Component
Catheterization laboratory
Intensive care unit/ECMO Care
Cardiac operating room
Personnel
Catheterizer
Intensivist
Surgeon
Catheter technician
Surgeon
Assistant surgeon
Anesthesiologist
Nurse
Anesthesiologist
Nurse
Respiratory therapist
Scrub nurse
Trainees
ECMO specialist/perfusionist
Circulating nurse
Surgeon (for hybrid procedures)
Trainees
Perfusionist
Consultants
Trainees
Echocardiographer
Equipment
Fluoroscopy equipment
ECMO circuit
CPB Circuit
Fixed catheterization table
Resuscitation carts
Anesthesia machine
Instrument table
Surgical instrument table
Minimally invasive equipment
Surgical instruments (for hybrid procedures)
Surgical equipment (cautery, headlamp, etc.)
Echocardiography machine
Clinical/systems
Rapidly changing physiology
Multiple patients
Time pressures on CPB
Radiation exposure
Bed-availability issues
High level technical skills
Multiple equipment changes (catheters)
Blended teams
Hierarchy of personnel
Communication between control room and lab
Hierarchy of personnel
High level technical skills
Hierarchy of personnel
The Bristol Royal Infirmary Inquiry and the Manitoba Pediatric Cardiac Surgery Inquest, two highly publicized investigations of mortality in pediatric cardiac surgery, provided strong evidence that the deaths were related not only to surgical errors but to systems failures and poor communication as well [4, 5]. Subsequent rigorous human factors research has shown that errors are common in the realm of pediatric cardiac surgery. Direct observation of 102 pediatric cardiac surgery cases found a median of 1.1 major (potential to cause serious consequences) safety events and 18.3 minor events per case [6]. A multicenter study using direct observation of arterial switch operations reported that mortality and “near misses” were linked most strongly to major events but that minor events also increased the odds of death and that the impact of minor events was additive [7]. In the study by Barach et al., minor events most commonly represented communication errors [6]. Likewise, cardiac surgery teams with more effective teamwork strategies, including better communication, had fewer minor intraoperative events, improved intraoperative performance, and reduced operative times [3].
The literature also supports the pervasive nature of medical errors in the intensive care unit—an environment comprised of a multitude of technologies, large interdisciplinary provider teams, critically ill patients, high emotionality, and fatiguing work schedules—and the relevance of human error and systems failures [8, 9]. In around-the-clock direct patient and provider observations in an ICU, Donchin et al. identified an average of 1.7 errors per patient per day, 30 % of which could have led to marked deterioration in patient status or death without prompt recognition and management [10]. In pediatrics, a multicenter chart review of 15 ICUs documented 1,488 adverse events among 734 patients, with 62 % of patients suffering at least one adverse event, 45 % of which were classified as preventable [11]. Furthermore, analysis of errors and adverse events in the ICU showed lack of teamwork and communication to be major contributors to nearly half of critical incidents [12, 13].
Both in and out of the operating room, effective teamwork behaviors have been linked to positive outcomes. For instance, during both simulated and real resuscitations, factors such as effective leadership have a positive impact [14–16]. The ability of the leader to organize a team, avoid “task fixation,” and articulate a global assessment of the patient’s status and plans for management was associated with improved performance measures, such as hands-on time when providing chest compressions and time to defibrillation after recognizing ventricular fibrillation. These performance measures are clinically important, given that early defibrillation and increased CPR fraction are associated with improved survival after cardiac arrest [17–19]. The importance of specific teamwork skills has been acknowledged in recent resuscitation guidelines from the American Heart Association, including the Pediatric Advanced Life Support Guidelines [20]. Thus, incorporating multidisciplinary teamwork training across the cardiovascular care environment may help decrease preventable non-technical errors and improve patient outcomes.
