Pulmonary root dilation and valve regurgitation if translocated into the aortic position is frequently seen in children with transposition of the great arteries (TGA) after an arterial switch operation, as well as in patients after the Ross procedure. Many mechanisms are thought to be responsible for the progressive dilation. Despite the differences between the 2 groups, the similarity of having the pulmonary valve and its adjacent tissue working in the systemic circulation might have a comparable effect on the neoaortic root dimensions and elasticity. We prospectively recruited 52 patients with TGA, 23 Ross patients, and 48 healthy subjects for echocardiographic assessment of their aortic valve, root, sinutubular junction, and ascending aortic dimensions and elasticity. The data were compared, stratified by patient age at investigation and the duration of follow-up postoperatively. In relation to the healthy subjects, the neoaortic root dimensions were significantly larger and the tissue stiffer and less distensible in those with TGA and those who had undergone the Ross procedure. Although the pulmonary valve of the Ross patients had been under systemic pressure load for a significantly shorter period (4.4 ± 3.6 vs 10.1 ± 5.5 years), the dimensions and elasticity values had deteriorated more. These differences could neither be clearly attributed to the age differences at surgery or to an auxiliary congenital ventricular septal defect in those with TGA or the aortic valve phenotype before the Ross operation. In conclusion, the worse outcome of the neoaortic root dimensions and elasticity in the Ross patients should at least be partly related to the different predefined pulmonary artery structures and the different development of the normal and transposed pulmonary arteries.
Dilation of the pulmonary root in the aortic position and development of neoaortic regurgitation is a well-known problem in patients with transposition of the great arteries (TGA) after an arterial switch operation (ASO), as well as in patients after the Ross procedure, in which even dissection of the neoaortic root has been observed. Owing to the various underlying congenital problems, the procedures are profoundly different. In ASO, the valve stays in its previous position, and only the great arteries and coronary arteries are transposed. In the Ross procedure, especially with the widely used full root replacement technique, the entire valve, with the adjacent root tissue, is harvested and translocated to the aortic position. Again, the coronary arteries are reimplanted. The underlying morphologies and valve dysfunctions are also greatly different, which probably accounts for the different outcomes. Despite the obvious distinctions between the 2 groups, the similarity of having the pulmonary valve and its adjacent tissue working in the systemic circulation might have a comparable effect on the neoaortic root dimensions and elasticity. Distensibility reflects the condition of the vascular wall and is dependent directly on the valve dynamics. With these considerations, we measured the aortic dimensions and elasticity indexes in pediatric patients of both groups to gain additional insight into the consequences and their magnitude of influence on neoaortic root dilation.
Methods
The patients were selected through a review of the institutional pediatric cardiology and echocardiography database of the Pediatric Heart Center (Vienna, Austria). The inclusion criteria were age ≤18 years in both patient subgroups. Only isolated complete TGA corrected by single-stage ASO, including the Lecompte maneuver, with only additional ventricular septal defects and/or coarctations of the aorta, were accepted. Of the Ross patients, only those who had undergone the full root replacement technique and who had an underlying aortic valve defect such as congenital or acquired aortic stenosis or regurgitation (with or without coarctation of the aorta) without additional congenital heart defects were accepted. The exclusion criteria were genetic disorders such as Turner or Marfan syndrome in both cohorts. Of the 55 patients with TGA and 23 patients who had undergone the Ross procedure fulfilling these criteria, 52 with TGA and all 23 Ross patients were eligible for the present prospective echocardiographic investigation from February 2010 to September 2011. A cohort of 48 age-matching healthy patients with normal functioning tricuspid aortic valves who had been referred to our institution for routine checkups were prospectively recruited as controls. The institutional review board of the Vienna University Hospital committee on human research approved the study protocol. All patients or their relatives provided written informed consent, which was mandatory.
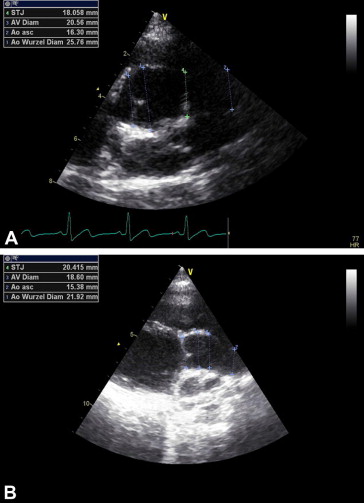
The echocardiographic assessment was performed with a Vivid E9 cardiovascular ultrasound system (GE Medical, Horton, Norway). The diameters of the aortic valve (AV), aortic root (AoR), sinutubular junction (STJ), and ascending aorta were measured perpendicular to the aortic flow in the parasternal long axis using the inner-edge to inner-edge method. Aortic valvular function was classified as being normal, stenotic, regurgitant, or combined by color and continuous wave Doppler measurements referring to the American Society of Echocardiography criteria. The z scores for inner edge to inner edge values were used to judge the degree of dilation of the aortic dimensions corresponding to body surface area. Compared to normal values, z scores ≥2 were considered dilated.
