkTM (ResMed, North Ryde, Australia) ventilators were highly correlated with bench test measurements. These results cannot, however, be extrapolated to all home bi-level ventilators because bench testing of different commercially available home ventilators has demonstrated important discrepancies in leak estimation between devices [5–7]. One important caveat is that devices do not all report estimations of leaks in the same way. For instance, leaks are reported either as an estimation of unintentional leaks or as an estimation of total leaks (i.e., leaks through mask exhalation valves plus unintentional leaks) (Fig. 8.3). Physicians monitoring patients on home NIV should therefore be aware of these differences. Manufacturers have determined an arbitrary threshold for leaks below which pressurization is considered effective. In case of major leaks, the leak compensation may be insufficient and impair efficacy of ventilation, as shown in Fig. 8.4 [8]. Conversely, thresholds reported by manufacturers are not necessarily relevant, inasmuch as recent home ventilators have a high capacity for leak compensation.
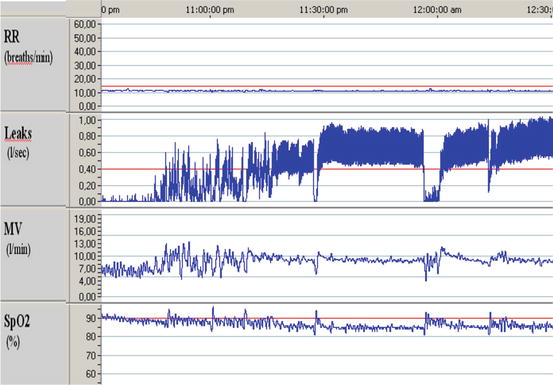
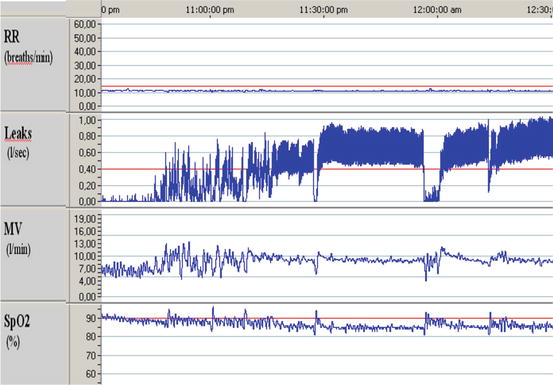
Fig. 8.4




VPAP-Reslink™ characteristic tracing showing – from top to bottom – respiratory rate, leaks (unintentional leaks in liters/second), minute ventilation, and SpO2. Important unintentional leaks (>0.4 l/s) are associated with a prolonged decrease in SpO2 directly measured by the device’s pulse oximetry module (Adapted from Ref. [8])
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