The contribution of human factors to catastrophic accidents and failures in non-medical high-risk industries, including nuclear power and aviation, has long been recognized, and substantial efforts have gone towards training staff in principles of teamwork to mitigate the effects of human error in non-technical skills. After analyzing a series of catastrophic accidents, the aviation industry turned to simulation-based teamwork training, in the form of “Crew Resource Management” Training, to overcome non-technical errors and improve teamwork. Crew Resource Management Training has now become a mandatory component of initial pilot licensure and maintenance of certification. In this training, highly realistic flight simulators are utilized to recreate emergency scenarios that the crew might encounter in flight, and post-simulation debriefings led by trained facilitators focus on teamwork principles.
Given the parallels between aviation and medicine in terms of the contribution of human factors to errors and accidents, the lessons from the aviation industry were transferred to medical training through the introduction of simulation-based Crisis Resource Management (CRM) Training. Indeed, since the introduction of immersive simulation in medicine in the 1980s [21], simulation has been applied broadly throughout acute care areas [22–24], not only for teamwork training but also for clinical skills training, competency assessment, and systems evaluation to identify latent safety threats at the point of care delivery.
Simulation training is particularly important in pediatric subspecialties, where high-risk events, such as cardiopulmonary arrest, are relatively rare, creating a “pediatric training paradox” [25]. Low numbers of training opportunities can result in an unfavorable “volume-outcome relationship” that may render providers ill-prepared to conduct pediatric resuscitation [26–28]. This effect is magnified in the field of pediatric cardiovascular care, where specific resuscitation skills, such as emergent chest re-opening, temporary epicardial pacing, and ECMO cannulation, fall outside the scope of traditional pediatric advanced life support training [29–32]. Additionally, work hour restrictions and societal expectations that senior physicians be involved at the bedside limit trainees’ clinical experience and opportunities and may delay acquisition of full proficiency before training is completed. Simulation offers unique solutions to this challenge in pediatric cardiovascular training through authentic on-demand, structured experiences combined with opportunities for summative and formative feedback. As a result, simulation is beginning to be applied across the spectrum of cardiovascular care—from the intensive care unit [29], to the catheterization laboratory [33], to the operating room [34].
Simulation for Team Training in Cardiovascular Care: Principles and Evidence
In the early 1980s, an early precursor to today’s high fidelity, whole-body mannequin simulators was developed by David Gaba and colleagues at Stanford University. The simulator interacted with monitors and anesthesia equipment to realistically replicate patient physiology as part of an immersive simulation environment (CASE, Comprehensive Anesthesia Simulator Environment) in which participants were able to engage in real-time clinical problem solving [35]. Gaba’s early work in anesthesia was unique in medicine in its recognition of the importance of human factors in the operating room [36]. He and others [37] defined standards of leadership and team behavior now described as the principles of Crisis Resource Management (CRM). These principles have since been widely adopted in training programs across acute care, including the emergency department [38], intensive care unit [29, 39], and operating room [40]. Likewise, a growing number of simulation-based CRM training programs applied to pediatric cardiac critical care have been shown to improve the comfort level of providers in navigating critical incidents [29, 30, 33].
Principles of Crisis Resource Management address issues related to event leadership, followership, communication, and team coordination (Table 35.2).
Table 35.2
Fundamental principles of crisis resource management training
Principle | Key components |
|---|---|
Role clarity | Event manager is explicitly identified |
Task assignments are clear | |
Communication | Names and eye contact are used between speaker and listener |
Closed loop (receiver confirms understanding sender) | |
Communication is explicit (no “hints”) | |
Communication is channeled through the event manager | |
Updates on task progress are given often | |
Communication is respectful | |
Personnel support | Support personnel/consultants are mobilized appropriately |
Resource utilization | Equipment and resources are mobilized appropriately |
Hospital emergency protocols and procedures are followed | |
Global assessment | The “50,000-foot view” is maintained by event manager throughout |
Fixation on one aspect of the task at the expense of other aspects avoided | |
Event manager frequently updates team on progress | |
An environment of psychological safety is maintained | |
Input from the team is invited |
1.