The elastic properties of the neoaortic root were gained using M-Mode imaging in the parasternal long axis view to measure off-line ≥5 to ≤15 systolic and diastolic diameters to calculate a mean value of the systolic and diastolic diameters (for schematic figure, see Pees and Michel-Behnke ). The blood pressure was measured simultaneously at the right forearm using a Philips SureSignsVS2 (Andover, Massachusetts). The stiffness index was calculated using the formula: aortic stiffness index = ln (SBP − DBP)/[(AoDS − AoDD)/AoDD)], where ln is the natural logarithm, SBP, the systolic blood pressure (mm Hg), DBP, the diastolic blood pressure (mm Hg), AoDS, the aortic diameter in systole (mm), and AoDD, the aortic diameter in diastole (mm).
For the distensibility calculations, 2 formulas were used. The first used the diameter and second, the area of the aortic root: aortic distensibility = 2(AoDS − AoDD)/[AoDD(SBP − DBP)] × 10 −3 [cm 2 ∙ dynes −1 × 10 −6 ]; and aortic distensibility = (AoAS − AoAD)/[AoAD(SBP − DBP) × 1,333] × 10 −7 [kPa −1 × 10 −3 ], where AoAS and AoAD are the aortic area in systole and diastole calculated using the formula: AoAS = π × (AoDS/2) 2 and AoAD = π × (AoDD/2) 2 , respectively.
Data analysis was performed with PASW Statistics, version 18.0 (SPSS, Chicago, Illinois). For continuous variables, Student’s t test was used, for nonparametric 2-way testing, the Mann-Whitney U test was used, and for >2 parameters, the Kruskal-Wallis test was used. The correlation structures were tested using the Pearson parametric correlation coefficient. Unless noted otherwise, values are given as the mean ± SD; p values <0.05 were considered statistically significant.
Results
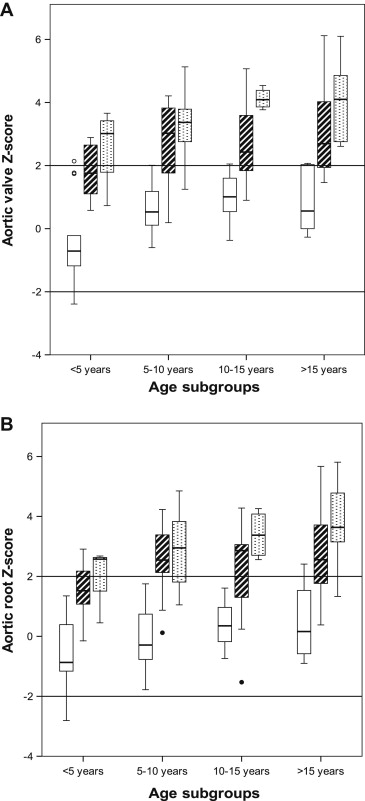
The demographic data are listed in Table 1 . As expected from the male predominance in TGA and congenital aortic valve diseases, statistically meaningful differences for this value were found. Significantly larger diameters and greater z scores were found in AV, AoR, STJ, and ascending aorta in patients after ASO than in the control subjects. Similarly, the elastic properties of the aortic root showed significantly stiffer and less distensible values in patients with TGA. Regarding the diameters of the neoaorta, the Ross patients presented with the greatest values and z scores for all, except the ascending aorta level of all 3 cohorts ( Figure 1 ). The elastic properties of the aortic root were significantly more deteriorated in the Ross patients than in the other 2 groups ( Table 2 ). These properties showed no gender differences in all 3 cohorts. In all patients, the AV, AoR, and STJ diameters were optimally assessable. Only in 6 patients after the Ross procedure and in 13 after ASO, echocardiographic assessment of the ascending aorta dimensions were suboptimal. After the Ross procedure, 19 patients (83%) had an aortic root z score of ≥2 and 12 (52%) a z score ≥3. Patients with and without a z score of ≥3 had similar elasticity indexes. Of the 52 patients with TGA, 31 (60%) presented with an AoR diameter exceeding the z score limit of +2 and 16 (31%) the z score limit of +3. The age at ASO (15 ± 36 days with z score ≥3 vs 9 ± 11 days with z score <3) were similar, and no differences in elasticity were noted.
