Patients with hypertrophic cardiomyopathy (HC) can experience exacerbation of exertional symptoms after a meal. The present study was designed to determine the prevalence and clinical correlates of postprandial symptom exacerbation (PPSE) in patients with HC. The records of 558 patients with HC and PPSE data who had undergone echocardiography at our institution from 2002 to 2006 were reviewed. Continuous-wave Doppler velocities were used to determine the left ventricular outflow tract gradient. Left ventricular filling was assessed using transmitral velocity curves. The Minnesota Living With Heart Failure questionnaire was administered to measure symptom limitations. A multivariate regression model was developed to determine the independent correlates with PPSE. Of the 558 patients whose records were reviewed, 189 (33.8%) had PPSE. The patients with PPSE were more likely to experience New York Heart Association class III/IV dyspnea or presyncope. PPSE was associated with greater resting outflow gradients and lower perceived quality of life. In conclusion, patients presenting with severe postprandial symptoms and reduced quality of life should be carefully evaluated for the presence of dynamic left ventricular outflow tract obstruction.
It has been recognized that patients with hypertrophic cardiomyopathy (HC) can experience exacerbation of cardiac symptoms after a meal. Previous studies of relatively small patient populations have estimated that approximately 1/3 of patients with HC experience this phenomenon. The hemodynamic effects of a meal have been well documented for producing an arterial vasodilation with afterload reduction and a compensatory increase in heart rate. These changes, directly and indirectly, lead to worsening of left ventricular (LV) outflow tract obstruction and elevation of diastolic filling pressures. However, the postprandial response in patients with HC has been difficult to demonstrate, and the clinical implications of postprandial symptom exacerbation (PPSE) remain unclear. If PPSE implies labile obstruction to outflow, the clinical recognition of its presence would warrant consideration in diagnostic and therapeutic decision making. The aims of the present study were to determine the prevalence of PPSE in a large population of patients with HC, to determine the clinical correlates with PPSE that relate to disease severity, and to assess the effect of PPSE on quality of life (QOL) in patients with HC.
Methods
The Mayo Clinic Institutional Review Board approved the study. The Mayo Clinic Department of Cardiovascular Disease has maintained a database of the clinical characteristics of all patients with HC evaluated at the clinic since 1959. The study was limited to all patients evaluated from 2002 to 2006 because tissue Doppler imaging had been phased in as a part of the standard echocardiographic evaluation at our institution in late 2001. All subjects for whom the symptomatic response to a meal was known were included. A graphic representation of the study population is shown in Figure 1 .
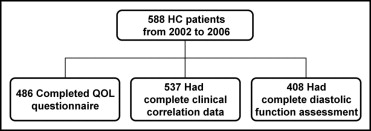
The clinical data for patients with HC were obtained from the Mayo Clinic HC database for the selected study period. The prevalence of PPSE was computed from all patients for whom the postprandial symptomatic response was known. Complete data for the analysis of clinical correlates with PPSE were available for a large subset of patients. The echocardiographic parameters included structural measurements and the resting LV outflow tract gradients derived from the continuous-wave Doppler velocities. A baseline comparison of the clinical and echocardiographic features of the study population was completed. Variables exhibiting a statistically significant difference on univariate analysis were entered into a logistic regression model to determine their independent association with PPSE.
An assessment of LV filling was made from an analysis of the transmitral velocity profiles using the ratio of early transmitral flow velocity (E) to medial mitral annular tissue velocity (e′). The nominal E/e′ value was compared between the PPSE-positive group and the PPSE-negative group, as was an E/e′ value >15, which has previously been correlated with elevated mean LV filling pressures.
The Minnesota Living With Heart Failure questionnaire was administered to provide an objective measurement of the patients’ QOL. All patients who completed the questionnaire were included. The questionnaire includes a series of 20 statements related to cardiac-specific symptom limitation and has been previously validated. The scores from the individual statements were summed to achieve a total QOL score with a range from 0 to 100, with lower scores indicating less symptom limitation (ie, better QOL). The scores from the completed questionnaires were compared between the PPSE-positive group and the PPSE-negative group to assess the effect of PPSE on QOL.