Role Clarity. Team members are assigned to specific tasks and responsibilities. Key to these are the “Event Manager” who organizes the team by assigning tasks, controlling communication, creating a shared mental model through frequent updates and maintaining global perspective on the evolving crisis. Effective Event Managers support an environment of psychological safety to promote free and effective communication [41].
2.
Communication. Effective communication strategies emphasize clear and explicit statements directed to specific individuals combined with consistent “closed-loop” communication (in which the listener confirms an understanding of the speaker’s message) and in which team members provide updates on assigned tasks as well as offering information and suggestions to the event manager—all of which occur across authority gradients.
3.
Global Assessment. The “50,000-foot view,” or situational awareness, of the entire event and environment is maintained to avoid “fixation errors,” in which participants focus on one aspect of the event at the expense of other relevant events. Strategies include provision of frequent updates by the Event Manager and team-based review of clinical status.
4.
Personnel Support. Proactively identifying and mobilizing additional resources, including expert consultants (i.e., “Calling for help early”).
5.
Resource Utilization. The use of systematic and institutional resources for critical event management is optimized. This issue includes understanding human and technical resource availability and operations and is supported by a working knowledge of current hospital policy and procedure.
Crisis Resource Management courses, once exclusively delivered at stand-alone centers, are now more frequently being applied directly to the point at which clinical care is delivered. Such in-situ or point-of-care simulations allow full native teams to train within their own complex care environments [42]. In the cardiac operating room and catheterization laboratory in particular, in situ training programs can optimize authenticity, realism, and engagement by including inherent environmental nuances that might otherwise be difficult to recreate (Fig. 35.1). In the catheterization laboratory, for instance, resuscitation efforts may be hampered by the dark environment and bulky fluoroscopy equipment that may obstruct access to the patient and challenge communication between team members. In addition, the ongoing need for fluoroscopy during resuscitation poses the threat of exposure to ionizing radiation to caregivers, underscoring team member safety during the resuscitation process.


Fig. 35.1
Team Training at the Point of Delivery in Pediatric Cardiovascular Care. Native team training within native environments incorporates preparedness training into the daily workflow. Participation of complete compliment of care providers during high-fidelity simulation courses in the highly nuanced environments, such as the cardiothoracic operating room (a, b) and the catheterization Laboratory (c, d)
Crisis Resource Management training holds both the intuitive appeal of a practice-makes-perfect model, as well as a rapidly growing literature of effectiveness at multiple levels, including (1) knowledge acquisition, (2) team-based elements, (3) behavioral processes (measures of communication, self-correction, etc.), (4) performance outcomes, and (5) translation to patient care. Applied to pediatric cardiac ICU, CRM training can increase self-efficacy, preparedness, and comfort for participants [29, 30, 32].
Although data specific to patient outcomes in pediatric cardiovascular care may be lacking, a growing literature base from other pediatric acute-care specialties suggests that CRM training substantially improves patient outcomes. In neonatology, trainees exposed to Neonatal Resuscitation Program training supplemented with high fidelity simulation practice, demonstrated more effective teamwork behavior, including information-sharing, updating the team on the patient’s status, and inquiry of other team members [39]. In the Emergency Room, team training reduces error rates [43]. A study from the Veterans Administration health care system found an 18 % reduction in annual mortality rates among centers in which formal team training programs were implemented compared to 7 % among those where team training was not introduced [44, 45]. Morbidity was likewise reduced in centers with formal team training programs [45]. In obstetrics, a field similar to pediatric cardiovascular care in that it relies heavily on resuscitation practices and skills outside of pediatric or advanced cardiac life support algorithms, Draycott et al. found clear links between effective utilization of teamwork principles and improved, more efficient care delivery, as well as patient outcomes. Particular team skills that correlated positively with outcomes included verbal declaration of a crisis, closed-loop communication, and effective resource utilization45, whereas clinical knowledge of management of obstetric emergencies, clinical skills in a simulator setting, or attitudes towards teamwork and patient safety were not correlated [46], suggesting that these factors alone are not sufficient for effective team performance. A decrease in the interval between diagnosis of cord prolapse and emergency cesarean delivery from 25 to 14.5 min (P < 0.001) after team training in a large UK maternity center further supports the value of CRM in improving care [47].