| Variable | Control (n = 48) | TGA Switch (n = 52) | Ross Operation (n = 23) | p Value | ||
|---|---|---|---|---|---|---|
| C/T | C/R | T/R | ||||
| Male infants | 26 (54%) | 34 (65%) | 18 (78%) | 0.027 ∗ | 0.002 ∗ | 0.027 ∗ |
| Weight (kg) | 35 ± 20 | 39 ± 23 | 45 ± 26 | 0.217 | 0.109 | 0.345 |
| Height (cm) | 129 ± 38 | 136 ± 32 | 141 ± 37 | 0.328 | 0.209 | 0.564 |
| Body surface area (m 2 ) | 1.1 ± 0.5 | 1.2 ± 0.5 | 1.3 ± 0.6 | 0.216 | 0.09 | 0.391 |
| Age at investigation (yrs) | ||||||
| Mean ± SD | 9.1 ± 5.3 | 10.1 ± 5.5 | 11.3 ± 5.9 | 0.359 | 0.135 | 0.404 |
| Range | 0.1–17.2 | 0.3–17.8 | 0.2–18 | |||
| Age subgroups (yrs) | ||||||
| <5 | 13 (27%) | 11 (21%) | 4 (17%) | |||
| ≥5–10 | 14 (29%) | 16 (31%) | 5 (22%) | |||
| ≥10–15 | 11 (23%) | 9 (17%) | 4 (17%) | |||
| ≥15 | 10 (21%) | 16 (31%) | 10 (44%) | |||
| Age at surgery (yrs) | ||||||
| Mean ± SD | NA | 0.03 ± 0.1 | 7.0 ± 5.0 | <0.001 ∗ | ||
| Range | 0–0.42 | 0.1–16.3 | ||||
| Interval since surgery (yrs) | ||||||
| Mean ± SD | NA | 10.1 ± 5.5 | 4.4 ± 3.6 | <0.001 ∗ | ||
| Range | 0.2–17.8 | 0.1–11.6 | ||||
| Systolic blood pressure (mm Hg) | 103 ± 12 | 109 ± 15 | 114 ± 12 | 0.011 ∗ | <0.001 ∗ | 0.204 |
| Diastolic blood pressure (mm Hg) | 59 ± 8 | 59 ± 7 | 61 ± 7 | 0.986 | 0.244 | 0.167 |
| Variable | Control (n = 48) | TGA Switch (n = 52) | Ross Operation (n = 23) | p Value | ||
|---|---|---|---|---|---|---|
| C/T | C/R | T/R | ||||
| Aortic valve | ||||||
| Diameter (mm) | 16.5 ± 4.4 | 21.8 ± 5.7 | 25.2 ± 7.4 | <0.001 ∗ | <0.001 ∗ | 0.031 ∗ |
| z Score | 0.47 ± 1.14 | 2.64 ± 1.24 | 3.68 ± 1.26 | <0.001 ∗ | <0.001 ∗ | 0.001 ∗ |
| Aortic root | ||||||
| Diameter (mm) | 20.9 ± 5.6 | 27.6 ± 7.6 | 32.1 ± 9.9 | <0.001 ∗ | <0.001 ∗ | 0.034 ∗ |
| z Score | −0.04 ± 1.15 | 2.33 ± 1.30 | 3.24 ± 1.37 | <0.001 ∗ | <0.001 ∗ | 0.006 ∗ |
| Sinutubular junction | ||||||
| Diameter (mm) | 16.9 ± 4.7 | 23.7 ± 7.5 | 26.9 ± 9.2 | <0.001 ∗ | <0.001 ∗ | 0.158 |
| z Score | −0.12 ± 1.15 | 2.41 ± 1.65 | 3.21 ± 1.74 | <0.001 ∗ | <0.001 ∗ | 0.065 |
| Ascending aorta | ||||||
| Diameter (mm) | 17.04 ± 4.5 | 22.34 ± 7.4 | 23.5 ± 7.8 | <0.001 ∗ | 0.120 | 0.614 |
| z Score | −0.90 ± 1.21 | 1.33 ± 2.17 | 1.67 ± 1.92 | <0.001 ∗ | 0.096 | 0.417 |
| Stiffness | 3.32 ± 0.86 | 4.99 ± 2.30 | 7.54 ±3.77 | <0.001 ∗ | <0.001 ∗ | 0.001 ∗ |
| Distensibility (cm 2 ∙ dynes −1 × 10 −6 ) | 8.21 ± 2.03 | 6.33 ± 3.56 | 3.91 ± 1.80 | 0.002 ∗ | <0.001 ∗ | 0.003 ∗ |
| Distensibility (kPa −1 × 10 −3 ) | 66.8 ± 18.2 | 51.8 ± 31.4 | 31.0 ± 14.7 | 0.004 ∗ | <0.001 ∗ | 0.003 ∗ |
Neoaortic regurgitation exceeding the limit of trace was recorded in 3 patients with TGA, who were slightly younger at ASO (age 4.3 ± 3.8 days) than those without aortic regurgitation (age 11.2 ± 22.8 days). A significantly elevated AV z score, but not a significantly different STJ z score, was noted in those 3 patients. The elastic properties were equal in both groups. A total of 6 patients with TGA presented with a concomitant ventricular septal defect (12%, 3 female infants and 3 male infants) that was closed, together with the ASO. These procedures were performed significantly later in life at a mean of 41.3 ± 58.8 compared to 6.8 ± 6.0 days of age in patients without a ventricular septal defect (p <0.001). However, no differences in the aortic z scores or elasticity indexes were found.
