Chapter 16 Sleep
 During normal sleep tidal volume is reduced, with maximal reduction in ventilation occurring during rapid eye movement sleep when breathing also becomes irregular.
During normal sleep tidal volume is reduced, with maximal reduction in ventilation occurring during rapid eye movement sleep when breathing also becomes irregular. Reduction in the speed and strength of pharyngeal muscle reflexes causes increased airways resistance, leading to snoring in many normal individuals.
Reduction in the speed and strength of pharyngeal muscle reflexes causes increased airways resistance, leading to snoring in many normal individuals.Normal Sleep
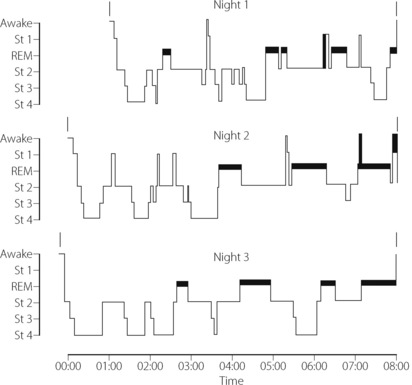
The stage of sleep changes frequently during the night, and the pattern varies between different individuals and on different nights for the same individual (Figure 16.1). Sleep is entered in stage 1 and usually progresses through 2 to 3 and sometimes into 4. Episodes of REM sleep alternate with non-REM sleep throughout the night. On average there are four or five episodes of REM sleep per night, with a tendency for the duration of the episodes to increase towards morning. Conversely, stages 3 and 4 predominate in the early part of the night.
Respiratory Changes
Ventilation.1 Tidal volume decreases with deepening levels of non-REM sleep and is minimal in REM sleep, when it is about 25% less than in the awake state. Respiratory frequency is generally unchanged, though breathing is normally irregular during REM sleep. Minute volume is progressively reduced in parallel with the tidal volume. These changes in ventilation are brought about by the same neurochemical changes that cause sleep. Increased activity of GABA secreting neurones during sleep has a direct depressant effect on the respiratory centre (see Figure 5.4) and activation of cholinergic neurones is thought to be responsible for the respiratory patterns seen during non-REM sleep.1
Arterial Pco2 is usually slightly elevated by about 0.4 kPa (3 mmHg). In the young healthy adult, arterial Po2 decreases by about the same amount as the Pco2 is increased, and therefore the oxygen saturation remains reasonably normal. Mean value for rib cage contribution to breathing (page 87) was found to be 54% in stage 1–2, decreasing slightly in stages 3–4.2 However, in REM sleep, the value was reduced to 29%, which is close to the normal awake value in the supine position.
Chemosensitivity. In humans, the slope of the hypercapnic and hypoxic ventilatory responses are markedly reduced during sleep.3,4 In both cases, the slope is reduced by approximately one-third during non-REM sleep, and even further reduced during REM sleep, but fortunately the responses are never abolished completely.
Effect of age. Compared with young subjects, the elderly have more variable ventilatory patterns when awake, which seems to result in more episodes of periodic breathing (page 76) and apnoea when asleep. Elderly subjects also have significant oscillations in upper airway resistance during sleep (see below),5 which may contribute to the observed variations in ventilation. Thus as age advances, episodes of transient hypoxaemia occur in subjects who are otherwise healthy, with saturations commonly falling as low as 75% during sleep. Such changes must be regarded as a normal part of the ageing process.
Pharyngeal airway resistance. Air flow through the sharp bends of the upper airway is normally laminar, but is believed to be very close to becoming turbulent even in normal subjects.6 Pharyngeal muscles may play a crucial role in maintaining the optimum shape of the airway to maintain laminar flow, and the speed at which these control mechanisms can respond to changes in pharyngeal pressure (page 83) may be more critical than previously thought.7 Any condition that attenuates or delays these reflexes even slightly, such as sleep or alcohol ingestion, will then have a major effect on airflow in the pharynx causing breakdown of the normally laminar flow.
The nasal airway is normally used during sleep, and upper airway resistance is consistently increased, especially during inspiration and in REM sleep. The main sites of increase are across the soft palate and in the hypopharynx.8 Changes in pharyngeal muscle activity with sleep are complex. Muscles with predominantly tonic activity, such as tensor palati, show a progressive decrease in activity with deepening non-REM sleep,9 reaching only 20–30% of awake activity in stage 4 sleep. This loss of tonic activity correlates very well with increased upper airway resistance.9 Unlike in the awake state, tensor palati also fails to respond to an inspiratory resistive load. The activity of muscles with predominantly phasic inspiratory activity (e.g. geniohyoid and genioglossus) are influenced little by non-REM sleep. In spite of maintained phasic activity during non-REM sleep, tonic activity of geniohyoid is reduced whilst that of genioglossus is well preserved, and responds appropriately to resistive loading.10 During REM sleep genioglossus activity is reduced.11 It thus appears that the major effect is upon the tonic activity of nasopharyngeal muscles and the increase in hypopharyngeal resistance seems to be due to secondary downstream collapse.
The ventilatory response to increased airway resistance is important in normal sleep because of the increased pharyngeal resistance, and is generally well preserved. There are substantial and rapid increases in both diaphragmatic and genioglossal inspiratory activity following nasal occlusion in normal sleeping adults.12
Snoring
Snoring may occur at any age, but the incidence is bimodal, peaking in the first and the fifth to sixth decades of life. It is commoner in males than females, and linked to obesity. It may occur in any stage of sleep, becoming more pronounced as non-REM sleep deepens, though usually attenuated in REM sleep. As may be expected, snoring is less severe when sleeping in the lateral rather than supine position.13 About one-quarter of the population are habitual snorers, but these vary from the occasional snorer (e.g. after alcohol or with an upper respiratory tract infection) to the habitual persistent and heavy snorer.
Snoring originates in the oropharynx and in its mildest form is due to vibration of the soft palate and posterior pillars of the fauces. However, in its more severe forms, during inspiration the walls of the oropharynx collapse and the tongue is drawn back as a result of the subatmospheric pressure generated during inspiration against more upstream airway obstruction. This may be at the level of the palate as described above or may be the result of nasal polyps, nasal infection or enlarged adenoids, which are the commonest cause of snoring in children.14 As obstruction develops, the inspiratory muscles greatly augment their action and intrathoracic pressure may fall as low as −7 kPa (−70 cmH2O).
‘Normal’ snoring is not associated with either frequent arousal from sleep or apnoea, but is believed to precede the development of more serious sleep-related breathing disorders, with both increasing age and obesity making this progression more likely.15
Sleep-Disordered Breathing16
This term is used to describe a continuum of respiratory abnormalities seen during sleep, which affect around 20% of the population16 and range from simple snoring to life-threatening obstructive sleep apnoea.17,18,19 All are characterised by periods of apnoea, with or without episodes of airway narrowing or obstruction, that lead to repeated episodes of arterial hypoxia and arousal from sleep. Repeated arousals throughout the night give rise to excessive daytime sleepiness. Four syndromes are described, but there is considerable overlap between them:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree