Sinus Arrhythmias
Overview
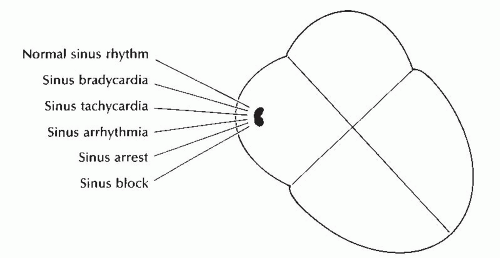
The term arrhythmia (also called dysrhythmia) is very general, referring to all rhythms other than the normal rhythm of the heart (normal sinus rhythm). Sinus arrhythmias (Figure 6-1) result from disturbances in impulse discharge or impulse conduction from the sinus node. The sinus node retains its role as pacemaker of the heart, but discharges impulses too fast (sinus tachycardia) or too slow (sinus bradycardia); discharges impulses irregularly (sinus arrhythmia); fails to discharge an impulse (sinus arrest); or the impulse discharged is blocked as it exits the sinoatrial (SA) node (SA exit block). Sinus bradycardia, sinus tachycardia, sinus arrhythmia, sinus arrest, and sinus block are all considered arrhythmias. However, sinus bradycardia at rest, sinus tachycardia with exercise, and sinus arrhythmia associated with the phases of respiration are considered normal responses of the heart.
Normal sinus rhythm
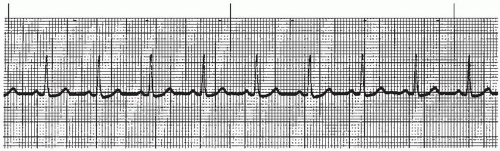
Normal sinus rhythm (Figure 6-2 and Box 6-1) reflects the heart’s normal electrical activity. The SA node normally initiates impulses at a rate of 60 to 100 beats per minute. Since this rate is faster than other pacemaker sites in the conduction system, the SA node retains control as the primary pacemaker of the heart. Sinus rhythm originates in the SA node and the impulse follows the normal conduction pathway through the atria, the AV node, the bundle branches, and the ventricles, resulting in normal atrial and ventricular depolarization.
Box 6-1. Normal sinus rhythm: Identifying ECG features
Rhythm: Regular
Rate: 60 to 100 beats/minute
P waves: Normal in size, shape, and direction; positive in lead II; one P wave precedes each QRS complex
PR interval: Normal (0.12 to 0.20 second)
QRS complex: Normal (0.10 second or less)
Normal sinus rhythm is regular with a heart rate between 60 and 100 beats per minute. The P waves are normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex is within
normal limits. Normal sinus rhythm is the normal rhythm of the heart. No treatment is indicated.
normal limits. Normal sinus rhythm is the normal rhythm of the heart. No treatment is indicated.
Sinus tachycardia
Sinus tachycardia (Figure 6-3 and Box 6-2) is a rhythm that originates in the sinus node and discharges impulses regularly at a rate between 100 and 160 beats per minute. The P waves are normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex is within normal limits. The distinguishing feature of this rhythm is the sinus origin and the rate between 100 and 160 beats per minute.
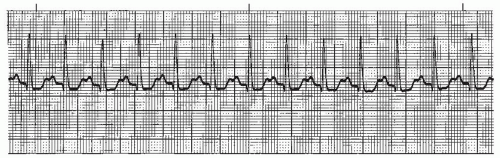 Figure 6-3. Sinus tachycardia. Rhythm: Regular Rate: 115 beats/minute P waves: Sinus PR interval: 0.16 to 0.18 second QRS complex: 0.08 to 0.10 second. |
Box 6-2. Sinus tachycardia: Identifying ECG features
Rhythm: Regular
Rate: 100 to 160 beats/minute
P waves: Normal in size, shape, and direction; positive in lead II; one P wave precedes each QRS complex
PR interval: Normal (0.12 to 0.20 second)
QRS complex: Normal (0.10 second or less)
Sinus tachycardia is the normal response of the heart to the body’s demand for an increase in blood flow (for example, exercise). The sinus node increases its rate in response to an increased need. When needs decrease, the
heart rate slows down. Sinus tachycardia begins and ends gradually in contrast to other tachycardias, which begin and end suddenly.
heart rate slows down. Sinus tachycardia begins and ends gradually in contrast to other tachycardias, which begin and end suddenly.
Sinus tachycardia can be caused by anything that increases sympathetic tone or anything that decreases parasympathetic tone. Factors commonly associated with sinus tachycardia are:
anxiety, excitement, stress, exertion, exercise
fever, anemia, shock
hypoxia, hypovolemia, hypotension, heart failure, hyperthyroidism
pain, pulmonary embolism (sinus tachycardia is the most common arrhythmia seen with pulmonary embolism)
myocardial ischemia, myocardial infarction (MI) (sinus tachycardia persisting after an acute infarct implies extensive heart damage and is generally a bad prognostic sign)
drugs that increase sympathetic tone (epinephrine, norepinephrine, dopamine, dobutamine, tricyclic antidepressants, isoproterenol, and nitroprusside)
drugs that decrease parasympathetic tone (atropine)
use of substances such as caffeine, cocaine, and nicotine.
Sinus tachycardia is usually a benign arrhythmia and treatment is directed at correcting the underlying cause (relief of pain, fluid replacement, removal of offending medications or substances, and reducing fever or anxiety). However, persistent sinus tachycardia should never be ignored in any patient, especially the cardiac patient. A rapid heart rate increases the workload of the heart and its oxygen requirements and may cause a decreased stroke volume leading to a decrease in cardiac output. In addition, heart rates higher than normal decrease the amount of time the heart spends in diastole, leading to a decrease in coronary artery perfusion (coronary arteries are perfused during diastole). Sinus tachycardia that persists may be one of the first signs of early heart failure.
Sinus bradycardia
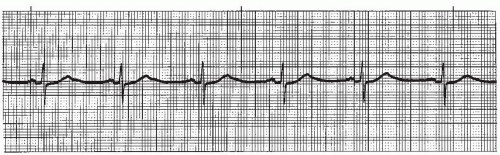
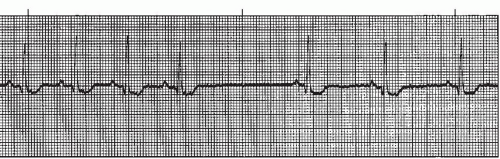
Sinus bradycardia (Figure 6-4 and Box 6-3) is a rhythm that originates in the SA node and discharges impulses regularly at a rate between 40 and 60 beats per minute. The P waves are normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex is within normal limits. The distinguishing feature of this rhythm is the sinus origin and a heart rate between 40 and 60 beats per minute.
Box 6-3. Sinus bradycardia: Identifying ECG features
Rhythm: Regular
Rate: 40 to 60 beats/minute
P waves: Normal in size, shape, and direction; positive in lead II; one P wave precedes each QRS complex
PR interval: Normal (0.12 to 0.20 second)
QRS complex: Normal (0.10 second or less)
Sinus bradycardia is the normal response of the heart to relaxation or sleeping when the parasympathetic effect on cardiac automaticity dominates over the sympathetic effect. It’s common among trained athletes who may have a resting or sleeping pulse rate as low as 35 beats per minute. Mild bradycardia may actually be beneficial in some patients (for example, acute MI) because of the decrease in workload on the heart.
Sinus bradycardia can be caused by anything that increases parasympathetic tone or anything that decreases sympathetic tone. It commonly occurs with the following:
during sleep and in athletes
in acute inferior wall MI involving the right coronary artery, which usually supplies blood to the SA node
as a reperfusion rhythm after coronary angioplasty or after treatment with thrombolytics
vagal stimulation from vomiting, bearing down (Valsalva’s maneuver), or carotid sinus pressure
as a vasovagal reaction. A vasovagal reaction is an extreme body response that causes a marked decrease in heart rate (due to vagal stimulation) and a marked decrease in blood pressure (due to vasodilation). This reaction may occur with pain, nausea, vomiting, fright, or sudden stressful situations. The combination of extreme bradycardia and hypotension may result in fainting (vasovagal syncope). The situation is usually reversed when the individual is placed into a recumbent position, thereby increasing venous return to the heart. If fainting occurs with the individual in a recumbent position, it can usually be reversed with leg elevation.
carotid sinus hypersensitivity syndrome, sleep apnea
decreased metabolic rate (hypothyroidism, hypothermia); hyperkalemia
sudden movement from recumbent to an upright position (common in the elderly)
increased intracranial pressure (a sudden appearance of sinus bradycardia in a patient with cerebral edema or subdural hematoma is an important clinical observation)
drugs such as digoxin, calcium channel blockers, and beta blockers
degenerative disease of the sinus node (sick sinus syndrome). Persistent sinus bradycardia is the most common and often the earliest manifestation of sick sinus syndrome. Sick sinus syndrome is a dysfunctioning sinus node, which is manifested on the ECG by marked bradyarrhythmias alternating with episodes of tachyarrhythmias and is commonly accompanied by symptoms such as dizziness, fainting episodes, chest pain, shortness of breath, and heart failure. This syndrome has also been called tachybrady syndrome. Permanent pacemaker implantation is recommended once patients become symptomatic.