Simulation-Based Technical Skills Training in Pediatric Cardiovascular Care
Early applications of medical simulation focused on technical or clinical skills, and included trainers for endotracheal intubation [21], as well as the Harvey Cardiology Patient Simulator, developed in the late 1960s to teach cardiovascular examination skills [48, 49]. The efficacy of simulation-based procedural skills training has been established in several lines of inquiry related to acute care medicine. In one medical intensive care unit, simulation-based curricula regarding safe placement of central venous lines reduced the mean number of attempts (1.70 vs. 2.78, P = 0.04), failure rates (22.8–16.0 %, P = 0.02) and overall complication rates (32.9–22.9 %, P < 0.01) among trainees [50]. The curricula also reduced catheter-associated blood stream infections by 70 % and saved money [51].
Work hour restrictions, increased public scrutiny of clinical outcomes, and pressures to reduce operative times all threaten procedural “hands-on” time for trainees and, as a result, impact the quality of experiences to learn complex procedures [52]. Simulation-based skills training, both through analog and virtual reality models, has the ability to overcome these threats by providing dedicated hands-on practice time without harming patients. Simulation-based surgical training, such as virtual reality laparoscopic training, can improve skill acquisition through repetitive, deliberate practice combined with rigorous assessment and feedback [53, 54]. Additionally, a sole focus on teaching skills apart from actual patient care may create a less-threatening environment for the trainee and thereby enhance quality of teaching at the level of skills acquisition [55].
The pathway to procedural competency begins with acquisition of technical skills followed by the associated cognitive skills, including complex intraoperative decision making, communication, and the ability to adapt based on changing circumstances during a procedure. By deliberatively focusing on each element in order through well -designed curricula, simulation stands to accelerate the learning curve from novice to expert, and thus make the greatest educational use of real intraoperative time when ready [56]. These factors, combined with the development of integrated 6-year cardiothoracic surgery training programs [57] increasingly focused on competency-based training [58], have lead the field of adult cardiothoracic surgery to invest heavily in simulation-based curricula, relevant models, and assessment tools to teach technical skills [59, 60] that range from coronary anastomosis [61, 62], to mitral valve repair [63], to cardiopulmonary bypass management [64, 65].
Virtual reality simulators are also being used increasingly in invasive cardiology and electrophysiology, where they have accelerated learning among novices performing trans-septal puncture and diagnostic catheterization [33, 55] with associated reductions in fluoroscopy time [66]. Given the heterogeneous nature of congenital cardiac defects, the development of high fidelity simulation-based models for skills training has been slower than in adult cardiovascular fields, although our group has recently reported on the development of a highly realistic infant ECMO cannulation trainer (Fig. 35.2). Use of this trainer within the context of a full cannulation training curriculum improved cannulation time and a composite technical score that evaluates both the individual steps of cannulation, and patient management [67]. Engineering advances, such as three-dimensional (“rapid prototyping”) printers, have the potential to speed the development of pediatric-specific trainers by translating individual patient imaging data into highly realistic trainers that accurately replicate complex pediatric anatomy.