Of the 23 Ross patients, 21 originally experienced congenital aortic valve stenosis, 1 congenital and 1 acquired aortic valve regurgitation (rheumatic fever). No correlation of aortic valve dysfunction with the aortic root z score or with aortic root elasticity was found. The underlying phenotype of the native aortic valves was bicuspid in 13 and tricuspid in 8; in 2, the phenotype was indistinguishable. The aortic dimensions and aortic elasticity values did not differ between the 2 phenotypes. Also, the age at Ross operation was comparable. All 21 patients with aortic stenosis had undergone previous interventions: balloon valvuloplasty in 8 (1 with an intrauterine approach) followed by surgical valvulotomy in 2; primary valvulotomy in 12, followed by aortic valve reconstruction in 4; and aortic homograft implantation in 1. A Ross-Konno procedure was performed in 2 patients; another 4 had undergone earlier or simultaneous correction of an aortic coarctation. The mean age at the Ross operation was 83.5 ± 60 months (6.9 ± 5 years; range 0.8 months to 16.3 years). The procedure was performed in 2 patients neonatally; in 6 at 4 weeks to 5 years of age, in 9 at 5–10 years, in 3 at 10–15 years, and in 3, after the age of 15 years. The age at surgery neither influenced the aortic z scores nor the elasticity levels significantly. The follow-up time after Ross procedure was <1 year in 6 patients, 1–5 years in 6, and >5 years in 11 children and adolescents. No failure of the neoaortic valve with a regurgitation exceeding the degree of trace occurred until now. No significant influence of the follow-up duration on the diameter or elasticity indexes was observed.
In the subdivided age groups, a nearly constant increase of the 4 diameters during somatic growth in the control group and to a statistically significant greater degree in patients with TGA was found. The z scores of the AV, AoR, and, inconstantly, the STJ had increased to greater than the normal limits of a z score of +2 in the patients with TGA at the age of 5 years and of the ascending aorta at the age of 15 years. At older ages, significantly worse elasticity indexes were noted in the TGA subgroups than in the controls, exceeding the upper limit of normal at about 10 years of age. In contrast, the elasticity values stayed constantly normal without increases during adolescence in the control group. The aortic dimensions after Ross procedure increased more than proportionally during somatic growth; therefore, matching age subgroups revealed statistically larger diameters of the AV, AoR, and STJ in the Ross subpopulation ( Figure 2 ). The mean AV and AoR diameters were constantly greater than z scores of +2 and even greater than +3 in AV, AoR, and STJ after the age of 5–10 years. Significantly stiffer and less distensible elasticity indexes were found, reaching pathologic levels after the age of 5 years. A subanalysis of the patient age subgroups showed that the elasticity indexes in the Ross patients worsened around 5 years earlier than in patients with TGA, regardless of age at Ross operation ( Figure 3 ).