All continuous variables were tested for normality of distribution. Ventricular septal thickness and resting LV outflow tract gradient data were normalized with a logarithmic transformation. The 2-tailed t test, Wilcoxon rank sum test, and Kruskal-Wallis test were used, as appropriate. Nominal data were analyzed using the 2-tailed Fisher exact test. A linear regression model was developed to determine the independent correlates with PPSE. A correlation coefficient was determined, and p values were calculated. The results are reported as the mean ± SD, with 95% confidence intervals. Statistical significance was set, a priori, at p <0.05.
Results
Of the 558 patients included in the present study, 189 (33.8%) reported PPSE. The clinical characteristics of a subset of 537 patients evaluated for clinical correlates with PPSE are summarized in Table 1 . The results of the baseline comparison indicated that patients with PPSE were more likely to have New York Heart Association class III/IV dyspnea or presyncope, greater septal thickness, and greater resting LV outflow tract gradients.
| Characteristic | PPSE | p Value | |
|---|---|---|---|
| Yes (n = 182) | No (n = 355) | ||
| Mean age (years) | 52 ± 15 | 50 ± 18 | 0.37 |
| Men | 115 (63%) | 203 (57%) | 0.20 |
| Family history of sudden cardiac death | 33 (18%) | 68 (19%) | 0.82 |
| Angina, New York Heart Association class III/IV | 18 (10%) | 25 (7%) | 0.25 |
| Dyspnea, New York Heart Association class III/IV | 119 (65%) | 124 (35%) | <0.001 |
| Presyncope | 130 (71%) | 148 (42%) | <0.001 |
| Syncope | 39 (21%) | 71 (20%) | 0.74 |
| Atrial fibrillation | 31 (17%) | 57 (16%) | 0.81 |
| Hypertension | 76 (42%) | 127 (36%) | 0.19 |
| Coronary artery disease | 26 (14%) | 41 (12%) | 0.41 |
| Diabetes mellitus | 12 (7%) | 17 (5%) | 0.42 |
| Mean ventricular septal thickness (mm) | 21.6 ± 8.5 | 20.4 ± 6.2 | 0.04 |
| Ventricular septal thickness >30 mm | 14 (8%) | 25 (7%) | 0.86 |
| Left ventricular outflow tract gradient at rest (mm Hg) | <0.01 | ||
| Mean | 48.7 | 37.1 | |
| 95% Confidence interval | 43.0–54.5 | 32.7–41.5 | |
| Obstruction at rest (left ventricular outflow tract or mid-ventricular) | 121 (66%) | 181 (51%) | <0.001 |
| Left ventricular outflow tract gradient >30 mm Hg at rest | 119 (65%) | 166 (47%) | <0.001 |
| Mid-ventricular obstruction | 2 (1%) | 15 (4%) | 0.07 |
| Left ventricular outflow tract gradient >30 mm Hg with provocation only | 36 (20%) | 72 (20%) | 0.91 |
| Nonobstructive | 25 (14%) | 102 (29%) | <0.001 |
| Pacemaker | 25 (14%) | 70 (20%) | 0.10 |
| Implantable cardioverter-defibrillator | 26 (14%) | 65 (18%) | 0.28 |
| Myectomy | 61 (34%) | 113 (32%) | 0.70 |
| Septal ablation | 29 (16%) | 35 (10%) | 0.05 |
| Medications | |||
| β Blocker | 129 (71%) | 230 (65%) | 0.18 |
| Calcium channel blocker | 53 (29%) | 99 (28%) | 0.76 |
| Disopyramide | 14 (8%) | 18 (5%) | 0.25 |
A logistic regression model was developed with the variables of statistical significance from the baseline comparison to assess their independent association with PPSE. The results of the regression model ( Table 2 ) showed that patients with PPSE were more likely to have advanced dyspnea (p <0.001) or presyncope (p <0.001) and resting LV outflow tract gradients >30 mm Hg (p = 0.02).