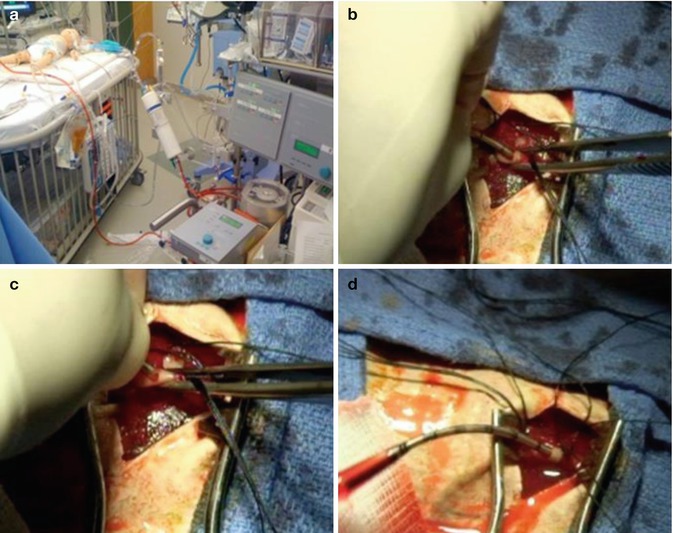
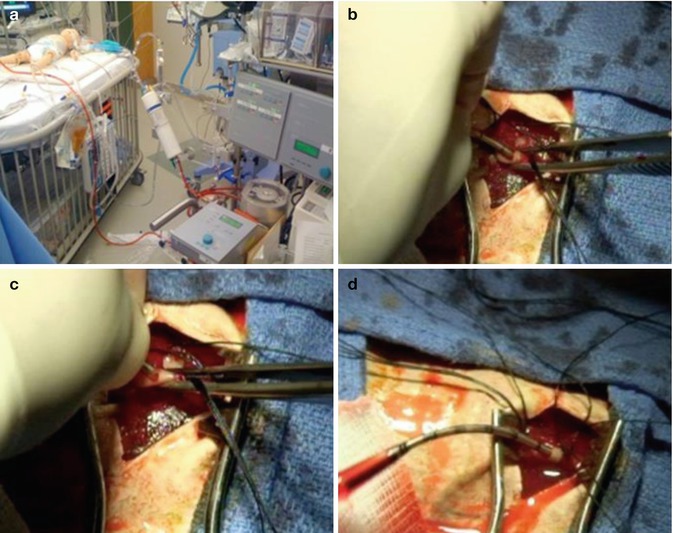
Fig. 35.2
The integrated ECMO cannulation skills trainer allows contextualized skills training for emergent ECMO cannulation during CPR. Contextualized skills training in the native cardiac intensive care unit environment (a) uses a highly realistic, embedded surgical skills trainer that allows dissection, vessel cannulation (b, c), and establishment of ECMO flow, and authentic “bleeding” from the surgical site (d) (Reprinted with permission from Allan et al. [67])
Point-of-Care Simulation to Enhance Systems Safety in Pediatric Cardiovascular Care
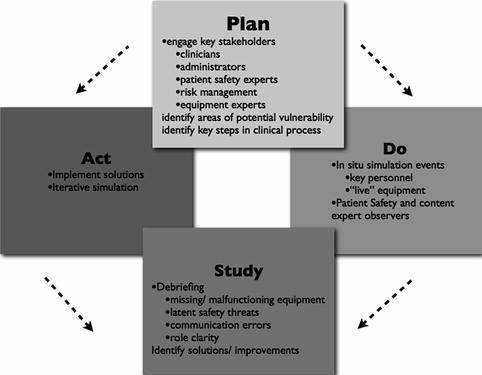
Simulation applied at the point of care offers opportunities not only to improve individual and team performance but also to study and improve the care system itself. Both in situ multidisciplinary team training programs [42, 68] and formalized simulation-based programs using rigorous human factors methodologies, such as “Lean [69]” or “Plan-Do-Study-Act (PDSA),” are now being employed as rapid-cycle-improvement methods to identify patient safety threats and to guide the design and implementation of system improvements [70]. Common factors among successful latent safety threat-analysis programs include (1) using expertise from multiple areas, including multidisciplinary clinical providers, simulation experts, risk management or systems safety experts, and equipment experts during planning, simulation, and debriefing; (2) a preparation phase to identify possible areas of vulnerability and key areas for testing and to clearly define steps in clinical processes when relevant; (3) iterative simulation events to identify safety threats and test changes implemented in reaction to identified threats; and (4) structured debriefing focusing not on individual performance but rather on identifying system deficiencies and generating solutions to threats [70] (Fig. 35.3).
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