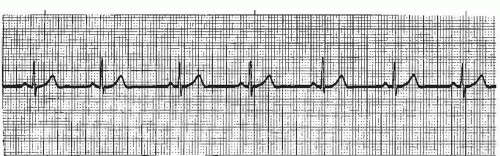 Figure 6-5. Sinus arrhythmia Rhythm: Irregular Rate: 60 beats/minute P waves: Normal in configuration; precede each QRS PR interval: 0.12 to 0.14 second QRS complex: 0.06 to 0.08 second |
Sinus bradycardia doesn’t require treatment unless the patient becomes symptomatic. Some clinical signs and symptoms requiring treatment include cold, clammy skin; hypotension; shortness of breath, chest pain, changes in mental status, decrease in urine output, and heart failure. If sinus bradycardia persists, the treatment of choice is atropine, a drug that increases the heart rate by decreasing parasympathetic tone. The usual dose is 0.5 mg IV push every 5 minutes until the bradycardia is resolved or a maximum dose of 3 mg is given. Atropine must be administered correctly; atropine administered too slowly or in doses less than 0.5 mg can further decrease the heart rate instead of increasing it. If the rhythm still doesn’t resolve after the atropine is administered, a transcutaneous (external) or transvenous pacemaker may be needed. All medications that cause a decrease in heart rate should be reviewed and discontinued if indicated. For chronic bradycardia, permanent pacing may be indicated.
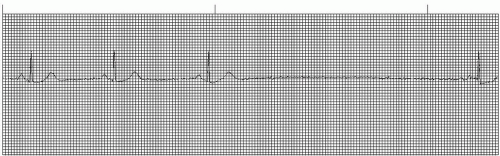
Sinus arrhythmia
Sinus arrhythmia (Figure 6-5 and Box 6-4) is a rhythm that originates in the sinus node and discharges impulses irregularly. The heart rate may be normal (60 to 100 beats per minute) or slow (commonly associated with a bradycardic
rate). The P waves are normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex is within normal limits. The distinguishing feature of this rhythm is the sinus origin and the rhythm irregularity.
rate). The P waves are normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex is within normal limits. The distinguishing feature of this rhythm is the sinus origin and the rhythm irregularity.
Box 6-4. Sinus arrhythmia: Identifying ECG features
Rhythm: Irregular
Rate: Normal (60 to 100 beats/minute) or slow (less than 60 beats/minute)
P waves: Normal in size, shape, and direction; positive in lead II; one P wave precedes each QRS complex
PR interval: Normal (0.12 to 0.20 second)
QRS complex: Normal (0.10 second or less)
Sinus arrhythmia is commonly associated with the phases of respiration. During inspiration, the sinus node fires faster; during expiration, it slows down. This rhythm is an extremely common finding among infants, children, and young adults, but may occur in any age-group. Sinus arrhythmia is a normal phenomenon that usually doesn’t require treatment unless it is accompanied by a bradycardia rate that causes symptoms.
Sinus pause (sinus arrest and sinus exit block)
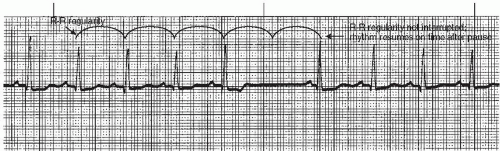
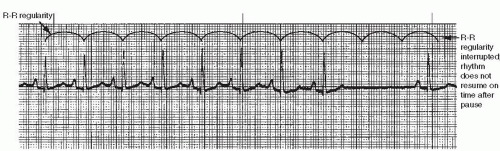
Sinus pause is a broad term used to describe rhythms in which there is a sudden failure of the SA node to initiate or conduct an impulse. Two rhythms fall under this category: sinus arrest and sinus exit block. Sinus arrest and sinus exit block, two separate arrhythmias with different pathophysiologies (Figures 6-6, 6-7, and 6-8 and Box 6-5), are discussed together because distinguishing between them is at times difficult, and because their treatment and clinical significance are the same.
Box 6-5. Sinus arrest and sinus exit block: Identifying
ECG features
Rhythm: Basic rhythm usually regular; there is a sudden pause in the basic rhythm (causing irregularity) with one or more missing beats; heart rate may slow down for several beats after pause (temporary rate suppression) but returns to basic rate
Rhythm: Basic rhythm usually regular; there is a sudden pause in the basic rhythm (causing irregularity) with one or more missing beats; heart rate may slow down for several beats after pause (temporary rate suppression) but returns to basic rate
Rate: That of underlying rhythm, usually sinus
P waves: Sinus P waves with basic rhythm; absent during pause
PR interval: Normal (0.12 to 0.20 second) with basic rhythm; absent during pause
QRS complex: Normal (0.10 second or less) with basic rhythm; absent during pause
Differentiating features
Sinus block: Basic rhythm (R-R regularity) resumes on time after pause
Sinus arrest: Basic rhythm (R-R regularity) doesn’t resume on time after pause
Both sinus arrest and sinus exit block originate in the sinus node and are characterized by a sudden pause in the sinus rhythm in which one or more beats (cardiac cycles)
are missing. The P waves in the underlying rhythm will be normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex in the underlying rhythm is within normal limits. The distinguishing feature of both rhythms is the abrupt pause in the underlying sinus rhythm in which one or more beats are missing, followed by a resumption of the basic rhythm after the pause.
are missing. The P waves in the underlying rhythm will be normal in size, shape, and direction; positive in lead II (a positive lead), with one P wave preceding each QRS complex. The duration of the PR interval and the QRS complex in the underlying rhythm is within normal limits. The distinguishing feature of both rhythms is the abrupt pause in the underlying sinus rhythm in which one or more beats are missing, followed by a resumption of the basic rhythm after the pause.
Sinus arrest is caused by a failure of the SA node to initiate an impulse and is therefore a disorder of automaticity. This failure in the automaticity of the SA node upsets the timing of the sinus node discharge, and the underlying rhythm won’t resume on time after the pause.
With sinus exit block, an electrical impulse is initiated by the SA node, but is blocked as it exits the sinus node, preventing conduction of the impulse to the atria. Thus, SA exit block is a disorder of conductivity. Because the regularity of the sinus node discharge isn’t interrupted (just blocked), the underlying rhythm will resume on time after the pause. Once the rhythm resumes after the pause (in both sinus arrest and sinus exit block) it’s common for the rate to be slower for several cycles (rate suppression). Rate
suppression is temporary and will cause a brief irregularity in the underlying rhythm, but after several cycles the basic rate and rhythm will return. An example of rate suppression is shown in Figure 6-8.
suppression is temporary and will cause a brief irregularity in the underlying rhythm, but after several cycles the basic rate and rhythm will return. An example of rate suppression is shown in Figure 6-8.
Differentiating between the two rhythms involves comparing the length of the pause with the underlying P-P or R-R interval to determine if the underlying rhythm resumes on time after the pause. This can be determined only if the underlying rhythm is regular. If the underlying rhythm is irregular, as in sinus arrhythmia (Figure 6-9), it’s impossible to distinguish sinus arrest from sinus exit block. In this case, the rhythm would best be interpreted using the broad term sinus pause, indicating that either rhythm could be present. From a clinical viewpoint, distinguishing between sinus arrest and sinus exit block usually isn’t essential.
Sinus arrest or sinus exit block can be caused by numerous factors, including:
increase in vagal (parasympathetic) tone on the SA node
myocardial ischemia or infarction
use of certain drugs such as digoxin, beta blockers, or calcium channel blockers.
The patient may become symptomatic if the pauses associated with sinus arrest or sinus exit block are frequent or prolonged. Another danger is that the SA node may lose pacemaker control. When the sinus node slows down below its minimum firing rate of 60 beats per minute because of bradycardia or a pause in the underlying rhythm, an opportunity is provided for pacemaker cells in other areas of the conduction system to usurp control from the sinus node and become the dominant pacemaker of the heart. The term ectopic is commonly applied to rhythms that originate from any site other than the SA node. Ectopic sites in the atria, AV node, or ventricles may assume pacemaker control for one beat, several beats, or continuously.
If symptomatic, the rhythm is treated the same as in symptomatic sinus bradycardia. In addition, all medications that depress sinus node discharge or conduction should be stopped.
A summary of the identifying ECG features of sinus arrhythmias can be found in Table 6-1.
Table 6-1. Sinus arrhythmias: Summary of identifying ECG features | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|